* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download formulation and in vitro evaluation of bilayered buccal patches of a
Discovery and development of neuraminidase inhibitors wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Tablet (pharmacy) wikipedia , lookup
Compounding wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Drug discovery wikipedia , lookup
Nicholas A. Peppas wikipedia , lookup
Neuropharmacology wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug interaction wikipedia , lookup
Drug design wikipedia , lookup
Theralizumab wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
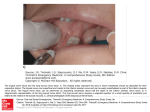
FORMULATION AND IN VITRO EVALUATION OF BILAYERED BUCCAL PATCHES OF A PROTON PUMP INHIBITOR a) BRIEF RESUME OF THE INTENDED WORK NEED FOR THE STUDY: Proton pump Inhibitors (PPIs) exhibit potent and long-lasting inhibition of gastric acid secretion by selectively interacting with the gastric proton pump (K+ /H+ -ATPase) in the parietal cell secretory membrane. However, the bioavailability of proton pump inhibitors following oral administration is usually very low, since they degrade very rapidly in the acidic environment of stomach and undergo hepatic first pass metabolism. To improve the bioavailability of Proton pump Inhibitors, in particular by preventing gastric degradation, various oral formulations of Proton pump Inhibitors such as enteric coated granules and tablets have been developed1. PPIs are better antisecretory agents than H2 receptor antagonists (H2-RAs) 2, 3. In this study, an attempt will be made to develop a PPI buccal adhesive patch to avoid gastric degradation and first-pass metabolism in the liver. Absorption of drug from the buccal mucosa and attachment of the patch with buccal mucosa without collapse are the two prime considerations in the design of a conventional buccal adhesive patch .However, an additional consideration in the case of PPI’s is the stability of PPI’s in human saliva, since it is very unstable in acidic media4. Moreover, it has been reported that a controlled release of the drug, over an extended period of time can be secured by using various combination of polymers in a bilayered buccal adhesive patch5. Hence, various formulations of a buccal adhesive patch of a PPI with bioadhesive polymers and stabilizers, that may fulfill the above requirements, will be investigated. Advantages of Buccal Patches:1. Rapidity of Action6. 2. Medications administered buccally bypass the first pass metabolism6. 3. Medications administered buccally directly enter systemic circulation without undergoing gastrointestinal degradation6. 4. Buccal mucosa provides efficient blood supply and has relatively low enzymatic activity7. 5. Moreover, the buccal mucosa is easily accessible and acceptable to patients; it allows the patient to interrupt drug administration by simply removing the drug delivery system7. Hence, the present work is an attempt to formulate a bilayered mucoadhesive buccal patch, containing proton pump inhibitor for inhibiting gastric acid secretion, bypassing the first pass metabolism and to ensure better patient compliance. 6.2 REVIEW OF LITERATURE Mucoadhesive buccal films of Ranitidine were formulated and evaluated by solvent casting technique using polymers like hydroxy propyl methyl cellulose-15 cps and poly vinyl pyrrolidone. The formulations of Ranitidine bioadhesive buccal were reported to give controlled drug delivery, improve bioavailability and the dose of ranitidine could be minimized by preventing the colonic degradation of ranitidine by colonic bacteria8. Chitosan based sustain release mucoadhesive buccal patches containing verapamil hydrochloride were formulated and evaluated using different ratios of chitosan and polyvinylpyrrolidone (PVP K-30). It was concluded that Chitosan with PVP K-30 can meet the ideal requirement for buccal devices, which can be good way to bypass the extensive hepatic first pass metabolism and increase bioavailability9. Mucoadhesive buccal patch of carvedilol formulated and evaluated by using two different mucoadhesive polymers. Good results were obtained both in vitro and in vivo conditions for films of HPMC E15 LV. It was concluded that development of bioadhesive buccal formulation for carvedilol may be a promising one as the dose of carvedilol may be decreased and hence side effects may be reduced10. Mucoadhesive buccal patch of Propranolol hydrochloride formulated and evaluated by using different ratios of chitosan and polyvinylpyrrolidone (PVP K-30). Finally it was concluded that the optimized buccoadhesive patches of propranolol hydrochloride with the combination of chitosan and PVP K-30 can meet the ideal requirements for buccal devices, which can be a good way to bypass the extensive hepatic first pass metabolism11. Buccal adhesive tablets of Omeprazole formulated and evaluated by using sodium alginate and hydroxypropylmethylcellulose (HPMC). The results suggest that the oral buccal adhesive tablet would be useful to deliver omeprazole1. Carvedilol(CAR) buccal tablets using Methyl-β-cyclodextrin (CAR-MβCD) complex ,Carbopol 974P, sodium carboxymethylcellulose, lactose, PVPK30, talc and magnesium stearate were formulated and evaluated for drug release, mucoadhesive strength and exvivo permeability. It was concluded that buccal tablet containing complexed CAR would have improvement in bioavailability12. Results from numerous comparative clinical trials and meta-analyses of these studies have shown that Proton pump inhibitors (PPIs) are significantly more effective than H2 receptor antagonists for suppressing gastric acid secretion and healing duodenal and gastric ulcers and erosive oesophagitis, and for the relief of acid-related symptoms. PPIs are also significantly more effective than H2RAs or misoprostol for preventing and healing NSAID-associated ulcer disease13. It was concluded that the buccal mucosa was a promising delivery route for drugs that need to avoid the gastrointestinal tract due to degradation by the gastric pH, intestinal enzymes, or due to a substantial hepatic first pass effect. It can also be an alternative to skin, pulmonary, or nasal delivery. The physiology of the buccal mucosa allows for the penetration of active substances and due to its rapid cellular turnover and recovery, the use of penetration enhancers is possible14. Buccal patches of famotidine were formulated and evaluated by using Hydroxypropylmethylcellulose, Sodium carboxymethylcellulose, and polyvinyl alcohol by using solvent casting method. The study successfully demonstrated that buccal patches of famotidine reduced the dose and thereby decreased side effects15. Mucoadhesive bilayered buccal devices comprising of a drug containing mucoadhesive layer and drug free backing membrane were successfully formulated and evaluated , using mixture of drug (methotrexate) and sodium alginate alone or in combination with sodium carboxy methyl cellulose, polyvinyl pyrollidine and carbopol 934 and backing membrane(ethyl cellulose) by solvent casting technique5. Bilayered buccal pacthes of felodipine were formulated and evaluated using hydroxyl propyl methyl cellulose as primary layer and Eudragit RLPO as secondary layer by solvent casting technique The results indicated that suitable bilayered buccoadhesive patches with desired permeability could be prepared16. A new validated, simple, rapid and reliable UV Spectrophotometry method for the estimation of Omeprazole in blend & capsules formulations was reported 17. 6.3 OBJECTIVES OF THE STUDY The present research work is an attempt to formulate a bilayered mucoadhesive dosage form of PPIs by varying possible formulation variables and evaluation by process of optimization. This research work is an attempt to 1. Formulate a bilayered mucoadhesive dosage form containing a PPI. 2. Evaluation for the following i. Film weight and thickness. ii. Surface pH of the patches. b) iii. Folding endurance. iv. Tensile strength of the patches, v. Drug Content Uniformity of patches. vi. In Vitro Release Studies of PPI patches. vii. In Vitro Bioadhesive Test. viii. Percentage moisture absorption.(PMA)test. ix. Percentage moisture loss.(PML)test. x. Swelling percentage.(%S)test. MATERIALS AND METHODS 7.1 SOURCE OF DATA: Data on drugs and dosage forms will be collected from Drug Information Center, standard books, physicochemical database and literature search from Scientific journals and related articles. Internet facilities. Krupanidhi College of pharmacy library. Publication and Journals of Pharmacy. 7.2 METHOD OF COLLECTION OF DATA: The data on physicochemical and pharmacokinetic properties of the drug will be collected from drug information center, various standard Books, journals, websites and other sources like research literature databases such as Medline, Science Direct etc. The experimental data will be collected from study of the drug; its formulation, through investigation of the process and product variables in the laboratory of Krupanidhi College of Pharmacy, Bangalore-35. c) REFERENCES 1. Han GC, Hee JJ, Soon CY, Dal CR, Kyung ML, Hee JH, et al. Formulation and in vivo evaluation of Omeprazole buccal adhesive tablet. J Control Release 2000; 68:405-12. 2. Colin-Jones DG. The role and limitations of H2-receptor antagonists in the treatment of gastro-oesophageal reflux disease. Aliment Pharmacol Ther 1995; 9(Suppl. 1):9–14. 3. Scarpignato C, Bruley des Varannnes S. Traitment médical du RGO parles antagonistes des récepteurs H2 de l’histamine. Gastroenterol Clin Biol 1999; 23:S78–89. 4. Han GC, Chong KK. Development of omeprazole buccal adhesive tablets with stability enhancement in human saliva. J Control Release 2000; 68:397-404. 5. Reddy CP, Ramesh G, Vishnu VY, Kumar S, Rao MY. Development of bilayered mucoadhesive patches for buccal delivery of felodipine: in vitro and ex vivo characterization. Curr trend Biotech Pharm 2010; 4:1-10. 6. Cassidy J, Berner B, Chan K, John V, Toon S, Holt B, et al. Human Transbuccal Absorption of Diclofenac Sodium from a Prototype Hydrogel Delivery Device. Pharm Res 1993; 10(1):126-129. 7. Rossi S, Sandri G, Caramella C.Buccal Delivery Systems for Peptides: Recent Advances. Healthcare Technology Review. Am J Drug Del 2005; 3(4):215-225. 8. Alagusundaram M, Chengaiah B, Ramkanth S, Parameswari SA, Chetty MSC, Dhachinamoorthi D. Formulation and evaluation of mucoadhesive buccal films of Ranitidine. Int J Pharmtech Res 2009; 1(3):557-563. 9. Subash VD, Madhuri AC, Anil VC, Joshi UM, Kailash RB.Chitosan based sustain release mucoadhesive buccal patches containing verapamil HCL. Int J Pharm Pharm Sci 2009; 1(1):1-14. 10. Vishnu VY, Chandrasekhar K, Ramesh G Rao MY. Development of mucoadhesive patches for buccal administration of Carvedilol. Curr Drug Del 2007; 4: 27-39. 11. Vishnu MP, Bhupendra GP, Madhabhai MP. Design and characterization of chitosan containing mucoadhesive buccal patches of propranolol hydrochloride. Acta Pharm 2007; 57:61-72. 12. Hirlekar RS, Kadam VJ.Design of buccal drug delivery system for a poorly soluble drug. Asian J Pharm Clin Res 2009; 2(3):1-5. 13. Hauang JQ, Richard HH. Pharmacological and pharmacodynamic essentials of receptor antagonists and proton pump inhibitors for the practising physicians, Best Practice and Research. Clin Gastroenterol 2001; 15(3):335-370. 14. Javier OM, Jason TMC. Manufacture and characterization of mucoadhesive buccal films. Eur J Pharm Biopharm 2011; 77:187-199. 15. Kumar M, Garg G, Kumar P, Kulakarni GT, Kumar A. Design in vitro evaluation of mucoadhesive buccal films containing Famotidine. Int J Pharm Pharm Sci 2010; 2(3):1-5. 16. Bhanja S, Ellaiah P, Choudhury R, Murthy KVR, Bibhutibhusan P Kumar SM. Design and evaluation of methotrexate buccal mucoadhesive patches. Int J Pharm Biomed Sci 2010; 1(2): 31-36. 17. Kumaraswamy D, Thinaraj SB, Rajveer CH, Sudarshini S, Shrestha B, Rao RSP. Process validation of analytical method development and validation for Omeprazole capsules and blend. Int J Pharm Biomed Sci 2010; 1(2):1-6.