* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter 38
Survey
Document related concepts
Transcript
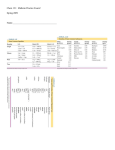
Chapter 38 Hypertension Hypertension/High Blood Pressure • Persistent SBP >= 140 mmHg • Persistent DBP >= 90 mmHg • “the silent killer” • Higher prevalence in African Americans • Risk factors: obesity, family history Classification & Risks Risk Group A Risk Group B Risk Group C No major risk factors 1+ risk factors (not including diabetes) May or may not have risk factors No target organ damage No target organ damage Target organ damage No clinical cardiovascular disease No clinical cardiovascular disease Clinical cardiovascular disease or diabetes Classification Systolic (SBP) Diastolic (DBP) Normal 90-119 mmHg 60-79 mmHg Pre-hypertensive 120-139 mmHg 80-89 mmHg Stage 1 140-159 mmHg 90-99 mmHg Stage 2 >= 160 mmHg >= 100 mmHg Classification • Primary (essential): identifiable factors (increased sodium, obesity, diabetes, excessive alcohol) • Secondary: caused by an underlying condition (kidney disease, pregnancy, arterial conditions) Blood Pressure Factors BP = CO x PVR • Blood pressure = cardiac output X peripheral vascular resistance • Cardiac output: volume of blood pumped by the heart in 1 minute • PVR: force in the blood vessels that the LV must overcome to eject blood from the heart ▫ Diameter of blood vessels ▫ Blood viscosity ▫ PVR increased when arteries or arterioles are narrow or there is increased fluid volume Age-Related Changes • Reduced elasticity of arteries • Decreased cardiac output, increased PVR • Decreased ability of aorta to stretch Primary (Essential) Hypertension • Risk Factors: dyslipidemia, atherosclerosis, diabetes, tobacco use, 55+ men or 65+ women, family history, sedentary lifestyle, obesity, stress • S/S: no symptoms; headaches; lightheadedness; epistaxis; impaired organ function • Complications: heart attack, heart failure, stroke, kidney disease, blindness, organ damage ▫ Heart: CHD can cause angina, MI, or CHF; the LV has to work harder, leading to hypertrophy & failure ▫ Kidneys: renal arteries narrow, decreasing renal function & leading to renal failure; nocturia, azotemia, proteinuria, & hematuria may indicate failure ▫ Brain: cerebral arteries constrict & are damaged, leading to risk for TIAs & CVAs ▫ Eyes: narrowing of retinal arterioles, retinal hemorrhage, or papilledema can lead to blindness Diagnostic Tests & Procedures • At home monitoring (ambulatory) • Lifestyle data, cardiovascular risks, medical diagnoses • Lab studies • EKG • Chest radiograph Treatment • Gradually reduce PVR & BP to less than 140/90 mmHg • Goal 130/80 mmHg if they have diabetes or renal disease • Optimal BP is less than 120/80 mmHg • Treat underlying condition if secondary • Nonpharmacologic tx first • Drug therapy, if needed Treatment: Lifestyle Modifications • • • • • Weight reduction Smoking cessation Sodium/alcohol restriction Exercise program Relaxation Treatment: Pharmacologic Therapy • • • • • Indicated for 160/100 or greater Individualized treatment With diurectics, monitor fluids & electrolytes Monitor s/s hypokalemia Irritability,confusion pg775 Treatment: Pharmacologic Therapy 1. Centrally Acting Agents (Alpha2-Agonists) 1. Reduces peripheral resistance & lowers BP 2. Alpha-Adrenergic Receptor Blockers (Antagonist) 1. 2. Reduces peripheral resistance SE: orthostatic hypotension (lie down for 2 hours after taking first or increased dose); dizziness, headache, drowsiness 3. Beta-Adrenergic Receptor Blockers (Beta Blockers) 1. 2. 3. Lower HR; decrease cardiac constriction Do not use in patients with asthma, COPD, or heart blocks Monitor for bradycardia, hypotension, & hypoglycemia 4. Direct Vasodilators 1. 2. Relaxes arteriolar smooth muscle Sometimes used for emergency situations via IV fluids Treatment: Pharmacologic Therapy 1. Calcium Channel Blockers (Calcium Antagonists) 1. 2. Reduces HR, reduces cardiac contraction, dilates peripheral arteries SE: flushing, dizziness, headache, hypotension, bradycardia, edema 2. Angiotensin-Converting Enzyme Inhibitors (ACE) 1. 2. Decreased peripheral resistance, decreased fluid retention SE: chronic cough, dizziness, headache, fatigue, angioedema, hyperkalemia, hypotension 3. Diuretics 1. 2. Monitor for fluid/electrolyte imbalance; I/O; Signs of hypokalemia (especially in geriatrics) Potassium replacement, if needed 4. Angiotensin II Receptor Antagonists 1. 2. Prevent vasoconstriction, reduces blood volume SE: dizziness Treatment: Nursing Implications 1. 2. 3. 4. Be familiar with the drugs & side effects Monitor the patient Teach about their drug regimen & disease process Carefully monitor geriatric patients due to reduce liver/kidney functions & risk for orthostatic hypotension (risk for falls) Secondary Hypertension • Causes: renal disease, excess secretion of adrenal hormones, narrowed aorta, increased intracranial pressure, some drugs Nursing Assessment • Health History: previous hypertension; renal, cardiac, or endocrine disorders; previous BP measurements; pregnancy/hormone replacement therapy; all medications/OTC/herbal remedies; family history; review of systems for symptoms (headache, epistaxis, dizziness, dyspnea, angina, nocturia); occupational history, activity levels; sleep/rest/stress; nutrition • Physical Exam: general appearance; signs of distress; height/weight/VS; BP in both arms, if possible; RR rate & effort; extremities (edema/color); reassess BP 1-5 minutes later; notify MD immediately if DBP > 115 mmHg (risk for stroke!) Pg778-779 Secondary Hypertension: Interventions • Ineffective Self-Health Management: educate on therapy adherence and disease process; listen & address concerns; include family or support system; teach about medications & at-home monitoring; educate on diet therapy, including weight loss & low-sodium diet ▫ Exercise: educate; encourage; start a program; discuss with physicians; motivate ▫ Stress Management: identify stressors; discuss stress reduction strategies; refer to counselor if needed ▫ Drug Therapy: educate about medications, timing, purpose, side effects; advise not to stop or change drug therapies without talking to their doctor; discuss OTC therapies that can cause high blood pressure ▫ DASH Diet (Dietary Approaches to Stop Hypertension) 2000 calories a day 7-8 servings of grains/grain products 4-5 servings of vegetables 4-5 servings of fruits 2-3 servings of low-fat or fat-free dairy 2 or less lean meats, poultry, fish 4-5 per week of nuts, seeds, dry beans 2-3 fats & oils 5 per week of sweets Secondary Hypertension: Interventions • Risk for Injury: due to drug side effects; educate & monitor ▫ Orthostatic Hypotension: sudden drop in SBP (20 mmHg) when going from lying/sitting to standing position; monitor for syncope, lightheadedness, dizziness; encourage leg exercises & to rise slowly ▫ Sedation: take meds at nighttime (if ordered) to promote sleep; if unavoidable, do not do activities (driving) during peak drug times • Ineffective Coping: depression (drug side effect), consult MD; refer if needed • Sexual Dysfunction: (Rx side effect); ask about sexual abilities if patient does not offer this information; advise MD Older Patients • • • • Monitor drug therapy response Watch for orthostatic hypotension & sedation Monitor & assess for depression Never assume they are not sexually active pg782 Hypertensive Crisis • Life-threatening medical emergency! Death can occur! • S/S: severe headache, blurred vision, nausea, restlessness, confusion, Elevated DBP (130 mmHg or more); tachycardia, tachypnea • “Malignant hypertension:” type of hypertensive crisis with DBP > 140 mmHg; sudden onset; usually African-Americans aged 30-40. • Diagnosis: elevated BP, HR, RR; retinal hemorrhage; papilledema; labs & chest radiograph; direct BP monitoring through arterial catheter • Treatment: rapidly reduce BP to nonlife-threatening level, then slowly to normal range; diuretics & potent vasodilators THIS CAN HAPPEN IF A PATIENT ABRUPTLY STOPS THEIR HTN MEDICATIONS! EDUCATE TO NEVER STOP TAKING THEIR MEDS WITHOUT TALKING TO THEIR DOCTOR FIRST!!! Hypertensive Crisis Nursing Care • Assessment: monitor closely, frequently check VS; record I/O; watch for N/V (early signs of seizure or coma) • Interventions: administer drugs; monitor VS; monitor cardiac/renal function; continue IV therapy & oxygen; comfort patient; ensure safety if possible seizure activity (raise/pad side rails, elevate HOB, ensure oral airway & suction equipment is available); encourage & educate patient Questions?