* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download File
Survey
Document related concepts
Transcript
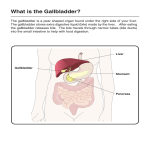
Option D Human Physiology D. 3 Functions of the Liver D.3 Essential idea: The chemical composition of the blood is regulated by the liver Nature of science: Educating the public on scientific claims – scientific studies have shown that highdensity lipoprotein could be considered “good” cholesterol. Application: Dual blood supply to the liver and differences between sinusoids and capillaries Blood arrives at the liver from two sources: o Hepatic artery branches off aorta bringing oxygen-rich blood from heart o Hepatic portal vein brings blood from stomach and intestines, most blood circulating comes from this vein, blood is rich in nutrients that have been absorbed, oxygen content low. The vein subdivides inside liver into divisions called sinosoids. These are capillaries but are wider and walls are not continuously lined with cells. This allows blood to come in contact with hepatocytes (liver cells) and allows proteins to enter and leave the blood. Hepatic artery subdivides into arterioles, which join with sinusoids providing oxygenated blood. The sinusoids merge with venules that lead to hepatic vein, and this caries blood from liver to vena cava. Diagrams of circulation within the liver Notice: Off the Aorta (brings blood from heart) comes the hepatic artery. Attached the vena cava (takes blood to heart) is the hepatic vein. Notice: Kupffer cells Bile duct is taking stuff away. D.3 U7 The liver intercepts blood form the gut to regulate nutrient levels. One main function of liver is to regulate quantity of nutrients circulating in the blood. Key role in glucose, it can store glucose as glycogen or break down glycogen to glucose. Body can’t store proteins or amino acids, excess quantities in diet are broken down in liver to be utilized as energy sources. Waste product produced is nitrogenous waste. Liver also manages circulating lipids. Lipids come in many forms: Chylomicrons arrive from intestines and need to be broken down. Very low density lipoproteins (VLDL) are synthesized by hepatocytes which transport the triglycerides synthesized in liver into blood plasma for storage and use. Cholesterol in surplus is converted into bile salts. D.3 U8 Some nutrients in excess can be stored in the liver. If glucose level is high, insulin is released and stimulates hepatocytes to take up glucose and store it as glycogen. When levels fall, hormones such as glucagen is released and result is breakdown of glycogen, glycerol, amino acids and fatty acids in liver releasing glucose to the blood stream. Iron, retinol (vitamin A) and calciferol (vitamin D) are stored in liver when in excess and released if deficit D.3 U2 Components of red blood cells are recycled by the liver. Lifespan of erythrocyte (RBC) in an adult is 120 days. Old and damaged RBC’s undergo changes in plasma membrane which makes them susceptible to recognition by macrophages. RBC’s are removed form circulation and broken down in the spleen and liver. Liver breakdowns erythrocytes and hemoglobin and most products are recycled. D.3 U3 The breakdown of erythrocytes starts with phagocytosis of red blood cells by Kupffer cells. As RBC’s age they swell and are engulfed by macrophage Kupffer cells that line sinusoids in liver (see earlier picture) Inside Kupffer cell, hemoglobin is spit into globin chains and a heme group. Amino acids from globin chains are recycled, while heme group is broken down into iron and bilirubin. The Kupffer cells release bilirubin to blood. Iron is transferrin and transported to liver and spleen for storage, or to bone marrow to be used to make new RBC’s. D.3 U4 Iron is carried to the bone marrow to produce hemoglobin in new red blood cells. Hemoglobin is made in RBC’s where iron is added to the heme group. Iron is essential for RBC function as it is part of hemoglobin molecule but it is toxic in high concentrations. When iron is absorbed from intestine or released during recycling of damaged RBC’s it is transferred in the blood bound to a protein called transferrin. Cells have receptors for this transferrin molecule. RBC’s are formed form stem cells in bone marrow. Developing RBC’s have high levels of transferrin receptors. Once bond the receptor-iron complex enters the cell and iron is incorporated into the heme molecule or transferred to a storage molecule called ferritin. Application: Causes and consequences of jaundice. When RBC’s are broken down in liver and spleen, hemoglobin is released. Macrophages digest it and release heme a globin. Globin is digested into amino acids which are recycles. The heme group is converted to iron and a yellow pigment called bilirubin. Bilirubin is also released from breakdown of other proteins such as myoglobin an cytochrome. And bilirubin made outside liver is moved to liver and bound to protein albumin. Bilibubin is insoluble so in liver it is reacted with glucuronic acid to make it soluble. This water soluble form is secreted into canaliculi along with water, electrolytes, bicarbonate, cholesterol, phospholipids, and salts. This mixture is called bile. Hepatocytes secrete a green-brown fluid called bile. Bile is drained away from liver through network of bile canaliculi toward gallbladder. After a meal, bile is expelled form gall-bladder into duodenum of small intestines and plays a role in breakdown and digestion of fatty compounds. If normal metabolism or excretion of bilifubin occurs, like a disease, it can build up in blood. Result is jaundice or yellowing of eyes and skin. Normal concentration in blood plasms is 1.2 mg dl-1. Higher than 2.5 mg dl-1 results in jaundice. Jaundice is seen in liver diseases such as hepatitis or liver cancer. Can occur due to obstruction of bile duct by gallstones or pancreatic cancer. Jaundice in newborns is common and caused by high turnover or RBC’s, liver is still developing, or not feeding properly. Treatment includes exposure to ultraviolet light or sun because it converts excess bilirubin into products that can be excreted. If exposed to high levels for extended time can cause neurological damage called kernicterus and results in deafness and cerebral palsy. Adults usually experience itchiness. D.3 U5 Surplus cholesterol is converted to bile salts. Cholesterol is absorbed from food in the intestine, a large quantities is made by hepatocytes (liver cells). It is a raw material needed for making vitamin D and steroid hormones. It is also part of structural component of membranes and used in making bile. Liver regulates amount of circulating lipids like cholesterol and lipoproteins. It can make them if needed or break them down and secreting it into bile. The amount of cholesterol made by body varies with diet. Excess saturated fat increases the production of cholesterol. D.3 U6 Endoplasmic reticulum and Golgi apparatus in hepatocytes produce plasma proteins. The rough ER of hepatocytes produce 90% of the proteins in blood plasma, including fibrinogen and albumin. Albumin is a carrier protein that binds to bilirubin and helps maintain osmotic balance in the blood. Fibrogen is essential for clotting. Hepatocytes cells show extensive networks of ER and Golgi body which provides evidence of high levels of protein synthesis. Estimated that 13 million ribosomes attached to ER of a liver cell. D.3 U1 The liver removes the toxins from the blood and detoxifies them. The liver also has a role in detoxification. The cells absorb toxic substances from blood a convert them into non-toxic or less toxic by a range of chemical conversions. Ex. Alcohol is converted into a less toxic substance by enzyme ethanol dehydrogenase. Ex. Converts toxic ammonia into urea. Also converts foreign compounds like converting hydrophobic compounds into more easily excreted hydrophilic compounds.