* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Bacterial infection and antibiotics
Globalization and disease wikipedia , lookup
Community fingerprinting wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Lyme disease microbiology wikipedia , lookup
Triclocarban wikipedia , lookup
Neonatal infection wikipedia , lookup
Trimeric autotransporter adhesin wikipedia , lookup
Horizontal gene transfer wikipedia , lookup
Cross-species transmission wikipedia , lookup
Schistosoma mansoni wikipedia , lookup
Infection control wikipedia , lookup
Bacterial cell structure wikipedia , lookup
Germ theory of disease wikipedia , lookup
Human microbiota wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
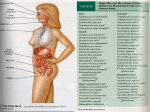
Molecular mimicry wikipedia , lookup
Bacterial Pathogenesis Bacterial infection and antibiotics --------------Bacterial pathogenesis (细菌致病机制) • References: 1. Murray, P. et al., Medical Microbiology (5th edition) 2. Samuel Baron, Medical Microbiology (4th edition) 3. Wilson, B.A. et al., Bacterial Pathogenesis: A Molecular Approach (3rd edition) 4. Falkow, S. and Miller, V.L., Molecular Genetics of Bacterial Pathogenesis: A Tribute to Stanley Falkow Outline Bacterial Pathogenesis • Introduction • Host Susceptibility • Pathogenic Mechanisms • Virulence Factors • Steps in Successful Infection pathogen Opportunistic pathogens The significance of normal flora • constitute a protective host defense mechanism: Competition of nutrients and receptors Metabolic substances by normal flora: e.g., bacteriocins, antibiotics, etc. • • serve a nutritional function: several B vitamins and vitamin K keep our immune systems in tune normal flora share many antigenic determinants with pathogenic organisms • Definition: normally nonpathogenic microorganisms capable of causing an infection in an immunosuppressed host. • Conditions of causing diseases by opportunistic pathogens: o Alteration of colonization sites o Declination of host immune system function Introduction of Bacterial Pathogenesis What a real pathogen will do? 1. Infection: growth and multiplication of a microbe in or on the body with or without the production of disease. 2. The capacity of a bacterium to cause disease reflects its relative “Pathogenicity (致病性).” 3. Virulence(毒力) is the measure of the pathogenicity of a microorganism. 4. Pathogenesis refers both to the mechanism of infection and to the mechanism by which disease develops. Host Susceptibility Obligate pathogens are more virulent and can cause diseases in a normal person. 1. Susceptibility to bacterial infections => Host Defenses vs Bacterial Virulence 2. Host Defenses: - Barriers (skin & mucus) – first line - Innate Immune Responses (complement, macrophages & cytokines) – the early stage - Adaptive Immune Responses (Ag-specific B & T cells) – the later stage 3. Host defenses can be comprised by destructing barriers or defective immune response. e.x. Cystic Fibrosis => poor ciliary function => NOT clear mucus efficiently from the respiratory tract => Pseudomonas aeruginosa => serious respiratory distress. Entry into the human body Opportunistic pathogens are typically members of normal flora and cause diseases when they are introduced into unprotected sites, usually occur in people with underlying conditions. Pathogen ↔ Disease The most frequent portals of entry- Mucus - Skin • Koch‘s postulates (科赫法则) – the pathogen must be present in every case of the disease – the pathogen must be isolated from the diseased host & grown in pure culture – the specific disease must be reproduced when a pure culture of the pathogen is inoculated into a healthy susceptible host – the pathogen must be recoverable from the experimentally infected host Routes: Ingestion, inhalation, trauma, needles, catheters, arthropod bite, sexual transmission : infection : shedding Stanley Falkow, Ph.D Molecular Koch's postulates • Microbiologist and a professor of microbiology and immunology at Stanford University School of Medicine • • The father of molecular microbial pathogenesis, which is the study of how infectious microbes and host cells interact to cause disease at the molecular level. • • He formulated molecular Koch's postulates, which have guided the study of the microbial determinants of infectious diseases since the late 1980s. • • President of the ASM (1997- 1998); elected member of the Institute of Medicine, the National Academy of Sciences, and the National Academy of Arts and Sciences. Fellow of AAAS, UK-FRS (Foreign member) • The prestigious Lasker Award for medical research (2008) • • • The iceberg concept of infectious disease Poliomyelitis(脊髓灰质炎) in a child 0.1-1% of infections are clinically apparent "The phenotype or property under investigation should be associated with pathogenic members of a genus or pathogenic strains of a species." Additionally, the gene in question should be found in all pathogenic strains of the genus or species but be absent from nonpathogenic strains. "Specific inactivation of the gene(s) associated with the suspected virulence trait should lead to a measurable loss in pathogenicity or virulence." Virulence of the microorganism with the inactivated gene must be less than that of the unaltered microorganism in an appropriate animal model. "Reversion or allelic replacement of the mutated gene should lead to restoration of pathogenicity." In other words, reintroduction of the gene into the microbe should restore virulence in the animal model. "The gene, which causes virulence, must be expressed during infection." "Immunity must be protective.“ For many pathogenic microorganisms, it is not currently possible to apply molecular Koch's postulates to a gene in question. Testing a candidate virulence gene requires a relevant animal model of the disease being examined and the ability to genetically manipulate the microorganism that causes the disease. Suitable animal models are lacking for many important human diseases. Additionally, many pathogens cannot be manipulated genetically. Characteristics of Pathogenic Bacteria 1. Transmissibility classical clinical disease 2. Adherence to host cells less severe disease 3. Invasion of host cells and tissue 4. Evasion of the host immune system Rubella(风疹) 50% of infections are clinically apparent 5. Toxigenicity asymptomatic infection Spectrum of virulence A bacterium may cause diseases by 1. Destroying tissue (invasiveness) 2. Producing toxins (toxigenicity) Rabies(狂犬病) 100% of infections are clinically apparent 3. Stimulating overwhelming host immune responses Pathological Mechanisms of Bacterial Infections 1. Bacteria-mediated Pathogenesis 2. Host-mediated Pathogenesis 3. Bacterial virulence factors Bacterial Virulence Mechanisms => bacterial factors causing diseases Adopted from Samuel Baron “Medical Microbiology” Bacterial virulence factors Adhesins Pili (fimbriae) Nonfimbrial adhesins Invasion of host cells Tissue damage Growth byproducts Tissue-degrading enzymes Immunopathogenesis Toxins Exotoxins (cytolytic enzymes and A-B toxins); enterotoxins; superantigens; endotoxin and other cell wall components Antiphagocytic factors Intracellular survival Antigenic heterogeneity Antigenic variation Phase variation Iron acquisition Siderophores Receptors for iron-containing molecules Resistance to antibiotics Microbial defenses against host immunologic clearance Encapsulation (Inhibition of phagocytosis and serum bactericidal effect) Antigenic mimicry Antigenic masking Antigenic or phase variation Intracellular multiplication Escape phagosome Inhibition of phagolysosome fusion Resistance to lysosomal enzymes Production of anti-immunoglobulin protease Inhibition of chemotaxis Destruction of phagocytes Mechanisms for escaping phagocytic clearance and intracellular survival Mechanisms for escaping phagocytic clearance and intracellular survival Mechanisms for escaping phagocytic clearance and intracellular survival Steps in successful infection • Sex comes before disease – acquire virulence genes • Sense environment – and Switch virulence genes on and off • Swim to site of infection • Stick to site of infection • Scavenge nutrients – especially iron • Survive stress • Stealth – avoid immune system • Strike-back – damage host tissues • Subvert – host cell cytoskeletal and signalling pathways • Spread – through cells and organs • Scatter Bacterial Sex Bacterial Sex acquiring virulence genes Mobile genetic elements • Bacteria have three ways of exchanging DNA – Transformation • cells take up naked DNA – Transduction • phages carry DNA – Conjugation • cells mate through specialised appendages • Transposons – ST enterotoxin genes • Virulence Plasmids – e.g. TTSSs in Shigella, Yersinia; toxins in Salmonella, E. coli, anthrax • Phage-encoded virulence – e.g. botulinum toxins, diphtheria toxin, shiga-like toxin (linked to lysis), staphylococcal toxins, TTSS substrates in Salmonella. Bacterial Sex Bacterial Sex Pathogenicity Islands Pathogenicity Islands • Concept originated from study of uropathogenic E. coli strains • Defining Features – Carriage of (many) virulence genes – Presence in pathogenic versus non-pathogenic strains – Different G+C content from host chromosome – Occupy large chromosomal regions (10-100 Kb) – Compact distinct genetic units, often flanked by DRs, tRNAs, ISs – Presence of (cryptic) mobility genes – Unstable, prone to deletion • often encode secretion systems – LEE region in EPEC – Spi1, Spi2 in Salmonella – Cag in H. pylori • can also encode adhesins, siderophores, toxins – Uropathogenic E. coli (Pai I, II, IV, V) – Yersinia spp. (HPI) – V. cholerae (VPI or TCP-ACF element) Sense environment • Bacteria can sense changes in environment – e.g. in temperature, nutrient availability, osmolarity, cell density (“quorum sensing”). • In simplest cases, change in intracellular concentration of ion linked directly to gene expression – e.g. fall in intra-cellular iron levels triggers de-repression of diphtheria toxin gene • In more complex cases, sophisticated signal transduction cascades allow bacteria to regulate gene expression in response to environmental cues – the pathogen as an information processor Switch virulence factors on and off A multi-layered hierarchy • Changes in DNA sequence – Gene amplification – Genetic rearrangements – Enterics, Campylobacter, Helicobacter, spirochaetes • Motility crucial for virulence in some cases • Usual organelle of motility=flagellum • Variants – Twitching motility – Swarming – Stability of protein, controlled cleavage – Covalent modifications • e.g. Hin flip-flop control of flagellar phase variation • Transcriptional Regulation • e.g. phosphorylation in two-component sensorregulator systems – Activators and Repressors (helix-turn-helix motif) – mRNA folding and stability Swim • Many bacterial pathogens are motile • Translational Regulation • Post-translational Regulation Stick • To avoid physical and immunological removal, bacteria must adhere to – cell surfaces and extracellular matrix e.g. in respiratory, gastrointestinal and genitourinary tracts – solid surfaces e.g. teeth, heart valves, prosthetic material – other bacteria • Direct interaction • Molecular bridging via e.g. fibronectin • Adherence often combined with manipulation of host cell signalling and cytoskeleton – Invasion – Intimate adherence Stick Stick • Common adherence mechanisms – Capsules and slime – Biofilm formation • Gram-positive adhesins – MSCRAMMs (microbial surface components recognizing adhesive matrix molecules), e.g. protein A – Fimbriae • Gram-negative adhesins (CHO and protein receptors) – Fimbriae, Afimbrial adhesins (FHA, Pertactin etc.) – Outer Membrane Proteins – Types III-IV secretion Scavenge nutrients e.g. iron • Free iron levels very low in body fluids – Acute phase response causes further drop – Iron overload increases susceptibility to infection • Many different bacterial systems for scavenging iron – Siderophores chelate available iron & transport it into bacteria – Iron can be scavenged direct from host iron-binding proteins, e.g by lactoferrin-binding proteins – Often co-ordinately regulated e.g. by fur locus in E. coli – Some pathogens avoid the problem by cutting out need for iron, e.g. Treponema pallidum • Iron used to regulate aggressive virulence factors – Diphtheria toxin (DtxR repressor) – Shiga-like toxin – Pseudomonas aeruginosa exotoxin A Survive Stress • In addition to nutrient-limitation stress, pathogens face many other stresses – Acid stress within stomach – Heat shock during fever – Oxidative stress within phagocytes • Stress response proteins, such as chaperonins, feature as immunodominant antigens • Detoxification proteins play a role in virulence, e.g. periplasmic Cu,Zn-superoxide dismutases • Infectious dose for enteric pathogens much lower in achlorhydria (no need to overcome acid stress) Stealth Stealth avoid immune system • IgA proteases – metalloproteases active against IgA • Immunoglobulin-binding proteins – e.g. protein A of S. aureus • Resist complement, opsonisation – Capsule (usually polysaccharide) – Lipopolysaccharide – Surface proteins and OMPs • Antigenic mimicry avoid immune system • Antigenic or phase variation – Involves surface structures such as proteins, LPS, capsules – Variety of mechanisms • slip-strand mispairing • flip-flop • cassettes • Adopt cryptic niche – inside phagocytes – in biofilm – e.g. sialic acid capsule of group B meningococcus Strike-back 67700 67710 67720 GAAGTGCATTTAACTT**GGGGGGGGGGGTAAT GAAGTGCATTTAACTT*GGGGGGGGGGGGTAAT GAAGTGCATTTAACTTGGGGGGGGGGGGGTAAT GAAGTGCATTTAACTT***GGGGGGGGGGTAAT GAAGTGCATTTAACTT**GGGGGGGGGGGTAAT GAAGTGCATTTAACTT****GGGGGGGGGTAAT GAAGTGCATTTAACTT*GGGGGGGGGGGGTAAT GAAGTGCATTTAACTT**GGGGGGGGGGGTAAT GAAGTGCATTTAACTT***GGGGGGGGGGTAAT GAAGTGCATTTAACTT***GGGGGGGGGGTAAT GAAGTGCATTTAACTT***GGGGGGGGGGTAAT GAAGTGCATTTAACTT**GGGGGGGGGGGTAAT GAAGTGCATTTAACTT*GGGGGGGGGGGGTAAT Homopolymeric tract in Campylobacter jejuni Endotoxin of Gram-negatives Damage host tissues • Endotoxin • Exotoxins Gramnegative cell cytopl. mem. peptidoglycan outer mem. – Toxins acting on cell membranes – Toxins active inside cells – Superantigens Lipopolysaccharide (LPS) Lipid A Core polysaccharide O sidechain The toxic part Helps solubilise Lipid A Somatic antigen Strike-back Endotoxin • Actions of Endotoxin – Pyrogenicity – Leucopenia then leucocytosis – Hypotension • • • • “Gram-negative Shock” Life-threatening complication of septicaemia e.g. in meningococcal infection, in ITU or oncology patients Endotoxic shock seen with dirty intravenous equipment • Most of the effects of endotoxin are mediated by tumour necrosis factor – Attempts at therapy using anti-endotoxin or anti-TNF antibodies Strike-back Toxins active inside cells • Toxins often consist of translocation and binding B subunit that delivers the active A subunit into the host cell cytoplasm • Example of AB toxin: diphtheria toxin an ADP-ribosyltransferase Strike-back Membrane-Damaging Exotoxins • Many bacterial toxins form pores in eukaryotic cell membranes, producing oligomeric rings, e.g. – streptolysin O of Streptococcus pyogenes – listeriolysin of Listeria monocytogenes – alpha-toxin of S. aureus • Other toxins, such as phospholipases, degrade components of the membrane – e.g. Clostridium perfringens alpha toxin AB5 Toxins LYSIS Spread Subvert • inject proteins into host cells to subvert the cytoskeleton and signal-transduction pathways: – manipulating (e.g. Rho GTPases and the cytoskeleton) to induce membrane ruffling and bacterial invasion – preventing uptake by phagocytic cells, e.g. Yersinia spp. and Pseudomonas spp. – remaining within a vacuole by manipulating host cell vesicular transport and endocytosis …through cells and organs: • within macrophages, e.g. in typhoid • through blood (need to be complement-resistant) • within cells – actin-based motility of Listeria monocyogenes, depends on ActA protein. Scatter Summary Transmission, virulence and evolution • Established dogmas – balanced pathogenicity – being too virulent is no good – high virulence is a sign of recent emergence of a pathogen – pathogens evolve towards symbiosis • Counter-arguments – Where pathogens rely on spread through biting arthopods, high bacteraemias advantageous – Where pathogens rely on shedding into water, highest possible shedding rates good for pathogen – Where pathogens cause incidental disease (e.g. Legionella) no selective pressure towards low virulence – Virulence as a local adaptation (why meningitis?) – Bad vaccines and effect on virulence • Spectrum of virulence – Commensals – Opportunistic pathogens – Obligate pathogens • Difficulties in linking pathogen to disease – Koch’s postulates – Molecular Koch’s postulates • Multi-dimensional view of virulence • • • • • • • • • • • • Sex Sense Switch Swim Stick Scavenge Survive stress Stealth Strike-back Subvert Spread Scatter Home Work 1. Name at least 3 ways bacterial pathogens can evade host defence. 2. What is endotoxin? What is exotoxin? 3. Why both escaping and overly stimulating immune system are bad for the host being infected?