* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Overview of Tenofovir`s Anticipated Adverse Events and Resistance
Psychopharmacology wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Drug interaction wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Metalloprotease inhibitor wikipedia , lookup
Discovery and development of non-nucleoside reverse-transcriptase inhibitors wikipedia , lookup
Discovery and development of neuraminidase inhibitors wikipedia , lookup
HIV vaccine wikipedia , lookup
Discovery and development of HIV-protease inhibitors wikipedia , lookup
Discovery and development of integrase inhibitors wikipedia , lookup
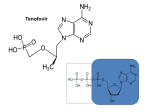
Overview of Tenofovir’s Anticipated Adverse Events and Resistance Concerns Devika Singh, MD, MPH Protocol Safety Physician VOICE Training July 2010 Today’s Discussion How does tenofovir work against HIV? What human body systems does it affect? What adverse events can we anticipate when tenofovir is used? HIV Life Cycle How does HIV enter the cell, and copy itself? How do drugs exploit this process? Key Concepts: Anti-retroviral (ARV) ARVs are drugs to treat HIV designed to interfere with virus’s ability to replicate They are best used in combination, i.e., anti-retroviral therapy (ART) Different ARVs target different steps in the HIV life cycle Generally, ARVs are safe and effective Approved Antiretrovirals (ARVs) Nucleoside / tide reverse transcriptase inhibitors: Zidovudine Didanosine Zalcitabine Stavudine Lamivudine Abacavir Emtricitabine Tenofovir Non-nucleoside reverse transcriptase inhibitors: Delavirdine Nevirapine Efavirenz Etravirine These drugs were approved in 2007/2008 Protease inhibitors: • • • • • • • • • • Indinavir Saquinavir Nelfinavir Amprenavir Fosamprenavir Lopinavir Atazanavir Darunavir Tipranavir Ritonavir Fusion / Co-receptor inhibitors: • • Enfuvirtide Maraviroc Integrase Inhibitors: • Raltegravir 2 keys are needed to “open the door” CD4 & chemokine receptors are required for viral entry Fusion / Entry Inhibitors Viral RNA is released (yellow strands) Reverse transcription occurs Genetic data is copied backwards from viral RNA to DNA (Viral RNA yellow, DNA blue) Reverse transcriptase inhibitors Work by blocking this process www.cellsalive.com Tenofovir Nucleoside reverse transcriptase inhibitor (NRTI) drug used to treat HIV-1 infection in adults Interferes with HIV’s ability to reproduce itself by inhibiting reverse transcriptase Fusion / Entry Inhibitors Reverse Transcriptase Inhibitors Fusion / Entry Inhibitors Reverse Transcriptase Inhibitors Fusion / Entry Inhibitors Reverse Transcriptase Inhibitors Integrase Inhibitors Viral DNA integrates into the host chromosome DNA www.cellsalive.com HIV uses the CD4 cell as a virus producing machine Cell operates like a photocopier Viral RNA coming off the photocopy is packaged in an `envelope` Eventually runs out of toner www.cellsalive.com Viral Protease is an enzyme that cuts up proteins These new virions are now mature www.cellsalive.com Protease inhibitors (PIs) block protease and inhibit replication www.cellsalive.com Fusion / Entry Inhibitors Protease Inhibitors Reverse Transcriptase Inhibitors Integrase Inhibitors Release of new HIV virions Mature virions are now available to infect new CD4 cells. This is how CD4 cells are profoundly depleted as HIV infection progresses Tenofovir Dose: one 300 mg tablet taken once a day, with or without food Used in combination with other oral drugs Safety profile comparable to placebo Resistance emerges slowly Also called Viread® or TDF Truvada Combination drug - tenofovir and emtricitabine (FTC) Both are NRTI’s One tablet contains 200 mg of FTC and 300 mg tenofovir taken once a day Safety profile similar to tenofovir Also called Truvada®, FTC/TDF or tenofovir+FTC Oral Tenofovir: How It’s Handled Oral bioavailability ~25% After taking 300 mg orally, maximum serum concentrations are achieved in about 1 hour (+/- 0.4 hours) Half-life is 17 hours; persists in peripheral blood cells much (PBMC) longer Must be taken up by cells to be activated Tenofovir Diphosphate Cellular kinase Tenofovir (TDF; inactive) Cellular kinase Tenofovir monophosphate (inactive) Tenofovir diphosphate (active) Intracellular Extracellular TDP: tenofovir diphosphate is active form; 2 phosphates added inside cells TDF: tenofovir disoproxil fumarate; Inactive prodrug; only active after modification inside cells Potential adverse effects/events What body systems does tenofovir affect? Kidney Bone Liver Adverse Events That May Lead to Product Hold Hypophosphatemia Decreased creatinine clearance Nausea Dipstick abnormalities Clinical experience with Tenofovir: >12,000 in expanded access programs Clinical Trial Experience 3 large published clinical trials in HIV+; N = 1,544 (Gilead 903, 934, 907) Incidence >10%, Grades 2-4 Rash Diarrhea Headache Pain Depression Nausea Oral Tenofovir: Elimination Tenofovir is eliminated by the kidney at two sites and using two mechanisms Glomerular filtration Active tubular secretion The Nephron, Basic Unit of the Kidney Glucose, water, salts & small metabolites are filtered through glomerulus & pass through to tubule Reabsorbed there Protein is filtered at glomerulus (kept in blood) TDF effect on kidney function • Can affect the proximal tubule • Accumulates in the proximal tubule • “Spilling” of glucose and phosphate in urine (glucosuria, hypophosphatemia) TDF effect on kidney function • Can also affect the glomerulus, making it “leaky” • Protein in urine • Lowered creatinine clearance • Elevated serum creatinine TDF effect on kidney function • Accumulates in the proximal tubule • “Spilling” of glucose and phosphate in urine (glucosuria, hypophosphatemia) • Can also affect the glomerulus • Protein in urine • Lowered creatinine clearance (creatinine, CrCl and proteinuria) • Tubular effects more common (cohort studies suggest ~2% incidence) • Also a small, stable increase in creatinine Summary Tenofovir accumulates in the proximal tubule cells and can be toxic Causes “spilling” of glucose and phosphate in urine Look for glucosuria and hypophosphatemia in VOICE Tenofovir can also affect the glomerulus Protein in urine is due to damage at glomerulus Why we look for changes in creatinine and proteinuria in VOICE Tenofovir Kidney Toxicity: Summary Cohort studies suggest ~2% incidence of tubule problems in HIV patients treated with TDF Small, stable increase in creatinine Normal renal response to acidemia is to reabsorb all of the filtered bicarbonate and to increase hydrogen excretion primarily by enhancing the excretion of ammonium ions in the urine Impairment of this can lead to renal tubular acidosis (RTA) Tenofovir effect on liver Liver enzymes (AST, ALT) = hepatitis Lactic Acidosis / Severe Hepatomegaly with steatosis (fatty infiltration of liver) Can occur with tenofovir use alone or in combination anti-HIV therapy May not have increases in liver enzymes (transaminitis) Majority of cases in women Obesity and prolonged concomitant nucleoside use may be risks Pre-existing liver disease not necessary Tenofovir & Hepatitis B Tenofovir is a treatment for hepatitis B infection Worsening of chronic hepatitis B has been observed after stopping tenofovir abruptly Black box warning in package insert Flares typically self-limited, but some reports of more serious liver damage For this reason, VOICE will exclude women with chronic hepatitis B (HBSAg+) and encourage immunization for women vulnerable to future infection Tenofovir: Post-Marketing Experience Renal insufficiency, renal failure, acute renal failure, Fanconi syndrome, proximal tubule problems, protein loss in urine, increased creatinine, acute tubular necrosis (severe damage), nephrogenic DI (diabetes insipidus), polyuria, interstitial nephritis liver enzymes (AST, ALT) --> hepatitis Hypophosphatemia, lactic acidosis Myopathy, osteomalacia (both associated with proximal renal tubulopathy) Allergic reaction Dyspnea Abdominal pain, amylase, pancreatitis Rash Asthenia Tenofovir: Precautions New onset or worsening renal impairment, including acute renal failure & Fanconi syndrome Assess creatinine clearance pre-initiation; dose adjust if <50 Monitor creatinine clearance and phosphate in patients at risk Avoid drugs that might damage the kidneys *Package insert Tenofovir: Precautions Decreases in bone mineral density in HIV+ persons Consider monitoring if h/o pathologic fracture or osteopenia risk Osteomalacia (softening of bones) can also result from Fanconi syndrome (loss of important minerals from kidney tubule) Lipodystrophy - redistribution/accumulation of body fat No data on setting when tenofovir is used as the only anti-HIV drug *Package insert Truvada: Anticipated AE’s Essentially contained in information already presented about Tenofovir information (and in its drug description/package insert) EXCEPT for: Skin discoloration Hyperpigmentation (darkening of skin) primarily on palms and soles Generally mild and asymptomatic Implications for product hold? None discontinued for this reason in clinical trials Oral PrEP:One Completed Trial West Africa Phase II PrEP Trial (FHI/BMGF) in HIV-negative women (n=936) in Ghana, Cameroon, Nigeria RCT: daily TDF 300 mg and placebo Conducted June 2004 - March 2006 No evidence of increased clinical or laboratory adverse effects Peterson L, et al. PLoS Clinical Trials 2007 Phosphate In FHI PrEP study, one grade 3 hypophosphatemia was seen in 428 p-y followup (Peterson 2007) Partners PrEP study & MTN001 to date: Not uncommon Several grade 2 and one grade 3 hypophosphatemia Nearly all NOT found to be persistent with repeat testing; phosphate levels may vary in normal, healthy people Few holds for phosphate abnormalities Adverse Events That May Lead to Product Hold Hypophosphatemia Decreased creatinine clearance Nausea Dipstick abnormalities 1% Tenofovir Vaginal Gel Active ingredient is tenofovir (also called PMPA) Provided in pre-filled applicators (40 mg TFV in 4 ml) Leads to low levels of drug in the blood Most levels below 5 ng/mL Detectable in 79% of HPTN059 participants Low frequency of side effects Tenofovir 1% Gel: Clinical Experience HPTN 050: Phase I study with 14 days of product exposure Male tolerance study (CONRAD) PMPA gel safe and acceptable in HIV-infected and uninfected women (Mayer, AIDS 2006) No complaints HPTN 059: Expanded safety study of 200 HIV-uninfected women in India and US (Hillier, Microbicides 2008, New Delhi) HPTN-059 Lessons Learned Safety: Daily or coitally dependent 1% tenofovir gel no different from placebo Adherence: Coitally dependent adherence within 2 hours of sex: 80%; 83% of daily doses reported used PK: 79% of women reporting gel use in past 12 hours had low but detectable plasma tenofovir supporting self reported adherence data Acceptability: Daily and coital use highly acceptable to women and they would use it if found to be effective at preventing HIV Key Concepts: Resistance Definition: ability of a microorganism to survive and multiply in the presence of drugs that would normally kill or weaken it. For HIV, drug resistance means the virus is no longer sensitive to one or more ARV HIV is “resistant” to a medicine if it keeps reproducing even while a person is taking that medicine Key Concepts: Resistance How does it happen? The enzyme HIV needs to replicate (reverse transcriptase) is error prone, resulting in mistakes (mutations) Some mutations make the virus not sensitive to a drug The drug-resistant virus can now replicate and take over other drug-sensitive virus Resistance Resistance is common in HIV-infected people being treated with ART Where ART is widely used, 5-20% of new HIV infections can involve drug-resistant virus Can be managed when detected early (suppressed by other ARV combinations) However, treatment options may be limited for some types of resistance Will resistance be a problem? We don’t know Very little scientific or clinical information is available about the nature or incidence of resistance among those using ARV-based microbicides or oral ARVs for prevention, however Limited modeling data suggest circulating drug resistance in the community won’t limit PrEP effectiveness (Van de Vijver, JID, 2009) Resistance with PrEP? Impact on future care for people infected while on PrEP is unknown FHI trial in 936 HIV-negative women in Ghana (primarily), Cameroon and Nigeria with daily tenofovir: Tenofovir safe – no serious side effects 8 seroconversions occurred: 2 in the active arm and 6 in placebo arm HIV infections too few to draw conclusions on efficacy Moving Forward Resistance will be a risk associated with being in a study like VOICE At the same time, much more research is needed because we know very little The risks are not considered high enough to think that PrEP studies should not be done Summary: Implications Non-specific, generalized complaints occur commonly with tenofovir Most will not necessitate product hold However, presentation of severe AEs (ARF, lactic acidosis), require balance between high index of suspicion for immediate laboratory evaluation & prudent watchful waiting Clinical judgment will be critical! We are carefully monitoring for HIV resistance and want to minimize use of study products in established HIV infection Acknowledgments Jeanne M. Marrazzo Jane E. Hitti Questions? Serologic markers of acute hepatitis B with recovery HBV detectable by PCR Source: http://www.cdc.gov/ncidod/diseases/hepatitis/slideset/index.htm Serologic diagnosis of chronic hepatitis B HBV detectable by PCR Source http://www.cdc.gov/ncidod/diseases/hepatitis/slideset/index.htm Hepatitis B serology interpretation (Appendix IV of protocol) Test Result Interpretation & Management HBsAg Negative HBV susceptible (offer vaccination) Flag chart & set up vaccination tracking log If declined, counsel about infection risk & potential for flares if ppt becomes infected Revisit need for vaccination regularly & test annually, at PUEV & 6mths after PUEV (oral). anti-HBs Negative HBsAg Negative anti-HBs Positive possibly due to prior infection or vaccination Flag chart as “HBV Immune”. No further action needed HBsAg Positive HBV anti-HBs Negative “Immune” infected. Not eligible if at screening. If detected during follow up, permanently stop product & refer for care (per local standard) AST/ALT at 1,2, 3 months after initiation of product hold (Section 7.6.2) Timing matters Resistant virus is overtaken by sensitive virus within weeks of stopping ARVs Monkey studies: virus initially transmitted is usually not drug-resistant, but resistance is more likely with time if the PrEP ARV is continued Mothers who took single dose nevirapine for pMTCT and developed nevirapine resistance: no decrease in response to ARV treatment if initiated after 6 months (Mashi Study) For this reason, we are testing frequently for new HIV infection, and stopping study product immediately if it’s detected (or strongly suspected)