* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download diuretics
Survey
Document related concepts
Transcript
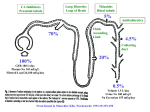
DIURETICS Victor Nadler A diuretic is an agent that increases the rate of urine formation. Urine volume increases with a net loss of solute and water. Diuretics are safe, effective, and cheap drugs. Several classes of diuretics are used to produce a variety of clinically-beneficial effects. These include reduction of blood pressure, treatment of acute and chronic congestive heart failure, reduction of localized or generalized edema, improvement of renal function, reduction of aqueous humor volume, and correction of specific ion imbalances. Effects of diuretics, when they are being used to increase urine volume, can be explained by alteration of renal physiology. Note, however, that some important effects of diuretics involve actions at sites other than the kidney. Relevant Features of Renal Physiology The glomerular filtration rate of healthy adults is usually about 1.7-1.8 ml/min/kg. More than 99% of this filtrate is transferred from tubular lumen back to the blood. Although other substances are involved, + reabsorption mainly involves the recovery of Na with water passively following. Indeed more than 90% + of the oxygen consumption of the kidney is spent on Na reabsorption. There are several mechanisms of + Na reabsorption; they differ in different parts of the nephron. Reabsorption of solutes involves movement from the tubular lumen across the apical membrane of the tubular epithelial cell, from the epithelial cell across its basolateral membrane, and from the interstitial fluid into the capillaries. The capillary membrane normally presents an insignificant barrier to reabsorption, because the fluid pressure of the extracellular space greatly exceeds that in the capillaries and because the capillary blood is relatively concentrated due to previous glomerular filtration of water. Reabsorption across the + + basolateral membrane depends on the energy-requiring Na /K -ATPase. Anions and water passively + accompany the Na . Reabsorption across the apical membrane is accomplished by a variety of channels and pumps that differ in different parts of the nephron. 1 + Proximal Tubule About 65-70% of the filtered Na and water is reabsorbed in the proximal tubule. + + There are four mechanisms of Na reabsorption. (1; A in the top figure) Na channels are present in the + apical membrane of tubular epithelial cells throughout the proximal tubule. Diffusion of Na through these channels is favored by the internal electronegativity of the epithelial cells. This electronegativity is created + + + + by the operation of Na /K -ATPase, which extrudes 3 Na ions for every 2 K ions countertransported. (2; + B in the top figure) Na is cotransported with glucose, amino acids, phosphate and other vital metabolites. + + (3; C in the top figure) Na is exchanged for H by a carrier molecule. In the early part of the proximal tubule, this mechanism supports the excretion of metabolic acid and reabsorption of HCO3 . In the late part of the proximal tubule, Na+/H+ exchange is coupled to Cl-/anion exchange, which results in the reabsorption + of Na+ and Cl- and excretion of organic acids. (4) Na passively follows Cl , which diffuses through the tight junctions between epithelial cells. Mechanisms 1, 2, and 3 operate in the early (convoluted) part of the proximal tubule. Mechanisms 1, 2, and 4 operate in the late (descending) part of the proximal tubule. + + + Reabsorption of K is purely passive. The epithelial cell membranes are permeable to K and some K + + + diffuses through the tight junctions. However, some K is pumped back into the epithelial cell by Na /K + ATPase. Thus only about half the K in the proximal tubular fluid is reabsorbed. 2 + + - Thick Ascending Limb One key feature of this region of the nephron is Na /K /2 Cl + cotransport. Na flows through channels in the apical membrane into the luminal epithelial cell. This + + entry of Na turns on a transporter called NKCC2 that pumps K and 2 Cl into the epithelial cell against + + + their electrochemical gradients. Na /K -ATPase in the basolateral membrane pumps Na accompanied by + Cl into the interstitial fluid. The other Cl flows through a specific channel into the interstitial fluid. K can flow through specific channels either back into the lumen or into the interstitial fluid. Another feature of the thick ascending limb that facilitates cation reabsorption is that the interstitial space is electrically negative relative to the tubular lumen. This electronegativity is created by the flow of K+ only through the apical membrane, whereas both K+ and Cl- flow through the basolateral membrane. It encourages the 2+ 2+ reabsorption of cations, including Ca and Mg , through the tight junctions between epithelial cells. By + + the end of the thick ascending limb, nearly all the remaining Na and K are reabsorbed; only 5-10% of the + + Na originally filtered and only 10% of the K remain in the tubular fluid. The second key feature of this region is the low permeability of the tubular epithelium to water. The reabsorption of salt with little water in the thick ascending limb is the mechanism that allows the kidney to excrete a urine more dilute than plasma. The same mechanism creates the interstitial hyperosmolarity necessary for the countercurrent exchange system and thus for concentration of the urine. Thus both dilution and concentration of the urine depend on the activity of NKCC2. 3 + - Distal Tubule The apical membrane of tubular epithelial cells has a Na /Cl co-transporter. + + + Na is pumped across the basolateral membrane by Na /K -ATPase with Cl following by diffusion through + specific channels. This process plays a relatively minor role in overall Na reabsorption, because there is + relatively little Na left in the tubular fluid at this time. Distal tubular cells are also the site of parathyroid 2+ hormone- and vitamin D-sensitive Ca reabsorption. Ca2+ enters the tubular epithelial cells through voltage-sensitive channels in the apical membrane and is exchanged for Na+ in the basolateral membrane. Like the thick ascending limb, the epithelium of the distal tubule has a low permeability to water. Collecting Duct When the tubular fluid reaches the collecting duct, about 20% of the filtered water + and less than 5% of the filtered Na remain. Thus the collecting duct receives a relatively small volume of dilute fluid. This is the major site for physiological regulation of salt and water balance. Vasopressin (a.k.a. anti-diuretic hormone, ADH) controls the permeability of the tubular epithelium to water. It acts on the V2 receptor that is coupled to adenylate cyclase. Without vasopression, the apical membrane of collecting duct epithelial cells has a low permeability to water. Vasopressin causes additional water channels (aquaporins) to be inserted into the apical membrane. Water can then flow down its concentration gradient from the dilute fluid of the collecting duct to the hyperosmolar environment of the interstitial fluid that lies between the collecting duct and the loop of Henle. Water reabsorption in the collecting duct thus depends on the plasma vasopressin concentration, the osmolarity of the tubular fluid, and the osmolarity of the interstitial fluid. The hyperosmolarity of the interstitial fluid depends on the functioning of NKCC2 in the thick ascending limb. + + Aldosterone controls the amount of Na and K present in the final urine. Aldosterone induces the synthesis of a complex of proteins. Although the mechanisms involved are poorly understood, these + + + proteins increase the number of Na channels in the apical membrane. The number of Na /K -ATPase + molecules in the basolateral membrane also increases, but at a slower rate. Na flows into the luminal + + epithelial cells through its channels and is then pumped into the interstitial fluid by Na /K -ATPase. + Simultaneously, K is pumped into the epithelial cell across the basolateral membrane. The diffusion 4 + + of Na through the apical membrane creates an electrical potential (+ inside, - outside) that causes K to + diffuse out of the cell into the tubular lumen. Another reason for K secretion at this site is that the tubular + lumen is less electropositive than the interstitial space. Thus aldosterone promotes Na reabsorption + + and K secretion. This process is enhanced by a high fluid volume and/or a large quantity of Na in the fluid that reaches the collecting duct. Renal Handling of Inorganic Ions Sodium Reabsorbed by diffusion through selective ion channels, cotransport with nutrients, + + Na /H exchange, passive diffusion through tight junctions following Cl , Na /K /2 Cl cotransport and + + Na /Cl cotransport. The driving force for reabsorption of Na and counterions from the tubular epithelium + + to the circulation is Na /K -ATPase activity. + Potassium Passive reabsorption in the proximal tubule. Active secretion by exchange for Na in the collecting duct. + + + Chloride Reabsorbed passively with Na . Reabsorbed actively by Na /K /2 Cl cotransport and + Na /Cl cotransport. + + Bicarbonate Reabsorbed in association with Na /H exchange in the proximal tubule. There is little movement of HCO3 in the rest of the nephron. Calcium Specifically reabsorbed in the distal tubule. Major site of passive reabsorption is the + 2+ thick ascending limb. Most drugs that increase the excretion of Na have the same effect on Ca . Magnesium Major site of passive reabsorption is the thick ascending limb. Drugs that increase + 2+ the excretion of Na have the same effect on Mg . + + Major Classes of Diuretics Osmotic Diuretics Prototype: Mannitol Mechanism of action The simplest diuretic would itself be a solute that holds water in the tubular lumen. It must be filtered, but little can be reabsorbed. It should also be pharmacologically inert, metabolically inert, and nontoxic. The osmotic diuretics fit this description. The one most often used is mannitol. Mannitol must be administered iv, because it is not absorbed from the GI tract. Obviously, to be effective it must be given in large amounts. Mannitol distributes throughout extracellular body water (except for the brain and the eye). The extracellular hypertonicity draws water out of cells. Thus mannitol increases both plasma volume and total extracellular fluid volume. There are two components to the mechanism of osmotic diuretics: increased osmolarity of the glomerular filtrate and reduction of renal interstitial osmolarity. Because the glomerular filtrate now has an increased osmolarity, reabsorption of ions in the proximal tubule is accompanied by less reabsorption + of water. Thus the ionic composition of the tubular fluid initially falls. However, changes in the Na gradient across the apical membrane and other compensatory mechanisms lead to some increase in the urine concentration of all the inorganic ions. The increased renal interstitial blood flow removes solutes from the normally hypertonic interstitial fluid, thus partially counteracting the countercurrent exchange system. The kidney is less able to concentrate the urine. The combination of these two effects leads to about a 10-fold increase in urine volume. Clinical uses Osmotic diuretics are used primarily in a hospital setting. Mannitol is used to maintain renal function in persons with renal failure, who are being treated with a nephrotoxic drug like cisplatin, or who have overdosed on salicylate, barbiturate, etc. Its role in these circumstances is 5 to increase urine volume, thus protecting the renal tubular epithelium from dehydration and flushing potentially damaging drug from the body. Mannitol is also frequently used for its dehydrating actions outside the kidney. Here it is important to remember that mannitol does not enter the brain or the eye. Therefore the high concentration of mannitol in the blood tends to draw water from the brain and eye, particularly when intracranial or intraocular pressure is elevated. This action is very useful in the treatment of cerebral edema (due to head trauma or neurosurgery) and angle-closure glaucoma. Powdered mannitol can be used to reduce bronchial mucus in persons with cystic fibrosis. Thiazides (a.k.a. Benzothiazides) Prototypes: Hydrochlorothiazide, Chlorthalidone Mechanism of action The mechanism by which thiazide diuretics resolve edema and cause an initial fall in blood pressure differs from the mechanism by which these drugs reduce blood pressure over the long term. + Thiazide diuretics inhibit Na /Cl cotransport in the distal tubule This action produces only + about a 3-fold increase in urine volume, because Na /Cl cotransport accounts for only a small percentage + of the total ion reabsorption in the renal tubules. There is a net loss of Na . Unlike other diuretics, thiazides 2+ + 2+ uncouple Ca excretion from Na excretion. Ca reabsorption is actually enhanced. Although the mechanism is not fully understood, thiazide diuretics promote the reabsorption of Ca2+ in the distal tubule by increasing influx through a unique type of Ca2+ channel expressed in the apical membrane of the epithelial cells. Reduction of plasma and extracellular fluid volume plays only a relatively minor role in the sustained antihypertensive effect of thiazide diuretics. The 3-fold increase in urine volume occurs only during the first few days to months of therapy. This initial fluid loss is accompanied by a transient drop in extracellular fluid volume that resolves peripheral edema. The accompanying reduction in cardiac output reduces blood pressure transiently. However, compensatory mechanisms (e.g., increased renin secretion, + enhanced activity of Na reabsorption mechanisms in the renal tubules) substantially reduce urinary volume after this time, and cardiac output returns to the pretreatment value in 4-6 weeks. 6 The long-term reduction in blood pressure is clearly attributable to a fall in peripheral resistance. Thiazide diuretics do exert direct vasorelaxant activity when perfused through arterial tissues. However, the mechanism by which thiazide diuretics produce this effect is not understood. One theory to explain this effect postulates that thiazide diuretics act directly on vascular smooth muscle to facilitate opening of a Ca2+-dependent K+ channel (i.e., a K+ channel whose opening is stimulated by increased cytoplasmic Ca2+ concentration). Opening of these channels hyperpolarizes the smooth muscle fiber and thus inhibits the opening of voltage-dependent Ca2+ channels. Because Ca2+ entering the vascular smooth muscle cell by this route is important for the generation of Ca 2+ action potentials and for the strength of contraction, the indirect inhibition produced by thiazide diuretics results in vasodilation. However, the small (~5%) lasting reduction in plasma Na+ concentration may also play a role. This should lead to Na+ depletion in vascular smooth muscle cells, which triggers an outward movement of cytoplasmic Ca 2+ via the Na+/Ca2+ exchanger. In addition, reduction of extracellular Na+ would be expected to reduce the contribution of Na+ to arterial and cardiac remodeling. Finally, recent work suggests that sodium-dependent hypertension involves a failure of vascular endothelial cells to increase NO production. Some studies suggest the direct vasodilatory effect of thiazide diuretics depends on an intact endothelium. These drugs may therefore work at the level of the endothelium to enhance NO production. Clinical uses Thiazide diuretics are commonly used antihypertensive drugs. Results of a large clinical trial (ALLHAT trial) showed that, for the North American population, thiazide diuretics (specifically chlorthalidone) reduce certain cardiovascular morbidities more effectively than ACE inhibitors, calcium channel blockers, or 1 receptor antagonists. The difference between thiazide diuretics and beta blockers or ACE inhibitors/ARBs is greater for the African-American population. Thiazide diuretics are very cheap and seldom produce bothersome side effects when used at the proper dose. As monotherapy for essential hypertension, thiazides are particularly successful over the long term in patients 7 + whose hypertension is caused by excessive Na retention (“sodium-dependent hypertension”). These individuals develop generalized edema in the presence of a normal sodium intake and also exhibit low plasma renin levels and low NO production. The relief of edema and excretion of excess Na+ provided by the diuretic adds to the benefit derived from relaxation of vascular smooth muscle. As many as two-thirds of all black people with hypertension may fall into this class. In addition, hypertension in the elderly and in obese individuals usually develops a major sodium-dependent component. Thiazide diuretics reduce blood pressure, relative to other first-line antihypertensive drugs (except for calcium channel blockers), more successfully in these populations. In addition, thiazide diuretics are normally used as the second drug in patients who require a second drug to normalize their blood pressure and who were prescribed a calcium channel blocker, ACE inhibitor, or ARB initially. Their effect is additive to that of the calcium channel 2+ blocker and can be synergistic with that of the ACE inhibitor or ARB. The enhancement of Ca reabsorption by thiazide diuretics is particularly useful in persons with osteoporosis or who are at risk for developing osteoporosis. JNC-7 (the Seventh Report of the Joint National Committee on High Blood Pressure) published in 2003 recommended that a thiazide diuretic be used as initial pharmacotherapy for all patients with hypertension, except those with chronic kidney disease, are immediately postmyocardial infarction, or who are diabetic and are adequately treated with an ACE inhibitor/AT1 receptor blocker (ARB) for renal protection. That is still the position of the American College of Cardiology, the American Heart Association, and the Centers for Disease Control. However, JNC-8 published in 2014 and statements from the American and International Societies of Hypertension recommend initial pharmacotherapy with a thiazide diuretic, vascular-specific calcium channel blocker, ACE inhibitor, or ARB in non-black patients and either a thiazide diuretic or vascularspecific calcium channel blocker in black patients. Note that the thiazide diuretic used in the ALLHAT trial was chlorthalidone. Clinical studies have shown hydrochlorothiazide inferior to ACE inhibitors and dihydropyridine-type (vascular-specific) calcium channel blockers in reducing cardiovascular morbidity and mortality. Yet chlorthalidone appears superior in some respects to antihypertensive drugs of these other classes. Indeed the superiority of chlorthalidone over hydrochlorothiazide has been demonstrated. It may be that the longer duration of action of chlorthalidone provides better management of blood pressure over 24 hr than is possible with once-a-day hydrochlorothiazide, but chlorthalidone also opens K+ channels in vascular smooth muscle with greater potency than hydrochlorothiazide. Chlorthalidone therefore should probably be chosen in preference to hydrochlorothiazide whenever possible. In addition, combinations of chlorthalidone with an antihypertensive drug from another class have begun appearing on the market. These combinations should be optimal for treatment of Stage 2 hypertension. However, most preparations that combine a thiazide diuretic with an antihypertensive drug from another class contain hydrochlorothiazide. One mechanism the body uses to counter the effect of the thiazide diuretic is to increase renin secretion. Angiotensin II, a potent vasoconstrictor, is produced. Diuretics are less effective than they otherwise would be because their antihypertensive effect is partially counteracted by angiotensin II-induced vasoconstriction. By blocking the actions of renin, an ACE inhibitor or ARB makes the thiazide diuretic a more efficacious antihypertensive drug. The combination of thiazide diuretic and ACE inhibitor or ARB can produce a large reduction in blood pressure (20-25 mm Hg, sometimes greater than one would like). This is particularly important in the treatment of Stage 2 sodium-dependent hypertension, a condition in which ACE inhibitors and ARBs alone have little effect (due to low plasma renin). It is now recommended that, if blood pressure is more than 20/10 mm Hg above the goal blood pressure, therapy should be initiated with two drugs, one of which is usually a thiazide diuretic unless there is a compelling reason not to use the diuretic. Problem: hypokalemia, hypomagnesemia Most of the significant side effects of thiazide + 2+ diuretics result from K /Mg depletion. They are uncommon when the diuretic is used at the recommended + + dose. Block of Na reabsorption causes more Na to be presented to the collecting duct. This results in 8 + + + greater Na /K exchange under the influence of aldosterone and thus greater K loss. In addition, Mg2+ excretion increases (the mechanism for this is not understood). The combined loss of K + and Mg2+ can sensitize the heart to the development of ventricular tachycardia and of another type of ventricular arrhythmia known as torsades de pointes. Either of these arrythmias can cause sudden cardiac death. Thiazide diuretics predispose to development of these arrhythmias predominantly by depleting cardiac muscle of K+. These drugs also lead to some degree of insulin resistance. Despite this, clinical studies demonstrate that thiazide diuretics are highly beneficial for individuals who suffer from both hypertension and Type 2 diabetes, especially when combined with an ACE inhibitor or ARB. Low dose therapy with a thiazide diuretic does not require consideration of K+ depletion, but therapy with higher doses does. Dietary supplementation does not often work with K+, possibly because few patients are sufficiently adherent to the necessary measures (e.g., eating a lot of bananas, drinking KCl solution, regular consumption of KCl tablets) and because increased aldosterone release counteracts the effect of K+ supplements. The only approach toward correcting the K+ imbalance that has been proved to prevent thiazide-induced sudden death is to combine the thiazide diuretic with a “K +-sparing diuretic” or an ACE inhibitor/ARB (which has K+-sparing activity due to reduced aldosterone production). A K+sparing diuretic may be preferred if blood pressure can be normalized with a thiazide diuretic/K +-sparing diuretic alone. Addition of an ACE inhibitor/ARB may be preferred if a greater reduction in blood pressure is required and/or the patient has some type of co-morbidity that requires treatment with an ACE inhibitor/ARB (e.g., congestive heart failure, diabetes, chronic renal insufficiency). Loop Diuretics (a.k.a. High-Ceiling Diuretics) Prototype: Furosemide Mechanism of action There are two components to the acute action of loop diuretics. These drugs inhibit NKCC2 in the thick ascending limb. Since between 20% and 40% of NaCl reabsorption takes place in this part of the nephron, a very impressive diuresis can be achieved. Urine volume can be increased by at least 8-fold. Loop diuretics also rapidly stimulate prostaglandin/NO synthesis by veins and some arteries. This leads to production and release of vasodilatory prostaglandins (PGE2, PGI2) and NO. Release of prostaglandin and NO increases venous capacitance, mildly reduces arterial pressure, and increases renal blood flow. In addition, it now appears that the sustained reduction in blood pressure produced by loop diuretics results from inhibition of NKCC1 in vascular smooth muscle. Clinical uses Loop diuretics are not often used to treat essential hypertension, because their short duration of action, steep dose-response curves, and large increase in urine volume make it difficult to achieve the desired antihypertensive effect. They are also no more effective as arterial vasodilators than thiazide diuretics. Thus their effects on systemic blood pressure over the long term are usually modest, no greater than that of thiazide diuretics. Nevertheless, loop diuretics do reduce blood pressure over the long term even when they are being used for a different purpose. As stated above, the drugs appear to do this by inhibiting NKCC1, the isoform of the Na/K/2Cl cotransporter expressed by vascular smooth muscle and many other cell types outside the kidney. Inhibition of NKCC1 reduces the intracellular Cl- concentration, hyperpolarizes the smooth muscle cells, and inhibits contraction in response to numerous stimuli. Loop diuretics are used predominantly in three clinical situations. First, furosemide is the drug of choice to treat acute decompensated congestive heart failure. It relieves this condition through two sequential actions. Furosemide (especially when administered intravenously) causes an almost immediate increase in vascular endothelial prostaglandin/NO synthesis and release of PGE2, PGI2, and NO. This effect occurs in veins, in the renal afferent arterioles, and in some other arterial beds more than in other vessels. Prostaglandin/NO release explains the acute increase in renal blood flow and systemic venous capacitance. The effect of the increase in venous capacitance is to reduce left ventricular filling pressure (preload) and to facilitate the return of edema fluid from the lungs to the circulation. This action provides immediate relief. Furosemide promotes diuresis with a slower time course. This action serves to eliminate the mobilized edema fluid from the body. Second, furosemide is 9 the diuretic most commonly used to relieve pulmonary and peripheral edema in chronic congestive heart failure. Its major role is to resolve the “congestion” (edema), thus improving respiration and reducing the preload on the heart. In this condition, furosemide is combined with other drugs, including an ACE inhibitor/ARB. Third, furosemide is used, along with an ACE inhibitor or ARB, to treat chronic renal insufficiency. Loop diuretics are the only diuretics that are generally useful for this purpose. This use relates to the large increase in urine volume and reduction in oxygen demand by the kidney. Problem: inability to regulate urine concentration Patients treated chronically with loop diuretics can neither dilute nor concentrate the urine. Recall that Na/K/2Cl cotransport in the absence of water reabsorption is the mechanism used by the kidney to dilute the urine. The same mechanism creates the extracellular hyperosmolarity needed to concentrate the urine by countercurrent exchange. The inability to excrete a dilute urine can result in “dilutional hyponatremia” (low plasma Na+ concentration due to inability to excrete excess water rapidly), especially in patients whose thirst mechanism causes them to drink more fluid than average. Dilutional hyponatremia leads to persistent generalized edema. Conversely, insufficient fluid intake will lead to dehydration and renal failure. Therefore the fluid intake of patients on chronic loop diuretic therapy must be strictly regulated. Problem: hypokalemia, hypomagnesemia, hypocalcemia Loop diuretics cause hypokalemia partly by increasing excretion in the same way as thiazide diuretics. However, the effect of loop diuretics on K+ excretion is greater, because even more Na+ is available for exchange with K+ in the collecting duct. Hypocalcemia occurs because loop diuretics lack the Ca2+-sparing activity of the thiazides and because they abolish the transepithelial electrical gradient in the thick ascending limb. However, increased reabsorption of Ca2+ in the distal tubule normally compensates for the lesser reabsorption in the thick ascending limb. Abolition of the transepithelial electrical gradient in the thick ascending limb can lead to hypomagnesemia. + These problems are addressed in the same manner as described for the thiazides: co-administration of a K 2+ 2+ sparing diuretic or ACE inhibitor/ARB plus dietary supplementation, if necessary, with Ca and Mg . Note that the major indications for use of a loop diuretic nearly always call for the use of an ACE inhibitor/ARB as well. Aldosterone Antagonist Prototypes: Spironolactone, Eplerenone + These drugs are classified as K -sparing diuretics. Spironolactone, its active metabolite canrenone, and eplerenone act as competitive antagonists at the mineralocorticoid receptor in the + + + early part of the collecting duct. Na reabsorption and K secretion are reduced. Because total Na excretion cannot be increased much by this mechanism, urine volume increases no more than 3-fold. There is a danger of hyperkalemia when these drugs are used alone. Aldosterone antagonists are not used primarily as diuretics. They have a unique clinical use in the treatment of hyperaldosteronism (elevated plasma concentration of aldosterone). Hyperaldosteronism occurs in a number of important clinical situations: e.g., hepatitis/cirrhosis and congestive heart failure (due to increased secretion and reduced elimination of aldosterone). Elevated plasma aldosterone plays a role in the development of arteriosclerosis, which is the pathological basis for hypertension. It is also involved in cardiac remodeling, which is the pathological basis for congestive heart failure. Spironolactone is not highly selective for the aldosterone receptor. It is a weak antagonist of the androgen receptor and a weak agonist of the progesterone receptor. Thus chronic use of spironolactone is often associated with gynecomastia and sexual dysfunction in men and with menstrual irregularities in women. To address this issue, the highly selective aldosterone receptor antagonist eplerenone was introduced. It is expected that this drug will eventually replace spironolactone. Spironolactone and eplerenone reduce mortality, reduce the number of hospitalizations, and improve functional status in persons with congestive heart failure. They also inhibit progression to congestive heart failure in persons who have had a myocardial infarction. These are important indications 10 for the use of aldosterone receptor antagonists. See handout on Pharmacotherapy of Congestive Heart Failure. Other Potassium-Sparing Diuretics Prototypes: Triamterene and Amiloride + These drugs block Na channels in the early part of the collecting duct. This action reduces + + Na reabsorption at that site. Lack of Na influx into the tubular epithelial cell removes the electrical + + + potential that drives the efflux of K . Therefore more Na and less K is excreted. Like spironolactone, the diuretic effect is small and there is a danger of hyperkalemia when a drug of this type is used alone. + Clinical uses as diuretics The K -sparing diuretics are seldom used alone; they are combined with + a thiazide or loop diuretic to prevent K loss. Their small diuretic action is additive to that of the principal diuretic agent. Triamterene is used most frequently, because it is better absorbed, acts more rapidly, and does not produce GI disturbances nearly so often as, for example, spironolactone. Fixed combinations of + thiazide or loop diuretic with a K -sparing diuretic are available, so that a patient can take just one preparation rather than two. 11