* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Steeper restitution slopes across right ventricular endocardium in
Coronary artery disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
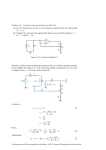
Am J Physiol Heart Circ Physiol 292: H1262–H1268, 2007. First published November 10, 2006; doi:10.1152/ajpheart.00913.2006. Translational Physiology Steeper restitution slopes across right ventricular endocardium in patients with cardiomyopathy at high risk of ventricular arrhythmias Raja J. Selvaraj, Peter Picton, Kumaraswamy Nanthakumar, and Vijay S. Chauhan Division of Cardiology, University Health Network and Mount Sinai Hospital, Toronto, Ontario, Canada Submitted 23 August 2006; accepted in final form 5 November 2006 of VF in humans, particularly those with left ventricular (LV) dysfunction, has not been substantiated. APD restitution properties may not be uniform throughout the heart. Recent modeling studies have suggested that spatial heterogeneity of APD restitution slopes can promote wavebreak and VF even in the absence of slopes ⬎1 (7). Laurita et al. (18, 19) demonstrated that APD restitution slopes vary throughout the guinea pig heart and restitution heterogeneity may be responsible for creating large repolarization gradients that promote reentrant ventricular arrhythmias including VF. In clinical studies involving patients with preserved ventricular function, restitution heterogeneity has also been demonstrated (22, 24, 32), but it is unclear whether this increases the propensity for ventricular arrhythmias. The purpose of this study was to test the hypothesis that steep APD restitution slopes and APD restitution slope heterogeneity contribute to ventricular arrhythmia vulnerability in patients with impaired LV function. To test this hypothesis, activation recovery interval (ARI) restitution slopes at multiple sites along the right ventricular (RV) endocardium were compared between cardiomyopathic patients considered to be at low risk and high risk of ventricular arrhythmias based on assessment of ventricular tachycardia (VT) inducibility and microvolt T wave alternans (TWA). MATERIALS AND METHODS a common cause of death in patients with cardiomyopathy. The underlying electrophysiological substrate that predisposes such patients to lethal ventricular arrhythmias is poorly understood. An important determinant of arrhythmia vulnerability is action potential duration (APD) restitution, which describes the relationship of APD to the preceding diastolic interval (DI). The restitution hypothesis states that a steep APD restitution relationship with slope ⬎1 can lead to ventricular fibrillation (VF) by creating unstable electrical oscillations, conduction block, and wavebreak (23, 25). This hypothesis has been supported by computational studies (12, 26). In animal studies, APD restitution slopes ⬎1 have been shown to potentiate VF, and antiarrhythmic drugs that flatten the restitution slope prevent or terminate VF (9, 27). The clinical relevance of APD restitution slope to the genesis Patients. Consecutive patients with cardiomyopathy, defined as an LV ejection fraction (LVEF) ⱕ40%, who were undergoing an invasive electrophysiology study for risk stratification were included in the study. LV function was assessed by gated blood pool nuclear imaging within 6 mo of enrollment. Patients with unstable angina or myocardial infarction within the past 3 mo, New York Heart Association class IV heart failure, uncontrolled hypertension, amiodarone therapy within the past 3 mo, or chronic atrial fibrillation were excluded. The study was approved by the Research Ethics Board of the University Health Network and Mount Sinai Hospital. All patients gave written, informed consent. Risk stratification. Risk stratification with invasive electrophysiological testing was performed in the nonsedated, postabsorptive state. Betablockers were held for five half-lives. Before 2004, risk stratification involved programmed ventricular stimulation to assess for inducible VT. Because of the limited sensitivity of this approach in nonischemic cardiomyopathy, only patients with ischemic cardiomyopathy were assessed for inducible VT. After 2004, TWA rather than VT induction was used for risk stratification in patients with both ischemic and nonischemic cardiomyopathy. Programmed stimulation was performed with a quadripolar catheter (Bard) placed in the RV apex. Pacing stimuli were delivered at twice diastolic threshold with a biostimulator (Bloom). The pacing protocol consisted of an eight-beat drive train at two different Address for reprint requests and other correspondence: V. S. Chauhan, PMCC 3-503, Toronto General Hospital, 150 Gerrard St. W., Toronto, ON, M5G 2C4 Canada (e-mail: [email protected]). The costs of publication of this article were defrayed in part by the payment of page charges. The article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact. sudden death; heart failure; ventricular fibrillation VENTRICULAR ARRHYTHMIAS ARE H1262 0363-6135/07 $8.00 Copyright © 2007 the American Physiological Society http://www.ajpheart.org Downloaded from http://ajpheart.physiology.org/ by 10.220.33.1 on August 1, 2017 Selvaraj RJ, Picton P, Nanthakumar K, Chauhan VS. Steeper restitution slopes across right ventricular endocardium in patients with cardiomyopathy at high risk of ventricular arrhythmias. Am J Physiol Heart Circ Physiol 292: H1262–H1268, 2007. First published November 10, 2006; doi:10.1152/ajpheart.00913.2006.—Steep action potential duration (APD) restitution slopes (⬎1) and spatial APD restitution heterogeneity provide the substrate for ventricular fibrillation in computational models and experimental studies. Their relationship to ventricular arrhythmia vulnerability in human cardiomyopathy has not been defined. Patients with cardiomyopathy [left ventricular (LV) ejection fraction ⬍40%] and no history of ventricular arrhythmias underwent risk stratification with programmed electrical stimulation or T wave alternans (TWA). Low-risk patients (n ⫽ 10) had no inducible ventricular tachycardia (VT) or negative TWA, while high-risk patients (n ⫽ 8) had inducible VT or positive TWA. Activation recovery interval (ARI) restitution slopes were measured simultaneously from 10 right ventricular (RV) endocardial sites during an S1-S2 pacing protocol. ARI restitution slope heterogeneity was defined as the coefficient of variation of slopes. Mean ARI restitution slope was significantly steeper in the high-risk group compared with the low-risk group [1.16 (SD 0.31) vs. 0.59 (SD 0.19), P ⫽ 0.0002]. The proportion of endocardial recording sites with a slope ⬎1 was significantly larger in the high-risk patients [47% (SD 35) vs. 13% (SD 21), P ⫽ 0.022]. Spatial heterogeneity of ARI restitution slopes was similar between the two groups [29% (SD 16) vs. 39% (SD 34), P ⫽ 0.48]. There was an inverse linear relationship between the ARI restitution slope and the minimum diastolic interval (P ⬍ 0.001). In cardiomyopathic patients at high risk of ventricular arrhythmias, ARI restitution slopes along the RV endocardium are steeper, but restitution slope heterogeneity is similar compared with those at low risk. Steeper ARI restitution slopes may increase the propensity for ventricular arrhythmias in patients with impaired left ventricular function. Translational Physiology RESTITUTION SLOPES IN HUMAN CARDIOMYOPATHY Table 1. Patient characteristics Patient Age, yr Male LVEF, % Ischemic EP Study Low risk 1 2 3 4 5 6 7 8 9 10 69 61 58 67 70 72 51 40 51 58 60 (10) Yes Yes Yes Yes Yes Yes Yes No Yes Yes 9 (90%) 40 32 25 26 15 35 40 32 20 24 29 (8) Yes Yes Yes Yes No Yes No No No Yes 6 (60%) ⫺VT ⫺VT ⫺VT ⫺VT ⫺TWA ⫺TWA ⫺TWA ⫺TWA ⫺TWA ⫺TWA High risk 1 2 3 4 5 6 7 8 63 48 57 55 64 62 50 32 54 (11)* Yes Yes Yes No Yes Yes Yes Yes 7 (86%)* 25 22 34 39 22 40 24 40 31 (8)* Yes Yes Yes Yes Yes No Yes No 6 (75%)* ⫹VT ⫹VT ⫹VT ⫹VT ⫹TWA ⫹TWA ⫹TWA ⫹TWA Individual and mean (SD) values are shown. ⫹VT, ⫽ inducible ventricular tachycardia (VT); ⫺VT, noninducible VT; ⫹TWA ⫽ positive T wave alternans; ⫺TWA ⫽ negative T wave alternans; LVEF, left ventricular ejection fraction; EP, electrophysiology. *P ⫽ not significant (vs. low-risk group). cycle lengths (CLs; 600 and 400 ms) followed by up to three ventricular extrastimuli delivered at progressively premature coupling intervals down to 200 ms, or until ventricular refractoriness was reached. Inducible VT was defined as sustained monomorphic VT (⬎30 s) with up to three extrastimuli or sustained polymorphic VT/VF induced with up to two extrastimuli. TWA was assessed during right atrial pacing at a heart rate of 110 beats per minute (bpm) for 5 min. Careful skin preparation with mild abrasion and the use of high-resolution electrodes (High-Res, Cambridge Heart) minimized noise. Electrocardiographic leads were placed in the standard 12-lead configuration in addition to an orthogonal X, Y, and Z configuration. TWA was measured with the Heartwave system (Cambridge Heart), which utilizes a spectral method designed to quantify TWA in the microvolt range. The Heartwave system automatically classifies TWA as positive or negative as follows. Positive TWA is defined as alternans voltage ⱖ1.9 V and an alternans ratio ⱖ3 at a heart rate ⱕ110 bpm for at least 1 min in any of the vector magnitude, X, Y, or Z leads, or in two adjacent precordial leads in the absence of significant artifact (3). TWA is considered negative in the absence of these criteria at a heart rate ⱕ110 bpm (3). Patients were classified as high risk for ventricular arrhythmias if they had inducible VT or a positive TWA. In the absence of inducible VT or negative TWA, patients were considered to be low risk for ventricular arrhythmias (2, 4 – 6). Endocardial recordings and ARI restitution protocol. Unipolar electrograms were recorded simultaneously from 10 distinct sites along the anteroseptal RV endocardium from apex to base with a decapolar catheter (Livewire, Daig). The catheter consists of five electrode pairs with an interelectrode distance of 2 mm, and each electrode pair is separated by a distance of 5 mm. Unipolar electrograms were filtered at 0.05–500 Hz and recorded on a Prucka workstation (GE Medical Systems) at a sampling rate of 1,000 Hz. ARI restitution was assessed with an S1-S2 pacing protocol using a quadripolar catheter (Biosense) positioned in the RV apex in close proximity to the apical electrodes of the decapolar catheter. A 2-min conditioning period of constant ventricular pacing at a CL of 500 ms preceded ventricular extrastimulus testing. S2 was introduced after a 10-beat drive train at a CL of 500 ms. The coupling interval of S2 was AJP-Heart Circ Physiol • VOL decreased in steps of 50 ms from 500 to 400 ms and subsequently in steps of 20 ms down to 300 ms. Decrements of 5 ms were used below 300 ms until ventricular refractoriness or an S1-S2 coupling interval of 200 ms. ARI measurement. ARI of the unipolar electrogram was used as an estimate of the APD (10). ARI was defined as the interval between the local activation time and recovery time of the unipolar electrogram. Activation time was defined as the minimum temporal derivative of voltage (dV/dt) of the unipolar QRS complex. Recovery time was defined as the minimum dV/dt for a positive T wave and the maximum dV/dt for a negative T wave (modified Wyatt method). ARI measurement by this method has been shown to correlate better with monophasic action potential duration at 90% repolarization than ARI measured by the standard Wyatt method (33). Activation and recovery times were determined automatically and manually verified with custom interactive software written in Matlab (Matlab 6.5, The Mathworks). Recovery time measurements were excluded if flat T waves with indistinct slopes were present. The DI between S1 and S2 was defined as the interval from the recovery time of the S1 unipolar electrogram to the activation time of the succeeding S2 unipolar electrogram. ARI restitution analysis. An ARI restitution curve at each endocardial recording site was obtained by plotting the ARI of each S2 as a function of the preceding DI. At shorter S1-S2 coupling intervals, DI cannot be directly measured because the S2 extrastimulus obscures assessment of the S1 ARI. In these instances, the ARI of the preceding S1 in the drive train rather than the last S1 was used to calculate DI. In five randomly selected patients, automated ARI measurements of the last two S1s of the drive train were compared from three drives with long S1-S2 coupling intervals that permitted accurate measurement of ARI. Difference in these measurements provided an estimate of the error arising from deriving the DI based on the ARI of the penultimate beat of the drive. For each ARI restitution curve, the slopes of least-squares linear fits to overlapping 40-ms segments of Fig. 1. A: unipolar electrograms (EGM) recorded from right ventricular (RV) endocardial electrode 2 during S1-S2 restitution pacing protocol. The S1-S2 coupling interval is indicated on left. The electrograms are aligned by their activation time (vertical line). The recovery time is indicated by an X, and the activation recovery interval (ARI) for each S1-S2 is shown at right of the electrogram. B: 1st derivative of the corresponding unipolar electrogram voltage shown in A is used to define local activation time and recovery time. The waveforms are aligned by their activation time (vertical line). The recovery time is indicated by an X. 292 • MARCH 2007 • www.ajpheart.org Downloaded from http://ajpheart.physiology.org/ by 10.220.33.1 on August 1, 2017 Group H1263 Translational Physiology H1264 RESTITUTION SLOPES IN HUMAN CARDIOMYOPATHY RESULTS Patients. A total of 24 patients completed the study. Three patients were excluded because ventricular ectopic beats after the extrastimulus at shorter S1-S2 coupling intervals precluded ARI measurement of S2. Another three patients were excluded because multiple recording sites manifested flat or ambiguous unipolar T waves that made ARI measurement unreliable. The remaining 18 patients formed the study group, of which 10 were classified as low risk and 8 were classified as high risk. Among the low-risk patients, four patients had no inducible VT and six had negative TWA. In the high-risk group, four patients had inducible VT and another four had positive TWA. The baseline characteristics of these patients are shown in Table 1. There were no differences in age, LVEF, or proportion with ischemic/nonischemic cardiomyopathy between the two groups. All patients with ischemic cardiomyopathy had a prior myocardial infarction (⬎3 mo). ARI measurement. Figure 1 illustrates unipolar electrograms recorded from electrode 2 along the apical RV endocardium in a low-risk patient during various S1-S2 coupling intervals. In this example, the ARI of the S2, derived from automated activation and recovery time measurements, decreases with shorter S1-S2 coupling intervals. The ARI measured after 2 min of preconditioning pacing at CL 500 ms was 291 (SD 19) ms in the low-risk group and 284 (SD 19) ms in the high-risk group (P ⫽ 0.98). The difference in ARI between the last two beats of the drive train by the automated algorithm in the 15 random paired ARI measurements was 3.9 (SD 3.7) ms. Thus the error in deriving the DI based on the ARI of the penultimate beat of the drive was negligible. ARI restitution slopes. Figure 2 shows ARI restitution curves at three different RV endocardial recording sites in a low-risk and a high-risk patient. The ARI restitution slope at each recording site is illustrated in this figure. The mean slope of the ARI restitution curves from the 10 endocardial recording sites was larger in the high-risk group than in the low-risk group [1.16 (SD 0.31) vs. 0.59 (SD 0.19), P ⬍ 0.001] (Fig. 3). The maximum slope and the proportion of recording sites with a Fig. 2. ARI restitution curves in a high-risk (top) and a low-risk (bottom) patient. For each patient, the restitution curves at 1 apical, 1 midendocardial, and 1 basal endocardial electrode are shown. The linear fit to the 40-ms diastolic interval with the maximum slope is shown. The number adjacent to the curve denotes the maximum slope. APD, action potential duration; DI, diastolic interval. AJP-Heart Circ Physiol • VOL 292 • MARCH 2007 • www.ajpheart.org Downloaded from http://ajpheart.physiology.org/ by 10.220.33.1 on August 1, 2017 the DI were determined (28). The maximum slope obtained over any 40-ms segment was used to define the slope of the restitution curve. This method is considered to be more robust than monoexponential curve fitting for tracking restitution slopes independently over a wide range of DIs (28). For each patient, spatial heterogeneity of restitution slopes was determined by using the range (maximum slope–minimum slope) and the coefficient of variation among the 10 endocardial recording sites. Statistical analysis. Continuous data are presented as means (SD). Continuous variables were compared between groups with an unpaired t-test. The paired t-test was used for comparisons within groups. Categorical variables were compared with the 2-test. The Pearson correlation coefficient was calculated for linear correlation analysis between two continuous variables. A two-tailed P value ⬍0.05 was considered statistically significant. All statistical analyses were performed with SPSS software (SPSS for Windows, Release 10). Translational Physiology H1265 RESTITUTION SLOPES IN HUMAN CARDIOMYOPATHY Table 2. ARI restitution slopes Mean slope Maximum slope Proportion of recording sites with slope ⬎1, % Range of slopes Coefficient of variation of slopes, % Low Risk (n ⫽ 10) High Risk (n ⫽ 8) P Value 0.59 (0.19) 0.93 (0.29) 1.16 (0.31) 1.73 (0.61) 0.0002 0.002 13 (21) 0.59 (0.35) 39 (34) 47 (35) 0.98 (0.67) 29 (16) 0.022 0.14 0.48 Values are means (SD). ARI, activation recovery interval. function of minimum DI for all endocardial sites in all patients revealed a significant inverse linear relationship (r ⫽ ⫺0.57, P ⬍ 0.001) with a slope of ⫺0.017 ms⫺1 (Fig. 5). The minimum DI at the RV pacing site is equal to the difference between the effective refractory period (ERP) and the APD at that site. The relationship between ERP and APD, expressed as the ERP-to-APD ratio, provides a measure of arrhythmia vulnerability, and a smaller ERP/APD has been associated with VT inducibility (15). We estimated ERP/APD in our study patients by substituting the ARI at the recording electrode closest to the RV pacing site for the APD at the pacing site, since the latter was not directly measured. The closest electrode to the pacing site was defined as the one with the shortest activation time. ERP/ARI was significantly smaller in the high-risk patients compared with the low-risk patients [0.78 (SD 0.07) vs. 0.84 (SD 0.04), P ⫽ 0.019]. DISCUSSION Fig. 3. Scattergram of the mean and maximum ARI restitution slope in the low-risk and high-risk groups. Mean and SD are plotted at left of the data points. AJP-Heart Circ Physiol • VOL The major finding of our study is that the ARI restitution slope is steeper in patients with cardiomyopathy at high risk of ventricular arrhythmias compared with those at low risk. Highrisk patients had a greater proportion of endocardial sites with a slope ⬎1. There was no difference in the spatial heterogeneity of ARI restitution slopes between the two groups. We observed an inverse linear relationship between the ARI restitution slope and the minimum DI. Ventricular arrhythmia risk in cardiomyopathy. Patients with impaired LV function are at an increased risk of sudden death due in the majority of cases to VT degenerating into VF (11). Identifying patients with cardiomyopathy at high risk of potentially lethal ventricular arrhythmias, who will derive survival benefit from prophylactic implantable cardioverterdefibrillator implantation, has primarily involved measurement of ventricular function (1, 21). Contemporary risk stratification algorithms also include assessment of VT inducibility and microvolt TWA. In patients with LVEF ⬍40%, the absence of VT inducibility (5) or negative microvolt TWA (2, 4, 6) has a high negative predictive value for nonfatal ventricular arrhythmias and death. Therefore, we used VT inducibility and TWA to classify our low- and high-risk patients. Restitution slopes and arrhythmogenesis. The electrophysiological substrate in patients with cardiomyopathy, particularly those deemed to be at high risk of ventricular arrhythmias, has not been well described. In computational models and experimental studies, the steepness of the restitution curve is critical to the stability of spiral wave reentry. A restitution slope equal to 1 can lead to persistent APD alternans around the restitution curve after an abrupt increase in pacing rate that models the onset of rapid clinical VT. If the restitution slope is ⬎1 and the 292 • MARCH 2007 • www.ajpheart.org Downloaded from http://ajpheart.physiology.org/ by 10.220.33.1 on August 1, 2017 slope ⬎1 were also significantly larger in the high-risk group (Table 2). In subgroup analysis, patients with inducible VT had steeper ARI restitution slopes than those without inducible VT. Similarly, when the subgroup of patients who underwent TWA was considered, those with positive TWA had steeper ARI restitution slopes than those with negative TWA (Table 3). ARI restitution slope heterogeneity. The dispersion of ARI restitution slopes across the 10 apicobasal recording sites was not significantly different between the high- and low-risk groups when assessed with range and the coefficient of variation (Table 2). ARI restitution slopes exhibited an apicobasal gradient such that the apical slopes were steeper than the basal slopes (Fig. 4). This was evident in both low-risk and high-risk patients. The mean slope in the three apical electrodes (electrodes 1–3) was larger than the mean slope in the three basal electrodes (electrodes 8 –10) for all patients [1.05 (SD 0.49) vs. 0.71 (SD 0.43), P ⫽ 0.005]. Minimum DI. We investigated the relationship of the ARI restitution slope with the minimum DI to ascertain whether the difference in ARI restitution slopes between 1) the high- and low-risk patients and 2) the apex and base were related to differences in the minimum DI. The average minimum DI across the 10 endocardial sites was significantly shorter in the high-risk group compared with the low-risk group [⫺22 (SD 14) vs. ⫺7 (SD 12) ms, P ⫽ 0.035]. The average minimum DI in the three apical electrodes was smaller than the average minimum DI of the three basal electrodes [⫺18 (SD 14) vs. ⫺9 (SD 15) ms, P ⫽ 0.001]. A plot of ARI restitution slope as a Translational Physiology H1266 RESTITUTION SLOPES IN HUMAN CARDIOMYOPATHY Table 3. ARI restitution slope subgroup analysis VT Induction Mean slope Maximum slope Range of slopes Coefficient of variation of slopes, % TWA ⫺VT (n ⫽ 4) ⫹VT (n ⫽ 4) P Value ⫺TWA (n ⫽ 6) ⫹TWA (n ⫽ 4) P Value 0.67⫾0.25 0.97⫾0.37 0.57⫾0.29 30⫾11 1.38⫾0.31 1.76⫾0.47 0.83⫾0.37 21⫾9 0.022 0.039 0.3 0.25 0.54⫾0.14 0.91⫾0.27 0.62⫾0.41 45⫾44 1.04⫾0.29 1.71⫾0.81 1.12⫾0.92 37⫾21 0.006 0.05 0.26 0.76 Values are means (SD). Fig. 4. Mean ARI restitution slope at each endocardial recording electrode plotted for the low-risk and high-risk groups. Endocardial electrodes 1–10 have been positioned from the apex to base, respectively. There is an apicobasal gradient of ARI restitution slope in both groups. The restitution slope at each recording electrode is significantly larger in the high-risk group than in the low-risk group. *P ⬍ 0.05, †P ⬍ 0.005 (high vs. low risk). AJP-Heart Circ Physiol • VOL regional differences in slope could cause wavebreak even in the absence of a slope ⬎1 at any site. In our study, an apical-to-basal gradient of restitution slopes was present in both high- and low-risk patients, with slopes being steeper at the apex. However, the spatial dispersion of ARI restitution slopes among the 10 endocardial sites was not significantly different between the two groups. These findings imply that spatial heterogeneity of restitution slopes may be less relevant than the steepness of restitution slopes in defining the substrate for arrhythmogenesis in patients with cardiomyopathy. However, the two may act synergistically, as suggested in computational studies. Xie et al. (30) showed that a steep APD restitution slope can reduce the degree of APD restitution slope heterogeneity required to produce wavebreak. Thus increased spatial dispersion of slopes may have a role in arrhythmogenesis by promoting initial wavebreak and by potentiating the proarrhythmic effect of a steep APD restitution slope. Restitution slope and minimum diastolic interval: Is there a link? We found a significant inverse linear relationship between the ARI restitution slope and the minimum DI such that endocardial sites with shorter minimum DIs also had steeper ARI restitution slopes. With a longer minimum DI, the initial segment of the restitution curve, which is usually steepest, is curtailed, resulting in a shallower restitution slope (14). This relationship may account for the steeper ARI restitution slopes in the high-risk patients in whom the minimum DI was shorter. Furthermore, the shorter DI at apical sites may contribute to Fig. 5. Plot of the ARI restitution slope as a function of the minimum DI for each recording electrode. Regression line is included, showing a significant linear relationship. 292 • MARCH 2007 • www.ajpheart.org Downloaded from http://ajpheart.physiology.org/ by 10.220.33.1 on August 1, 2017 rate of pacing or VT does not change, the magnitude of APD alternans will iteratively increase with each beat, accompanied by shortening in the proceeding DI until local refractoriness is reached. At this point, conduction block, wavebreak, and fibrillation can develop, and this may account for the transition of VT into VF in some patients (13, 23, 31). In our study, the mean ARI restitution slope in the high-risk patients was ⬎1, and 47% of endocardial sites had a slope ⬎1. In contrast, the low-risk patients had a mean ARI restitution slope that was ⬍1, and fewer (13%) endocardial sites had a slope ⬎1. Every high-risk patient had a slope ⬎1 in at least one endocardial site, while 6 of the 10 patients in the low-risk group did not have a slope ⬎1 at any site. These findings suggest that increased spatial distribution of steep ARI restitution slopes (⬎1) in the human heart may provide the substrate for ventricular arrhythmias by promoting greater dynamic repolarization instability and wavebreak, thereby ensuring that VF does not extinguish once initiated. Experimental studies have shown that a critical mass of tissue is required to sustain VF, and the functional size of this tissue may be governed by the spatial distribution of steep APD restitution slopes (29). Spatial heterogeneity of restitution slopes. The spatial heterogeneity of the APD restitution slope may be important in the genesis of VF even in the absence of a steep APD restitution slope (7, 22). Nash et al. (22) showed in a computer model that Translational Physiology RESTITUTION SLOPES IN HUMAN CARDIOMYOPATHY AJP-Heart Circ Physiol • VOL in mean APD restitution slopes between the two groups (0.91 vs. 0.83). The reported slopes, derived from overlapping linear segments, cannot be compared with our study because the patients differ substantially with respect to mean LVEF and arrhythmia risk. Limitations. A limited area in the RV endocardium was sampled with a single multielectrode catheter. The technical constraints of this approach and ethical considerations precluded more detailed sampling in the RV or LV. Higherresolution spatial mapping of ARI restitution is possible with reconstructed unipolar electrograms from noncontact balloon arrays (32), but this approach has limited applicability in assessing high- vs. low-risk cardiomyopathic patients in whom VT mapping is not clinically indicated. Second, the ERP-toAPD ratio was approximated by using the ARI of the recording electrode in closest proximity to the pacing site. This assumed that the ARI was similar to the APD at the pacing site, which is reasonable since the pacing catheter was positioned in the RV apex in close proximity to the distal electrode of the recording catheter. Third, VT inducibility and TWA provided a surrogate measure of ventricular arrhythmia risk. Clinical events were not used to define high vs. low risk. Confirmation of these results will require a prospective study with a considerably larger patient population and predefined clinical end points. In conclusion, ARI restitution slopes along the RV endocardium are steeper in cardiomyopathic patients at high risk of ventricular arrhythmias compared with those at low risk. In contrast, spatial ARI restitution heterogeneity does not differ between these groups. These findings suggest that steep ARI restitution kinetics rather than ARI restitution heterogeneity may increase the propensity for ventricular arrhythmias in patients with impaired LV function. ACKNOWLEDGMENTS We thank the nursing staff of the Clinical Cardiovascular Research Laboratory for help in the completion of these studies. GRANTS This study was supported by the Heart and Stroke Foundation of Canada (T5381) and the Canadian Foundation for Innovation (7498, V. Chauhan). REFERENCES 1. Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, Clapp-Channing N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip JH, Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverterdefibrillator for congestive heart failure. N Engl J Med 352: 225–237, 2005. 2. Bloomfield DM, Bigger JT, Steinman RC, Namerow PB, Parides MK, Curtis AB, Kaufman ES, Davidenko JM, Shinn TS, Fontaine JM. Microvolt T-wave alternans and the risk of death or sustained ventricular arrhythmias in patients with left ventricular dysfunction. J Am Coll Cardiol 47: 456 – 463, 2006. 3. Bloomfield DM, Hohnloser SH, Cohen RJ. Interpretation and classification of microvolt T wave alternans tests. J Cardiovasc Electrophysiol 13: 502–512, 2002. 4. Bloomfield DM, Steinman RC, Namerow PB, Parides M, Davidenko J, Kaufman ES, Shinn T, Curtis A, Fontaine J, Holmes D, Russo A, Tang C, Bigger JT Jr. Microvolt T-wave alternans distinguishes between patients likely and patients not likely to benefit from implanted cardiac defibrillator therapy: a solution to the Multicenter Automatic Defibrillator Implantation Trial (MADIT) II conundrum. Circulation 110: 1885–1889, 2004. 292 • MARCH 2007 • www.ajpheart.org Downloaded from http://ajpheart.physiology.org/ by 10.220.33.1 on August 1, 2017 steeper ARI restitution slopes. Kuo et al. (17) showed that recording sites remote from the site of pacing exhibited a longer minimum DI during ventricular extrastimulus testing due to longer activation times compared with more proximal recording sites. This would explain the longer minimum DI at basal sites compared with apical sites in our patients during RV apical pacing. The relationship between restitution slope and DI has not been previously reported in humans and should be considered in clinical studies evaluating restitution kinetics. The minimum DI is dependent on ERP and APD. The ERP-to-APD ratio was significantly smaller in our high-risk patients. ERP/APD is known to be constant over a range of CL in both animals and humans (8, 20). However, it can decrease during repetitive extrastimulation, leading to ventricular arrhythmia induction (14, 15). Smaller ERP/APD ratios allow myocardial stimulation within the vulnerable window of the action potential, which can result in localized conduction slowing and reentrant ventricular arrhythmias. In contrast, larger ERP/APD may be antiarrhythmic, as evident during amiodarone therapy (14). It is important to note that although smaller minimum DI and ERP/APD are associated with steeper restitution slopes, they can have independent effects on VF induction. For instance, a critically timed premature ventricular beat may induce stable reentrant VT in the face of smaller ERP/APD, but a steeper restitution slope may cause this VT to degenerate into lethal VF. Previous studies. There are no published data on APD restitution slopes in high-risk patients with LV systolic dysfunction (LVEF ⬍40%) from which to draw direct comparisons with our study. However, four reports have described APD restitution slopes in patients with relatively preserved ventricular function. Nash et al. (22) measured ARI restitution slopes from 256 sites on the epicardium in patients with preserved ventricular function undergoing cardiac surgery. No patient had a history of VT, and VT inducibility was not assessed. The mean ARI restitution slope was 1.1 (range 0 –5.6), and spatial heterogeneity in ARI restitution was observed with slopes ⬎1 in 45% of recordings sites. No apicobasal ARI restitution gradients were reported. The preponderance of steeper slopes in this population compared with our study may be due to epicardial recordings and methodological differences in calculating ARI restitution slopes that involved monoexponential curve fitting of ARI measurements derived by the Wyatt method. In contrast, Yue et al. (32) measured ARI restitution slopes from 16 endocardial sites, using overlapping linear segments similar to our study. Recordings were made after idiopathic VT ablation, and no patient had structural heart disease. The mean ARI restitution slope was 0.65 in the RV, and 25% of recording sites had a slope ⬎1, which is comparable to our low-risk patients with cardiomyopathy. Pak et al. (24) compared APD restitution slopes from two RV endocardial sites in patients with inducible vs. noninducible VT, but these patients all had a clinical history of VT with preserved ventricular function. This may account for the lack of a significant difference in mean APD restitution slopes between the two groups (VT inducible: 2.3, VT noninducible: 1.8). The APD restitution slopes reported were larger than those in our patients, possibly because of methodological differences in deriving slopes from monoexponential curve fitting. Similarly, Koller et al. (16) compared APD restitution slopes from a single RV endocardial site in patients with and without structural heart disease, but the mean LVEF was ⬎40% in both groups. This may explain the similarity H1267 Translational Physiology H1268 RESTITUTION SLOPES IN HUMAN CARDIOMYOPATHY AJP-Heart Circ Physiol • VOL 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. repolarization kinetics demonstrated by optical mapping of the intact guinea pig heart. Circ Res 79: 493–503, 1996. Lee RJ, Liem LB, Cohen TJ, Franz MR. Relation between repolarization and refractoriness in the human ventricle: cycle length dependence and effect of procainamide. J Am Coll Cardiol 19: 614 – 618, 1992. Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, Daubert JP, Higgins SL, Brown MW, Andrews ML, Multicenter Automatic Defibrillator Implantation Trial II Investigators. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 346: 877– 883, 2002. Nash MP, Bradley CP, Sutton PM, Clayton RH, Kallis P, Hayward MP, Paterson DJ, Taggart P. Whole heart APD restitution properties in cardiac patients: a combined clinical and modelling study. Exp Physiol 91: 339 –354, 2006. Nolasco JB, Dahlen RW. A graphic method for the study of alternation in cardiac action potentials. J Appl Physiol 25: 191–196, 1968. Pak HN, Hong SJ, Hwang GS, Lee HS, Park SW, Ahn JC, Moo Ro Y, Kim YH. Spatial dispersion of action potential duration restitution kinetics is associated with induction of ventricular tachycardia/fibrillation in humans. J Cardiovasc Electrophysiol 15: 1357–1363, 2004. Pastore JM, Girouard SD, Laurita KR, Akar FG, Rosenbaum DS. Mechanism linking T-wave alternans to the genesis of cardiac fibrillation. Circulation 99: 1385–1394, 1999. Qu Z, Weiss JN, Garfinkel A. Cardiac electrical restitution properties and stability of reentrant spiral waves: a simulation study. Am J Physiol Heart Circ Physiol 276: H269 –H283, 1999. Riccio ML, Koller ML, Gilmour RF Jr. Electrical restitution and spatiotemporal organization during ventricular fibrillation. Circ Res 84: 955–963, 1999. Taggart P, Sutton P, Chalabi Z, Boyett MR, Simon R, Elliott D, Gill JS. Effect of adrenergic stimulation on action potential duration restitution in humans. Circulation 107: 285–289, 2003. Wu TJ, Yashima M, Doshi R, Kim YH, Athill CA, Ong JJ, Czer L, Trento A, Blanche C, Kass RM, Garfinkel A, Weiss JN, Fishbein MC, Karagueuzian HS, Chen PS. Relation between cellular repolarization characteristics and critical mass for human ventricular fibrillation. J Cardiovasc Electrophysiol 10: 1077–1086, 1999. Xie F, Qu Z, Garfinkel A, Weiss JN. Electrophysiological heterogeneity and stability of reentry in simulated cardiac tissue. Am J Physiol Heart Circ Physiol 280: H535–H545, 2001. Xie F, Qu Z, Yang J, Baher A, Weiss JN, Garfinkel A. A simulation study of the effects of cardiac anatomy in ventricular fibrillation. J Clin Invest 113: 686 – 693, 2004. Yue AM, Franz MR, Roberts PR, Morgan JM. Global endocardial electrical restitution in human right and left ventricles determined by noncontact mapping. J Am Coll Cardiol 46: 1067–1075, 2005. Yue AM, Paisey JR, Robinson S, Betts TR, Roberts PR, Morgan JM. Determination of human ventricular repolarization by noncontact mapping: validation with monophasic action potential recordings. Circulation 110: 1343–1350, 2004. 292 • MARCH 2007 • www.ajpheart.org Downloaded from http://ajpheart.physiology.org/ by 10.220.33.1 on August 1, 2017 5. Buxton AE, Lee KL, DiCarlo L, Gold MR, Greer GS, Prystowsky EN, O’Toole MF, Tang A, Fisher JD, Coromilas J, Talajic M, Hafley G. Electrophysiologic testing to identify patients with coronary artery disease who are at risk for sudden death. Multicenter Unsustained Tachycardia Trial Investigators. N Engl J Med 342: 1937–1945, 2000. 6. Chow T, Kereiakes DJ, Bartone C, Booth T, Schloss EJ, Waller T, Chung ES, Menon S, Nallamothu BK, Chan PS. Prognostic utility of microvolt T-wave alternans in risk stratification of patients with ischemic cardiomyopathy. J Am Coll Cardiol 47: 1820 –1827, 2006. 7. Clayton RH, Taggart P. Regional differences in APD restitution can initiate wavebreak and re-entry in cardiac tissue: a computational study. Biomed Eng Online 4: 54, 2005. 8. Franz MR, Chin MC, Sharkey HR, Griffin JC, Scheinman MM. A new single catheter technique for simultaneous measurement of action potential duration and refractory period in vivo. J Am Coll Cardiol 16: 878 – 886, 1990. 9. Garfinkel A, Kim YH, Voroshilovsky O, Qu Z, Kil JR, Lee MH, Karagueuzian HS, Weiss JN, Chen PS. Preventing ventricular fibrillation by flattening cardiac restitution. Proc Natl Acad Sci USA 97: 6061– 6066, 2000. 10. Haws CW, Lux RL. Correlation between in vivo transmembrane action potential durations and activation-recovery intervals from electrograms. Effects of interventions that alter repolarization time. Circulation 81: 281–288, 1990. 11. Kannel WB, Plehn JF, Cupples LA. Cardiac failure and sudden death in the Framingham Study. Am Heart J 115: 869 – 875, 1988. 12. Karma A. Electrical alternans and spiral wave breakup in cardiac tissue. Chaos 4: 461– 472, 1994. 13. Karma A. Spiral breakup in model equations of action potential propagation in cardiac tissue. Phys Rev Lett 71: 1103–1106, 1993. 14. Kirchhof P, Degen H, Franz MR, Eckardt L, Fabritz L, Milberg P, Laer S, Neumann J, Breithardt G, Haverkamp W. Amiodaroneinduced postrepolarization refractoriness suppresses induction of ventricular fibrillation. J Pharmacol Exp Ther 305: 257–263, 2003. 15. Koller BS, Karasik PE, Solomon AJ, Franz MR. Relation between repolarization and refractoriness during programmed electrical stimulation in the human right ventricle. Implications for ventricular tachycardia induction. Circulation 91: 2378 –2384, 1995. 16. Koller ML, Maier SK, Gelzer AR, Bauer WR, Meesmann M, Gilmour RF Jr. Altered dynamics of action potential restitution and alternans in humans with structural heart disease. Circulation 112: 1542–1548, 2005. 17. Kuo CS, Atarashi H, Reddy CP, Surawicz B. Dispersion of ventricular repolarization and arrhythmia: study of two consecutive ventricular premature complexes. Circulation 72: 370 –376, 1985. 18. Laurita KR, Girouard SD, Akar FG, Rosenbaum DS. Modulated dispersion explains changes in arrhythmia vulnerability during premature stimulation of the heart. Circulation 98: 2774 –2780, 1998. 19. Laurita KR, Girouard SD, Rosenbaum DS. Modulation of ventricular repolarization by a premature stimulus. Role of epicardial dispersion of