* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The sick child and common presentations
Survey
Document related concepts
Cryptosporidiosis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Gastroenteritis wikipedia , lookup
Sarcocystis wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Herpes simplex virus wikipedia , lookup
Hepatitis C wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Leptospirosis wikipedia , lookup
Trichinosis wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Oesophagostomum wikipedia , lookup
Schistosomiasis wikipedia , lookup
Hepatitis B wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Transcript
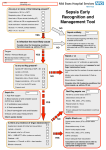
Recognising the sick child and common paediatric presentations Natasha Hawkins GP Learning objectives Recognising sepsis, traffic light system and cases UTI in children. CMPI and lactose intolerance. Nocturnal enuresis. Spotting sepsis in the sick child Re-ACT Talks: Spotting Sepsis in the Sick Child (3 min video) NHS England. Red Flags (The Sepsis Trust leaflet) Traffic Light system refresher. IF YOUR CHILD HAS: AMBER symptoms www.sepsistrust.org www.sepsistrust.org This information is derived, with permission, from the SAM leaflet produced by NHS England (South West) to improve recognition of sepsis in children. Contributors include paediatricians, sepsis experts, nurses, GPs and parents of children who’ve had sepsis. Spotting sepsis in children The UK Sepsis Trust is here to support you. ASK FOR MEDICAL ADVICE www.sepsistrust.org Protect your child’s health. Think sepsis. RED symptoms GET YOUR CHILD TO HOSPITAL QUICKLY Dial 999 for an ambulance if necessary This information relates to the law and procedures in England and Wales. All information included within this booklet is correct at time of print, June 20 16. The UK Sepsis Trust registered charity number (England & Wales) 1158843. Company registration number 8644039. Sepsis Enterprise company number 9583335. VAT reg number 225570222. Kind thanks to 11-London for the design of this leaflet – we hope you found it helpful. Photography by AminArt. www .aminart.co.uk Red Flags Temperature. Breathing. Skin, lips, tongue Eating and drinking Nappies Activity. See Handout. Traffic Light Sytem Common viral illnesses Duration of symptoms of RTI in children-resolution of symptoms Acute Otitis Media: 50% by day 3, 90% by day 7-8 Common cold: 50% by day 7-8, 80% by day 14. Cough: 50% by day 10, 90% by day 25. Croup: 50% by day 1, 80% by day 2 Bronchiolitis: 50% by day 13, 90% by day 21. BMJ 2013: 347:f7027 Case 1 5 month old 2/7 history of runny nose, snuffly, noisy breathing ‘Think she’s got a chest infection’ What do you want to know? What would be your diagnosis and management? Bronchiolitis Affects 1 in 3 children by the age of 1. Infectious disease of the lower respiratory tract. Usually viral (RSV) Most commonly 3-6 months. Fever >39 is unusual (consider bacterial) NICE recommend safety netting information for parents to take away. Particularly as may get worse before get better. -(Patient.co.uk, NHS choices) When to refer Poor feeding (<50% usual intake over the previous 24 hours) which is inadequate to maintain hydration Lethargy History of apnoea Signs of respiratory distress Sats <94% Where home care or rapid review cannot be assured Case 2 3 year old with noisy breathing last 2 days. Snuffly, well in herself ‘Thinks has a chest infection’ What do you want to know? What is your diagnosis and management? Viral Induced wheeze Wheeze- high pitched whistling sound usually on expiration. 6months-5 years. Viral wheeze is a similar but different condition from asthma, but some children will go onto develop asthma as they get older. Children with asthma can get wheezy even when they do not have a cough or cold. Children with asthma are often wheezy when they do lots of exercise. Children with asthma usually have a family history of asthma and allergy. If none of these apply to your child it is unlikely they will go on to develop asthma. Only recommend treatment in acute episode. 2-10 puffs up to 4 hourly. Managing wheeze in preschool children BMJ 2014; 348 Summary points Preschool wheeze should be divided into “episodic viral” and “multiple trigger” according to the history, and these categories, which can change over time, should be used to guide treatment No treatment has been shown to prevent progression of preschool wheeze to school age asthma, so treatment is driven solely by current symptoms In all but the most severe cases, episodic symptoms should be treated with episodic treatment Prednisolone is not indicated in preschool children with attacks of wheeze who are well enough to remain at home. Viral Induced Wheeze Case 3 4 year old not quite himself last 2 days. Fever 37.8 No cough or coryza What do you want to know? What is your diagnosis and management? UTI in children NICE recommends that all children without a focus of infection should have a urine sample tested within 24 hours. (A potty washed in hot water with washing up liquid is a good way to get a clean catch). Advise to be vigilant for future infections…............ If <6 months follow up USS within 6 weeks of treated infection or USS at time if complicated/atypical. 6months-3 years- only require imaging/referral if an atypical UTI or recurrent UTI >3 years- USS during infection if atypical. Non-urgent USS and DMSA if recurrent UTI. Non-E.Coli UTI is classed as an atypical UTI>>>>> needs f/u Recurrent - 2 UTI if complicated, 3 if uncomplicated. Cow’s milk protein allergy Cows' milk allergy (CMA), is one of the most common childhood food allergies. It is estimated to affect between 2% and 7.5% of babies under one, though most children grow out of it by the age of five. CMA typically develops when cows' milk is first introduced into your baby's diet either in formula or when your baby starts eating solids. More rarely, it can affect babies who are exclusively breastfed because of cows' milk from the mother's diet passing to the baby through breast milk. There are two main types of CMA: Immediate CMA – where symptoms typically begin within minutes of having cows' milk Delayed CMA – where symptoms typically begin several hours, or even days, after having cows' milk Dorset Guidelines Lactose Intolerance Lactose intolerance is another type of reaction to milk, when the body can't digest lactose, a natural sugar found in milk. However, this is not an allergy. Lactose intolerance can be temporary – for example, it can come on for a few days or weeks after a tummy bug. Symptoms of lactose intolerance include: diarrhoea vomiting stomach rumbling and pains Wind Treatment depends on the extent of intolerance. Some children with lactose intolerance may be able to have small amounts of dairy products without having symptoms. Nocturnal enuresis Up to the age of five, wetting the bed is normal. It usually stops happening as your child gets older without the need for any treatment. up to 1 in 5 five-year-olds wet the bed 1 in 20 10-year-olds wet the bed about 1 in 50 teenagers wet the bed Need investigation if daytime. MSU to exclude infection only if started recently. Try to prevent anger/blame towards child. www.eric.org.uk Alarm is 1st line treatment (can be purchased from eric shop) Any Questions?