* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download The nurse should
Survey
Document related concepts
Transcript
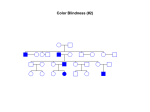
Pediatric Hematological Diseases Hemophilia Hemophilia (Factor VIII deficiency) • • • • • • • • • Sex linked recessive trait Excessive bleeding after circumcision Soft tissue bleeds Joints swollen, warm, and painful May have severe bleeding in GI tract, peritoneal cavity or CNS PTT is prolonged DDAVP Administer Factor VIII even with minor bleed episodes Gene Therapy PTT is prolonged • APTT prolonged Factor VIII deficiency Factor VIII • Blood product • Diluted and given IV The school nurse is assessing a child with hemophilia who has pain in the knee. The nurse suspects hem arthrosis. The nurse should: 1. Perform range of motion 2. Elevate leg above the heart 3. Give ASA or ibuprophen for pain 4. Apply warm soaks to reduce swelling The nurse is giving factor viii to a child with hemophilia. The nurse should observe for which potential complication during the infusion? Fluid overload Transfusion reaction Emboli formation Contracting AIDS Von Will brand Disease • Hereditary • Plasma • Symptoms: • Diagnosis: • Treatment: Von Will brand factor Idiopathic Thrombocytopenia Purpura (ITP) • Autoimmune disorder characterized by increased destruction of platelets • Most common bleeding disorder in children • Most commonly 2-10 years age • Usually follows viral infection • S/S: multiple ecchymosis and petechial • Diag: Hx, < platelets • RX: steroids, IVIG ITP Purpura Platelets A child with a platelet dysfunction has been receiving intravenous fluids for two days. The nurse is discontinuing the IV. The nurse should: 1. Restrict movement of the arm for 12 hours 2. Obtain a culture of the catheter tip 3. Place steri strips over the site 4. Apply direct pressure over the site for 5 minutes Sickle Cell Anemia • Hereditary hemoglobinopathy • Partial or complete replacement of normal hemoglobin S • Any organ can be affected resulting in organ related symptoms Sickle cell anemia • Inherited, autosomal recessive disease • Affects RBC’s acutely sickle shaped • 1 in 500 Black infants in US, occasionally Mediterranean decent • s/s not seen in newborn period due to high levels of fetal hemoglobin Symptoms in SCD • Any organ can be affected and cause symptoms • Symptoms triggered by infection, fever, dehydration, low oxygen level, emotional stress Clinical Manifestations Clinical symptoms are directly related to shortened life span of blood cells. Pathologic changes occur in most body systems and result in multiple signs and symptoms Autosomal Recessive Diagnostic testing • SCD test thru mandatory screening in most states • Hbg electrophoresis- positive diagnosis • Sickledex-Quick screens over 6 months age when fetal hbg fallen Normal Blood Cell Sickle Cell Clinical Management • Teach families watch for symptoms infection • Careful hydration, pain management, oxygen, bed rest to reduce energy and 02 expenditure • Transfusions for severe anemia as needed • Painful episodes—NSAIDS and narcotics Complications of SCD • • • • • • • Stroke (6-15%) CVA Acute chest syndrome Abdominal crises Splenic Sequestration Priapism (painful engorgement of penis) Leg ulcers Decreased resistance to infection Review question SCD Which of the following is true about SCD? A. Sickle cells carry excess oxygen B. Sickle cells decrease blood viscosity C. Sickle cell anemia results in decreased RBC production D. Sickle cell anemia results in increased RBC destruction A two year old child is in SCA crisis. The child is lying with knees flexed against abdomen The nurse would assess further for: 1. Stomach pain 2. Nausea 3. Constipation 4. Fear 2ndary to hospitalization Iron Deficiency Anemia •Most common childhood anemia •Neonatal iron stores from mother depleted after 6 months Causes of Iron Deficiency anemia • Inadequate supply of iron in blood • Excessive milk intake • Inadequate iron stores at birth • Impaired absorption • Blood loss and helminthes • Excessive demands for iron for growth Clinical Manifestations •Pallor, fatigue, irritability •Lab data: HGB, MCH, MCV, serum iron all decreased Underweight Underweight Undernourished Clinical Manifestations • Clubbing of fingers Overweight Diagnosis IDA • Lab studies, Hgb, MCV, microscopic analysis, serum iron binding capacity • Diet history and analysis Best food sources of iron • • • • • • • • • • • Chicken liver, cooked Crab pieces steamed Beef Liver fried Soybeans, baked Spinach, cooked Potato, baked Scallops, steamed Pistachios, dried Broccoli, cooked Cashews, dry roasted Turkey, dark meat Complications of Iron deficiency • Behavior problems • Impaired Cognition • Social problems • Research needed and ongoing Nursing Management/Treatment •Iron absorbed best on empty stomach •Teach developmental nutrition Nursing Management • Absorption • Vitamin C • Dental Care • Tarry stools • GI irritation Nursing Management of IDA • Screening 9 months • Plot growth and development • H and H—more detailed tests if abnormal • Diet History and education Aplastic Anemia • Deficiency of all blood cells • Congenital • Acquired Aplastic Anemia Disseminated Intravascular Coagulation • Serious condition in which clotting mechanisms are disturbed • Leads to extensive clotting and tissue damage. Review Questions • Foods that contain iron for a teenager’s diet are? • How is iron best absorbed? • What vitamin helps absorption of iron? • Side effects of iron taken orally? Questions Immune Function In Children Severe Combined Immune Deficiency Disorder • • • • • • Etiology Clinical Manifestations Diagnosis Clinical Therapy Prognosis Nursing Management Wiskott-Aldrich Syndrome • Combined congenital immune deficiency syndrome • X linked recessive • 4 in 1 million male births • Diagnosis: Thrombocytopenia • Treatment • Nursing Management HIV follows two patterns in children • Fast progresses—about 1/3 of children who develop serious signs and symptoms including encephalopathy, FTT, and opportunistic infections within the first 2 years of life • Less rapid progresses—approximately 2/3’s of children who develop less serious symptoms such as lymphadenopathy and recurrent childhood illness Diagnostic testing • HIV PCR (polymerase chain reaction) done by 2 weeks of age, preferable in first 48 hrs and repeated in 2 weeks if neg-also at 1-2-3-6 months • Antigen antibody ELISA ^ 18 months • CD4: measure of how well immune system working • Viral load: measure how much virus in blood Treatment HIV • Pregnant HIV women should start ZDV 1434 weeks thru pregnancy • Imperative women in labor to get ZDV for babies to receive it in first 12 hrs life • Babies ZDV 4x day until 6 weeks old • Exposed children followed closely treated with antivirals—method ongoing and effective • Monitor viral load, labs—very supportive care for entire family Immunizations and HIV • Same immunizations on same schedule as other children, including IPV, should not receive OPV • May receive MMR and Varicella vaccines if asymptomatic and CD4 levels 15-25 % • If exposed to Varicella and did not receive vaccine should be given VCG • Should take Pneumococcal and Influenza vaccines Review • What is the difference between HIV and AIDS? • What vaccines should a child with HIV receive at the 2 year visit (if the CD4 count is normal)? • What if a child with HIV is exposed to C Pox and has not had the immunization? What should the child receive? Herpes simplex 1 more than 1 mo. Herpes simplex 1 eye Kaposi's sarcoma Oral Kaposi sarcoma Pneumocystis Carinii Pneumonia (PCP) Juvenile Rheumatoid Arthritis • Chronic joint inflammation diagnosed prior to 16 yrs age • Peak age 1-3 yrs • > in females • Systemic autoimmune disorder with multiple manifestations Juvenile idiopathic Arthritis • Polyarthritis:5 or more joints and uveitis (30%) • Oligo arthritis: knees, ankles, elbows affects females (50-60%) • Systemic: males and females+ many joints, fever, rash, lymphadenopathy, hepatic splenomegaly Etiology/Prognosis • Theories of autoimmune process • 70 % experience permanent remission of disease by adulthood • Early onset better prognosis for complete recovery Pathophysiology/ Clinical S/S of JRA • Chronic inflammation of synovium with joint effusion and eventual erosion, destruction, fibrosis or articular cartilage • Symptoms Diagnosis and Management JRA • Diagnosis of exclusion • No specific labs • RF, HLA B27, ANA ESR, CRP detect amount of inflammation • X-rays rule out fractures Management • Medication, OT, PT, Exercise (noncontact) • Education :Complications Uveitis Well balanced diet, Meds with food Influenza vaccine yearly Peer contact Over exertion exacerbation symptoms Review Study • What would an appropriate activity be for a child with JRA? • What is thought to be the cause of JRA? • What are the common symptoms? Review Study • What would an appropriate activity be for a child with JRA? • What is thought to be the cause of JRA? • What are the common symptoms? Know s/s allergy • Get to medical care ASAP • Teach importance epipen • Which of the following assessment findings aids in diagnosing (HIV) human deficiency syndrome in children? • A. excessive weight gain • B. arrhythmia • C. Intermittent diarrhea • D. Tolerance of feedings • The primary goal of treatment for the child with JRA is to maintain: • A. joint function • B. excessive weight gain • C. Social isolation • D. Skin breakdown • What oral drugs are used for JRA? Side effects? • What drug has ASA besides ASA?