* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download PFO case study
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Echocardiography wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Electrocardiography wikipedia , lookup
Atrial septal defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
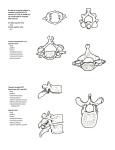
NUR 580 CASE STUDY Atypical Presentation of Congenital Anomaly CHIEF COMPLAINT “I’ve been sick for a few weeks now with this sinus thing and I’m having shortness of breath from it.” HISTORY OF PRESENT ILLNESS 17 yo female presents to her PCP office with: SOB/Chest tightness Times one week following treatment of URI Gradual onset Decreased with with rest Exacerbated by any prolonged (more than 5 minutes) activity such as walking Severity a 7/10 at its worst and 2/10 at baseline No pain involved Never occurred before Has lasted for one full week Went to ER day prior to this office visit and left after waiting for 7.5 hours. HPI CONTINUED…. Patient developed “chest tightness” that does not radiate and is brought on with previously described SOB. Cannot rate a pain intensity to it as she states “it doesn’t really hurt, it’s just weird when I’m really breathing hard after like walking to the office here.” Went to ER for this same complaint yesterday and sat in waiting room with her mom for 7.5 hours before leaving to go home. HPI CONTINUED…. Patient was also treated with Z-pak x5 days and Augmentin x10 days prior to onset of the current symptoms and previously tested positive for the flu following 5 days of symptoms. R.O.S. General: No: Changes in appetite Weight loss Denies: Fever Weakness Fatigue Skin: Denies: Rashes Lumps Sores Itching Dryness Changes in color of: Hair Nails R.O.S. Head: Denies: Ears: Dizziness Lightheadedness Headache Eyes: Denies: Blurred/double vision Spots/specks Flashing lights Excessive tearing Does not wear corrective lenses Denies: Hearing loss Tinnitus Vertigo Earaches Infection Discharge Nose/Sinuses: Denies: Itching/sneezing/bleeds Sinus pain/congestion Treated for URI more than 10 days ago R.O.S. Throat: Denies: Bleeding gums Frequent sore throats Sore tongue Dry mouth Hoarseness Last Dental Exam x8 months prior. Neck: Denies: Swollen glands/lumps/pain/stiffn ess in neck Breasts: N/A Respiratory: Denies: Hemoptysis Wheezing Complains of: Dyspnea on exertion Cough occassionally Dry Non-productive R.O.S. Cardiovascular: Denies: Rheumatic fever Murmurs Palpitations Orthopnea Edema Complains of: Chest pressure (see HPI) No recent blood work or ECG GI/GU: N/A Peripheral Vascular: N/A Urinary: N/A Genital: N/A Musculoskeletal: Denies: Trauma to chest Manually reproducible pain CP reproducible with deep inspiration/movement R.O.S. Psychiatric: Neurologic: N/A N/A Hematologic: Denies: Anemia Blood dyscrasias Endocrine: N/A PAST MEDICAL HISTORY General: Allergies: Not being medically treated for anything at this present time. None Medical Illness: Recently treated for URI that did not respond well to treatment and original symptoms have since dissipated and left with complaints of SOB/CP as described in HP. Denies: HTN, MI, CHF, COPD, Asthma, Cancer States had some heart defect as a child that resolved itself in a a few days. Mother states it was VSD that closed on it’s own shortly after her birth but was monitored and has not had issues with this. Cardiology cleared her of this years ago. PAST MEDICAL HISTORY Accidents/Injuries: Surgery/Hospitalizations/Transfusions: Broke her left forearm 2 years ago during cheerleading competition, no concerns/problems with it now. None reported Immunizations: School immunizations up to date and not on file at the office. Flu Shot received this season. Medications: None PAST MEDICAL HISTORY Family History/Social History: No: DM, Anemia, Cancers, HTN, Cardiac anomalies/problems. All family members alive and well. Does not smoke Has one glass of wine with family at home on special occasions. Occupation: Full Time High School Student Cheerleader Runs Track PAST MEDICAL HISTORY Insurance/Finance: Marital Status: Sleeps from 5-8 hours per night Safety: Single, no significant other Habits: Health insurance provided through her parents Drives with seat belt/at posted speed. Nutrition: Eats home cooked meals and school lunch most of the time, rarely eats out with friends. PHYSICAL EXAM General: Vitals: 122/78 – 104 – 98.7 – 26 – 0/10 – 95% on RA Height/Weight/BMI: White female pleasant and cooperative, well groomed, slim in appearance in mild respiratory distress upon initial presentation to the office. 5’7” 118 lbs, 18.5(normal) Skin: Warm, pink, intact with no lesions. Slight diaphoresis PHYSICAL EXAM Head: Normocephalic/atraumatic, symmetric Hair dry/intact. No lesions/balding/tenderness. No sinus pain with palpation. Nasal turbinates pink/pale with no drainage Eyes: Acuity 20/20 uncorrected Fields intact Pupils 5mm down to 2mm, equal, round, reactive to light and accommodation with consensual response. Sclera clear/white bilaterally. No: Nystagmus Ptosis Proptosis Lid lag Swelling Disc margins sharp, no hemorrhages or exudates, A:V ratio 2:3 and no AV nicking. Red reflex intact. Eye lids and lashes/brows intact PHYSICAL EXAM Ears: Tympanic membranes clear/pearly gray with appropriate landmarks Acuity good to whisper test Neck: Denies: Tenderness with palpation Difficulty swallowing Trachea midline No pre/post auricular, tonsilar, cervical, submandibular, submental, or supra clavicular lymphadenopathy. Mouth/Pharynx: Mucous membranes moist with mild erythema of uvula and mild clear post nasal drip Tonsils grade 2, pink PHYSICAL EXAM Breasts: N/A Respiratory: Thorax symmetric with good expansion Lungs resonant Breath sounds clear and equal bilaterally with no adventitious sounds No Bronchophony Egophony Diaphragm descends 6cm bilaterally Tachypneic at rest PHYSICAL EXAM Cardiovascular: S1 & S2 with no extra heart tones HR fast but regular Peripheral Vascular: GI/GU: N/A N/A Musculoskeletal: No deformity to chest wall No point tenderness No swelling Neurological: N/A DIAGNOSTICS 12 lead ECG (Stat): Blood work: T wave inversion in septal leads Cardiac Enzymes D-Dimer CBC with Diff. CMP Lipase Amylase Radiology: Chest X-ray Chest CT DIFFERENTIAL DIAGNOSIS ACS – Cardiac Enzymes/ECG (Serial) Costochondritis – Treatment with NSAIDS/rest Pulmonary Embolism – X-ray and CT will rule out Rib Fracture – X-ray will rule out PDA – (Typical in young children & very uncommon finding in adults Aortic Aneurysm – Radiology Imaging Aortic Dissection - Radiology Imaging Tension Pneumothorax - Radiology Imaging Pericarditis – ECG further testing Endocarditis Esophageal Tear - Radiology Imaging Pleuritis - Radiology Imaging, ECG GERD – symptoms and ruling out all other emergent causes of symptoms DIAGNOSIS Taken to local Emergency Department via Ambulance for continual monitoring and serial labs plus ECG. Patient followed up with PCP a week after the incident with a diagnosis of….. Patent Foramen Ovale A small opening in the septum between the atria’s. EPIDEMIOLOGY Prevalent in about 1 in 1,500 live births Undetected due to lack of symptoms Common in about 25% of the population No age/gender predominance PATHOPHYSIOLOGY During fetal circulation the PFO is a normal opening to allow the lungs to be bypassed, however closes very quickly after birth once the pulmonary pressures increase. Some PFOs do not close entirely but are so small that they are never detected Causes of reopening or increased symptoms are: Pressurization injuries or rapid changes Viral illness with respiratory compromise Right atrial pressures rise: Coughing PE Pneumonia Other respiratory conditions DIAGNOSTICS Known cardiac defects from childhood Agitated saline injection during Trans esophageal echocardiogram (TEE) or Trans thoracic echo. ECHO during coughing or major illness ECG – Septal changes noted, prolonged PRI (enlargement of Atria) Ejection systolic murmur if Pulmonic valve is involved Commonly found in deep water divers or sky diving. Common symptoms are: SOB with minimal exercise CHF CVA Cryptogenic CVA Abnormal ECG initially Migraines Cryptogenic CVA (small emboli typically go through the lungs and are absorbed, with this malformation they go directly to the body. SUGGESTED TREATMENT/PREVENTION Prevention focuses on early diagnosis and treatment prior to significant cardiac/neuro changes occur such as hypertrophy, CVA, MI. Correction is rarely needed as risk outweighs the benefit and patients are usually asymptomatic PFO repair: Open Heart Surgery Percutaneous implant/patch Medical management of symptoms Routine screening is not cost effective and is not covered by insurance companies so costs would be out of pocket. Screening is covered for patients who have TIAs or CVAs due to this possibly being cardiac related. Symptoms resolved following further treatment of cough which was from a resolving URI. She will be monitored by a cardiologist for worsening symptoms PATIENT EDUCATION Focus is on: S&S of peripheral arterial embolism CVA TIA DVT Importance of cardiology follow-up REFERENCES “ASD-PFO” (2006). Retrieved from http://www.marmur.com/ASD-PFO.html Butera, G., Romagnoli, E., Sangiorgi, G., Caputi, L., Chessa, M., & Carminati, M. (2008). Patent foramen ovale percutaneous closure: the no-implant approach. Circulation, 116, 1701-1706. Carroll, J. D., Dodge, S., & Groves, B. M. (2005). Percutaneous patent foramen ovale closure. Cardiology Clinics, 23, 15-33. “Diseases and Conditions: Patent foramen ovale” (2012). Retrieved from http://www.mayoclinic.org/diseasesconditions/patent-foramen-ovale/basics/definition/CON-20028729 Fisher, D., Fisher, E., Budd, J., Rosen, S., & Goldman, M. (1995). The incidence of patent foramen ovale in 1,000 consecutive patients. a contrast transesophageal echocardiography study. CHEST, Kerut, E., Lee, S., & Fox, E. (2006). Diagnosis of an anatomically and physiologically significant patent foramen ovale. Echocardiography: A Journal of CV Ultrasound & Allied Tech., 239, 810-815. Kizer, J. R., & Devereux, R. B. (2005). Patent foramen ovale in young adults with unexplained stroke. The New England Journal of Medicine, 353, 2361-2372. Naqvi, T., Rafie, R., & Daneshvar, S. (2010). Potential faces of patent foramen ovale. Echocardiography, 897907. “Patent Foramen Ovale” (2011). American Heart Association. Retrieved from http://www.heart.org/HEARTORG/Conditions/More/CardiovascularConditionsofChildhood/Patent-ForamenOvale-PFO_UCM_469590_Article.jsp “Patent Foramen Ovale” (2013). Retrieved from http://www.nlm.nih.gov/medlineplus/ency/article/001113.htm “Patent Foramen Ovale” (2015). Retrieved from https://online.epocrates.com/noFrame/showPage?method=diseases&MonographId=951&ActiveSectionId=52 “PFO” (2014). Retrieved from http://my.clevelandclinic.org/services/heart/disorders/congenital/pfo/hic_Patent_Foramen_Ovale_PFO