* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download the muscular system
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiac surgery wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Myocardial infarction wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
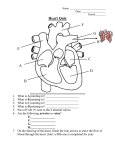
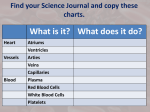
Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) LEVEL 3 DIPLOMA IN AROMATHERAPY MODULE 15 KNOWLEDGE OF ANATOMY, PHYSIOLOGY & PATHOLOGY FOR COMPLEMENTARY THERAPIES THE CARDIOVASCULAR SYSTEM MODULE 8 COURSE MANUAL CHRISTINA LYNE [email protected] Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) THE CARDIOVASCULAR SYSTEM This system is composed of the blood, blood vessels and the heart. It distributes oxygen and essential nutrients to the whole body and carries away carbon dioxide for excretion and potentially damaging waste products. It is the body’s main transportation system. WHAT IS BLOOD? Blood is a fluid connective tissue contained within a closed system of vessels. It consists of billions of cells suspended in a watery liquid. It circulates by the pumping action of the heart. Adult bodies contain approximately 4-5 litres. FUNCTIONS OF BLOOD Transports oxygen, carbon dioxide, nutrients and hormones around the body. Transports waste materials from the body to the organs of excretion. Transports heat around the body. Helps fight against foreign microbes and toxins and prevents infection. Prevents excessive loss of blood after accidents by clotting. Regulates body temperature, the body’s pH balance and water content of the cells. COMPOSITION OF BLOOD Blood is a thick, red liquid composed of four parts: red blood cells white blood cells platelets plasma BLOOD PLASMA is a watery, straw-coloured liquid and is the liquid part of blood. It consists mainly of water. 91.5% of plasma consists of water and the other 8.5% contains dissolved substances. It serves as a transport system delivering various materials to and from the cells. Without plasma, blood cells would be unable to travel around the body. Plasma consists of both helpful and harmful components: Helpful components: plasma retrieves the nutrients necessary for the body’s survival from organs such as the liver and the small intestine. These nutrients, delivered to the cells, are usually the results of digestion: amino acids, glucose, mineral salts, vitamins, fats and hormones. Plasma also supports the body’s defence system, as it contains antibodies, antitoxins and fibrin (a clotting agent that works with platelets to help heal wounds). Harmful components: Along with vital elements, plasma also carries harmful substances such as urea from the cells to the kidneys, where it is excreted in urine. It also absorbs the carbon dioxide resulting from respiration as hydrogen carbonate ions, which returns to carbon dioxide when the body exhales. Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) COMPONENTS IN BLOOD PLASMA Component Description Function Acts as a solvent and suspending medium for carrying other substances. Also absorbs, transports and releases heat Water Proteins albumins, globulins and fibrinogen Albumins – contribute to the osmotic pressure of blood and transport fatty acids, some lipid-soluble hormones and certain drugs Globulins – transport lipids, hormones and some mineral salts and function in defence (immunoglobulins), produced by lymphocytes Fibrinogen – functions in blood clotting Electrolytes sodium, calcium, chloride, potassium, magnesium, bicarbonate Maintain osmotic pressure, pH buffering and regulation of membrane permeability. Also serve as essential minerals Nutrients amino acids, glucose, glycerol, fatty acids Serve as essential nutrients for the cells Regulatory substances enzymes & hormones Enzymes – catalyse chemical reactions Hormones – regulate cellular activity Gases oxygen, carbon dioxide, nitrogen All are transported around the body dissolved in plasma Wastes urea, uric acid Carried to the organs of excretion TYPES OF BLOOD CELLS - there are three types: RED BLOOD CELLS - Erythrocytes These are the most numerous type of blood cell. They have no nucleus and are smaller than most other cells. They are shaped like biconcave discs. These discs are able to fold and bend and this makes it easier for them to squeeze through the smallest blood vessels and to collect oxygen and release it. It also provides a large surface area for the diffusion of gases into and out of the cells. Each cell has a life span of about four months, and is then destroyed either in the liver or the spleen. About 250 000 million red cells have to be replaced each day. Red cells are produced in the red, spongy bone marrow of long bones e.g. femur, ulna, fibula, radius, etc. Their chief function is to carry oxygen from the lungs to the tissues. These blood cells carry haemoglobin, a transport protein that contains iron. Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) WHITE BLOOD CELLS - Leucocytes These blood cells are white in colour because they do not contain haemoglobin. They are produced in the bone marrow and in lymphatic tissue. They have a short life span ranging from a few hours to a few days. They are able to increase rapidly in cases of serious infection by a process called mitosis. Their function is to help the body to fight infection and combat disease. There are two main groups of white blood cell - granulocytes and agranulocytes: 1. Granulocytes are made in the bone marrow. All granulocytes have multilobed nuclei in their cytoplasm. They defend the body against viruses and bacteria and form 75% of white blood cells. The following are all granulocytes: Type Structure Function Neutrophils Nucleus has 2-5 lobes. Cytoplasm has very fine, pale lilac granules They protect the body against microbial invasion and remove dead cells and debris from damaged tissue. They very quickly engulf and kill bacteria by phagocytosis. They contain enzymes to digest engulfed material Eosinophils Cytoplasm has large red - orange coloured granules They help to eliminate parasites / worms. They are found at the sites of allergic inflammation – asthmatic airways and skin. They help in the inflammatory process Basophils Nucleus has 2 lobes. Has large cytoplasmic granules that appear blue-purple They react to allergens and release heparin (anticoagulant) and histamine (inflammatory agent) to promote inflammation. They are closely associated with allergic reactions 2. Agranulocytes - make up the remaining 25% of white blood cells and are produced mainly in the lymphatic system. They have a large nucleus and do not contain cytoplasmic granules. Type Structure Function Lymphocytes Are smaller than monocytes. They have a large nucleus and no cytoplasmic granules. They contain T and B lymphocytes. These are found in lymphatic organs such as the spleen and lymph nodes. They are able to respond to antigens (foreign material). They play an important role in immunity Monocytes These are the largest white blood cells. They have a large nucleus and no cytoplasmic granules. Some circulate in the blood and have a phagocytic role. Others migrate into the tissues and become macrophages. They are powerful scavengers and clean up areas of chronic infection Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) PLATELETS - thrombocytes These are very small, granular, disc-shaped cells containing no nucleus. They are so small that they make up just a fraction of the blood volume. They originate from cells known as megakaryocytes, which are present in the bone marrow. When more thrombocytes are needed, the kidneys produce a hormone called thrombopoietin that stimulates the bone marrow to produce more megakaryocytes, which can then be broken up into hundreds of smaller thrombocyte pieces. They contain proteins on their surface that allows them to stick to breaks in the blood vessel wall and also to stick to each other. They also contain proteins that allow them to change shape when they become sticky. Thrombocytes survive for about 8 – 11 days and those not used are destroyed by macrophages, mainly in the spleen but also in the liver. About a 1/3rd are stored in the spleen and are released in an emergency when excessive bleeding needs to be controlled. The function of platelets is to prevent blood loss by forming a platelet plug. Their granules secrete proteins that promote vascular spasm and blood clotting. THE HEART FUNCTION The heart is the pump that drives the whole circulatory system. It receives and propels blood, rhythmically contracting, forcing the blood through a system of vessels (arteries, veins and capillaries). The heart’s action is controlled both by the autonomic nervous system and the relaxation and contraction of the cardiac muscle. The function of the heart is to pump blood around the body. LOCATION The heart is located in the thoracic cavity in the mediastinum (the space between the lungs). It lies left of the median line. THE STRUCTURE OF THE HEART The covering of the heart (outer pericardium) The heart is surrounded and protected by a triple-layered sac called the pericardium which is composed of: The outer fibrous pericardium – made of tough, inelastic connective tissue that prevents overstretching of the heart and anchors it in the mediastinum. The inner serous pericardium – made of a thin membrane that forms a double layer around the heart. The outer parietal layer is fused to the fibrous pericardium The inner visceral layer (epicardium) adheres to the heart The outer sac consists of fibrous tissue and the inner sac consists of a continuous layer of serous membrane. The serous membrane consists of flattened epithelial cells and secretes serous (pericardial) fluid into the space between the visceral and parietal layers. This then allows for smooth movement (reduces friction) between them when the heart beats. Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) The walls of the heart The heart is surrounded by a muscular wall with membranes covering and lining it. The wall is divided into three layers: 1. Inner Endocardium: this inner membrane lines the chambers and valves of the heart. It consists of a thin, smooth membrane composed of flattened epithelial cells. The smooth lining allows the blood to flow easily inside the heart. 2. Middle Myocardium: this middle layer is composed of a thick layer of specialised cardiac muscle tissue which is involuntary, striated and arranged in spiral-shaped bundles of one or more branches. It contracts to pump blood. 3. Outer Pericardium: this outer layer is also called the visceral layer of the serous pericardium (see above – covering of the heart) The chambers of the heart The heart is a hollow red organ. It is divided into four chambers lined with endocardium. 1. 2. 3. 4. Right atrium Right ventricle Left atrium Left ventricle The two atria are thin-walled chambers that receive blood from the veins. The two ventricles are thick-walled chambers that forcefully pump blood out of the heart. Differences in thickness of the heart chamber walls are due to variations in the amount of myocardium present. The walls of the left ventricle are much thicker than those of the right as it has to pump blood out to the entire body, whereas the right ventricle only has to pump blood to the lungs. Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) The right atrium receives deoxygenated blood from systemic veins; the left atrium receives oxygenated blood from the pulmonary veins. Valves of the Heart Pumps need a set of valves to keep the fluid flowing in one direction and the heart is no exception. The heart has four valves that keep the blood flowing in the right direction. They are composed of dense connective tissue covered by endocardium and they open and close in response to pressure changes as the heart contracts and relaxes. Each valve has flaps that open to let blood flow forwards only. 1. The right atrioventricular valve is also known as the tricuspid valve. 2. The left atrioventricular valve is also known as the bicuspid, or mitral, valve. These lie between the atria and ventricles. 3. The valve between the right ventricle and pulmonary trunk is the pulmonary semilunar valve. 4. The valve between the left ventricle and the aorta is the aortic semilunar valve. These lie between the ventricles and the arteries. The flow of blood through the heart to the body The two largest veins of the body – the superior and inferior venae cava - empty their contents into the right atrium. This blood passes through the tricuspid valve into the right ventricle and from there is pumped through the pulmonary valve and into the pulmonary artery (the only artery in the body that carries deoxygenated blood). After leaving the heart, the pulmonary artery divides into two – the right and left pulmonary arteries - which carries the venous blood to the lungs where the exchange of gases takes place: carbon dioxide is excreted and oxygen is absorbed. Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) Blood picks up oxygen in the lungs Two pulmonary veins from each lung carry oxygenated blood back to the left atrium. Blood then passes through the mitral valve into the left ventricle. It is then pumped through the aortic valve (formed by three semilunar cusps) into the aorta and to the body. The heart has a double pump which pumps blood into two different circulations (see notes on circulation of blood). CONDUCTING SYSTEM OF THE HEART The heart generates its own electrical impulses and beats independently of nervous or hormonal control i.e. it is not reliant on external mechanisms to initiate each heartbeat. Specialised areas in the heart wall provide the conduction system of the cardiac cycle. Two areas are called nodes whilst the third is a group of fibres called the atrioventricular bundle. Sinoatrial node (SA) This small mass of specialised cells lies in the wall of the right atrium near the opening of the superior vena cava. This is the part of the heart muscle where each heartbeat, or contraction, originates. It is called the pacemaker of the heart because it controls the heart rate. The heartbeat spreads from the SA node through the rest of the cardiac conduction system to reach all parts of the heart muscle, allowing contraction to occur in a coordinated manner. Atrioventicular node (AV) The AV is located between the atria and the ventricles. It is a collection of nerve and muscle cells that conducts signals between the upper and lower chambers of the heart. The AV node works in conjunction with the SA node. Impulses in the heart travel as follows: The SA node generates an electrical impulse that begins the heartbeat Contraction of the atria takes place as waves travel throughout the muscle The AV node is stimulated; a slower conduction through this node allows time for the atria to completely fill with blood and contract Waves rapidly travel throughout the ventricular walls though the bundles of fibres Both left and right ventricles contract almost at the same time CARDIAC CYCLE Systole – means contraction Diastole – means relaxation Atrial systole – contraction of the atria Ventricular systole – contraction of the ventricles Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) The cardiac cycle is the sequence of pumping and filling that occurs from the start of a heartbeat to its finish. The heart undergoes two main events during a complete cardiac cycle - diastole and systole. During diastole, the heart relaxes and fills with blood and during systole, the heart contracts and pumps the blood. It takes about one second to complete an entire cardiac cycle. The heart is composed of four chambers: the two atria on top and two ventricles on bottom. The atria receive blood from the body into the heart and the ventricles are responsible for pumping blood out of the heart. The first stage is a systolic, or relaxed, stage. The right atrium takes in deoxygenated blood from the body through the superior and inferior vena cavas. Since the right atrium and ventricle are relaxed and the tricuspid valve between the two chambers is open, the blood flows into the right ventricle. An electrical impulse from the sinoatrial (SA) node tells the atrium to contract and push in the remaining blood and signals to the Purkinje fibres. The Purkinje fibres cause the ventricle to contract, or go into the first stage of systole in the cardiac cycle, and pump the deoxygenated blood out of a semilunar valve into the pulmonary artery. The pulmonary artery takes the blood to the lungs, where it can be re-oxygenated. From the lungs, the oxygenated blood comes back into the heart via the pulmonary veins, and is received in the left atrium. The heart is now in the second stage of diastole, so the left atrium is relaxed and the tricuspid valve is open. The blood passes though the valve into the left ventricle. The left ventricle receives the signal from the Purkinje fibres to contract, or go into the second stage of systole. This contraction forces open the semilunar valve to the aorta, where the blood is pumped out to the rest of the body. Because blood is circulating continuously, the heart doesn’t have to wait for blood to return from the body or the lungs, so it is constantly filling up and pumping out. For this reason, the filling up of one side of the heart occurs at the same time as the filling up of other side, and the contraction of one side occurs simultaneously with the contraction of the other. So the first and second stages of diastole in the cardiac cycle happen simultaneously, and then the first and second stages of systole occur. The “lub-dup” noise heard when listening to the heartbeat is the sound of the valves closing. The “lub” is the sound of the atrioventricular valves closing, and the “dup” is the sound of the aortic valve closing. HEART RATE The heart rate is the number of times in a minute that the heart completes a cardiac cycle – commonly measured as a pulse. PULSE / HEART RATE Pulse refers to the rhythmic expansion of an artery that is caused by ejection of blood from the ventricle. The pulse can be felt in arteries that lie close to the surface of the body (radial artery / carotid artery) Each contraction of the left ventricle forces about 60 to 80 mls of blood through the already full aorta and into the arterial system. The aortic pressure wave is transmitted through the arterial system and can be felt where an artery is close to the surface and rests on something firm – like a bone. The number of pulse beats per minute normally represents the heart rate and varies considerably in different people and in the same person at different times. In health, the pulse rate and heart rate are identical, about 60 to 80 beats per minute at rest. The heart rate determines cardiac output. If the heart rate rises, cardiac output increases, and if it falls, cardiac output falls too. Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) Factors affecting pulse / heart rate Exercise: active muscles need more blood which is achieved by an increased heart rate Emotion: during time of stress, excitement, fear, anger, heart rate is increased Age: children have a higher heart rate than adults Gender: females have a higher heart rate than males Drugs: certain drugs can have an effect on the pulse rate Temperature: the heart rate rises and falls with body temperature Position: the heart rate is usually faster when a person is standing Tachycardia indicates an abnormally rapid resting heart or pulse rate - over 100 beats per minute. Bradycardia indicates an abnormally slow resting heart or pulse rate - under 60 beats per minute. Control of heart rate by nerves Cardiac muscle can contract without the need of a nerve supply from the brain provided it has a sufficient oxygen supply. The heart has a built-in pacemaker, so it will naturally beat at between 60 and 100 beats per minute. However, the following nerves are also able to control the rate at which the heart beats: Sympathetic nerves –these stimulate the release of noradrenaline, which, acting as a neurotransmitter, increases the heart rate. Parasympathetic nerves – these stimulate the release of the neurotransmitter acetylcholine which decreases the heart rate. Both sets of nerves ensure that the heart rate adjusts itself to meet demands. Control of heart rate by hormones Hormones such as adrenaline and noradrenaline increase the heart rate. Their release is stimulated by stress, exercise and excitement. Thyroid hormones can also increase the heart rate. BLOOD PRESSURE Blood pressure is the force or pressure that the blood exerts on the walls of the arteries. Systemic arterial blood pressure maintains the essential flow of blood into and out of the organs of the body. In common usage, the term blood pressure refers to arterial blood pressure, the pressure in the aorta and its branches. When the left ventricle contracts and pushes blood into the aorta, the pressure produced within the arterial system is called systolic pressure. In adults it is about 120 mmHg. Keeping blood pressure within normal limits is very important. If it becomes too high, blood vessels can become damaged, causing clots or bleeding from sites of blood vessel rupture. If it falls too low, then blood flow through the tissue beds may be inadequate. This can be very dangerous for essential organs such as the heart, brain or kidneys. Blood pressure is used as an indicator of the health of the blood vessels and heart. Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) Blood pressure varies according to the time of day, the posture, gender and age of the individual. Blood pressure falls at rest and during sleep. It increases with age and is usually higher in women than in men. Measuring blood pressure Blood pressure is the difference between systolic pressure and diastolic pressure. The first figure is the systolic pressure and shows the force exerted by blood on the walls of the arteries during contraction of the left ventricle. The second figure is the diastolic pressure and measures the pressure on the walls of the arteries during relaxation of the left ventricle. Arterial blood pressure is measured in millimetres of mercury (mmHg) with a sphygmomanometer and is recorded as the systolic pressure over the diastolic pressure. In a normal young adult, blood pressure is 120/80mm Hg while at rest. High blood pressure can be caused by smoking, obesity, lack of exercise, eating too much salt, stress, a high intake of alcohol, pregnancy, the contraceptive pill and hereditary factors. Factors affecting blood pressure Blood pressure is increased or decreased by the following factors: Cardiac output – this relates to the amount of blood pumped out of the heart. In an adult approximately 5 litres of blood passes through the whole body in one minute. Cardiac output is affected by the heart rate. If the demand for blood is high, this will increase the heart rate e.g. in exercise, and blood pressure will also increase. Blood loss decreases cardiac output and this decreases blood pressure. Volume of blood – this is the amount of blood that is present in the body. The more blood present in the body, the higher the rate of blood return to the heart and the resulting cardiac output. Blood vessel radius – resistance is related to blood vessel radius (the larger the radius, the lower the resistance). A decrease in the radius of a blood vessel increases resistance and thus increases blood pressure. Elasticity of blood vessel walls - arterioles have a tunica media composed almost entirely of smooth muscle, which responds to nerve and chemical stimulation. When elastic tissue in the tunica media is replaced by inelastic fibrous tissue as part of the ageing process, blood pressure rises. Blood vessel length - the longer the vessel, the higher the resistance. Obese people have longer vessels as additional vessels are needed to supply the additional adipose tissue. Viscosity – or thickness of blood can affect blood pressure. Certain medical conditions can alter the viscosity of blood. Anaemia or haemorrhaging reduces viscosity thereby reducing blood pressure. Dehydration increases thickness thereby increasing blood pressure. Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) BLOOD PRESSURE REGULATION Blood pressure is controlled in two ways: 1. Short-term control involving the baroreceptor reflex, chemoreceptors and the hypothalamus (higher centre). 2. Long-term control involving the regulation of blood volume by the kidneys and the renin-angiotensin-aldosterone-system. Short Term Regulation Baroreceptors These are nerve endings sensitive to pressure changes (stretch) within the vessels, situated in the aortic arch and in the carotid sinuses, and are the body’s principal moment-to-moment regulatory mechanism for controlling blood pressure. A rise in blood pressure in these arteries stimulates the baroreceptors to alert the cardiovascular centre (CVC) located in the brain stem. The CVC responds by increasing parasympathetic nerve activity to slow down the heart. At the same time, sympathetic activity to the blood vessels is inhibited, causing vasodilation. This results in a drop in blood pressure. If pressure within the aortic arch and carotid sinuses falls, the baroreceptors stop stimulating the CVC. As a result of this lack of stimulation, heart rate increases, cardiac output increases, and blood pressure increases to the normal level. Chemoreceptors These are nerve endings situated in the carotid and aortic bodies and are primarily involved in the control of respiration. They are sensitive to the changes in the levels of carbon dioxide, oxygen and the pH levels of blood. When changes are detected by the chemoreceptors, they send signals to the CVC, which then increases sympathetic nerve activity to the heart and blood vessels, pushing up blood pressure to improve tissue blood supply. Blood oxygen levels are also increased. Chemoreceptors only activate when severe disruption of respiratory function occurs or when BP drops dramatically. Higher centres in the brain Input to the CVC from the higher centres is influenced by emotional states such as fear, anxiety, pain and anger that may stimulate changes in blood pressure. The hypothalamus controls body temperature and influences the CVC, which responds by adjusting the diameter of blood vessels in the skin – an important mechanism for controlling heat loss and retention. Long Term Regulation Both of these systems regulate blood volume, thus influencing blood pressure: Renin-Angiotensin-Aldosterone (RAA) System When blood volume falls or blood flow to the kidneys decreases, cells in the kidneys secrete renin into the bloodstream. Together, renin and angiotensin converting enzyme (ACE) produce the active hormone angiotensin II, which raises blood pressure by causing vasoconstriction. Angiotensin II also stimulates secretion of aldosterone (increases Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) reabsorption of sodium ions and water by the kidneys). The water reabsorption increases total blood volume, which increases blood pressure. ADH - Anti-Diuretic Hormone ADH is produced by the hypothalamus and released from the posterior pituitary in response to dehydration or decreased blood volume. Among other actions, ADH causes vasoconstriction, which increases blood pressure. ANP - atrial natriuretic peptide In addition, the cells in the atria of the heart releases a hormone called ANP. ANP lowers blood pressure by causing vasodilation and by promoting the loss of salt and water in urine, which also reduces blood pressure. CIRCULATION OF BLOOD CORONARY CIRCULATION - circulation within the heart Arterial supply - The heart itself is, of course, a muscle and needs a constant supply of oxygen and nutrients and constant removal of its waste products to help it to operate efficiently. So it has its own circulatory system called the coronary circulation. The heart is supplied with arterial blood which arrives from the left ventricle. It passes through the aorta and to the right and left coronary arteries and branches within the heart wall to form a vast network of fine capillaries to feed the heart tissue cells. Venous drainage - Most of the deoxygenated blood is then collected back into the coronary veins that then join to form the coronary sinus, which opens into the right atrium. PULMONARY CIRCULATION – circulation between the heart and lungs Deoxygenated blood travels to the heart via the inferior vena cava and the superior vena cava into the right atrium. Blood flows from the right atrium through the tricuspid valve and into the right ventricle. From there, it passes through the pulmonary valve and into the pulmonary arteries. The blood goes to the lungs where an exchange of gases occurs. Carbon dioxide is breathed out and fresh supplies of oxygen and picked up. The blood is now oxygenated. The oxygenated blood is then returned via the pulmonary veins to the left atrium. SYSTEMIC CIRCULATION – circulation from the heart to the body and back to the heart Oxygenated blood passes from the left atrium through the bicuspid valve and into the left ventricle. It then passes to the aorta. Each part of the aorta gives off arteries that branch, leading to organs and finally to the arterioles and capillaries. This bright red blood carries oxygen and nutrients to the cells. As it moves through the capillaries, carbon dioxide is picked up from the tissues and the blood then contains little oxygen, so it becomes deoxygenated again. It turns a dark red colour. Deoxygenated blood returns to the heart through the systemic veins and empties into the superior vena cava and inferior vena cava, which in turn empties into the right atrium. Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) HEPATIC PORTAL CIRCULATION - the circulatory system of the organs of digestion This circulatory system is responsible for transporting blood from the gastrointestinal tract to the liver. Substances absorbed in the small intestine travel first to the liver to be stored or modified in order to maintain correct nutrient concentrations in the blood. If blood from the digestive organs contains harmful substances, the liver detoxifies it to ensure that they are not carried to the rest of the body and ultimately to the heart. Blood enters the liver from two sources: 1. The hepatic portal vein delivers deoxygenated blood from the gastrointestinal organs. The hepatic portal vein is formed by the union of several veins. They are the: Splenic vein Inferior mesenteric vein Superior mesenteric vein Right and left gastric veins Cystic vein They carry deoxygenated blood to the capillary-like structures in the liver, called sinusoids. This blood is rich with substances absorbed from the gastrointestinal tract. It is monitored and filtered by the liver before it passes into the general circulation. 2. The hepatic artery delivers oxygenated blood from the systemic circulation. At the same time, the liver receives oxygenated blood from the systemic circulation via the hepatic artery. The oxygenated blood mixes with the deoxygenated blood in the sinusoids. Ultimately, all blood leaves the sinusoids of the liver through the hepatic veins, which empty into the inferior vena cava. Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) ARTERIES, ARTERIOLES, CAPILLARIES, VENULES AND VEINS Blood vessels are tubes that carry blood. The vessels form a network around the body. Pumped by the heart, blood circulates through this network, delivering essential supplies and removing waste. The main types of vessels are arteries, veins and capillaries. Each type has a different structure and is shaped to work in a different way. ARTERIES These are the blood vessels that carry blood away from the heart towards the tissues. They vary considerably in size. They have a small lumen (hollow centre) surrounded by a wall consisting of three layers of tissue: 1. 2. 3. Tunica adventitia or outer layer of fibrous tissue Tunica media or middle layer of smooth muscle and elastic tissue Tunica intima or inner layer of squamous epithelium Arteries carry oxygenated blood away from the heart (not pulmonary arteries), the walls are thick, muscular and elastic to withstand the high pressure of arterial blood and there are no valves as blood must flow rapidly under high pressure delivering oxygen. Arterial blood contains a high concentration of nutrients. The oxygenated blood eventually reaches very small arteries called arterioles. ARTERIOLES These are tiny branches of arteries that lead to capillaries. They transport oxygenated blood from arteries to capillaries. They are the main regulators of blood flow and pressure. CAPILLARIES Blood flows from the arteries into arterioles and then finally into capillaries. Capillaries are tiny vessels and they form a vast network that links the smallest arterioles to the smallest venules. Capillary walls are made up of a single layer of endothelial cells sitting on a very thin basement membrane. This thin membrane allows the exchange of substances – nutrients and oxygen are delivered to the cells of the body and at the same time carbon dioxide and waste products are removed. These substances pass through the capillary walls – a process known as capillary exchange. They have a very small lumen. Capillaries connect with larger vessels called venules. Capillaries carry both oxygenated and deoxygenated blood, there are no valves as blood flows under pressure, but it is higher than in veins. Capillaries are able to narrow or widen through the mechanisms of vasodilation and vasoconstriction. VENULES Venules are minute vessels that drain blood from capillaries into veins. Many venules unite to form a vein. Their function is to drain blood from the capillaries into veins to be returned to the heart. Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) VEINS Blood flows through the venules until it reaches larger vessels called veins. These are the blood vessels that carry blood at low pressure away from the tissues and back towards the heart. They are similar in structure to arteries in that they also have three layers of tissue surrounding a large lumen, however, there are differences: Veins carry deoxygenated blood back to the heart (not pulmonary veins), the walls are thinner as there is less muscle and elastic tissue, valves occur at intervals to stop backflow of blood ensuring it flows towards the heart, blood flows under low pressure, venous blood contains a high concentration of waste products and they are situated nearer the surface of the body. GROWTH & REPAIR Process of Blood Clotting Platelets (thrombocytes) contain a variety of substances that promote blood clotting. When a blood vessel is damaged, platelets arriving at the site release serotonin causing the smooth muscle in the wall of the vessel to immediately constrict. This reduces the blood flow through it. The platelets stick to each other and release other substances which attract more platelets to the site. Passing platelets stick to those already at the damaged vessel and they too release their chemicals. Platelets rapidly arrive at the site and quickly form a temporary seal – the platelet plug. Initially the platelet plug is quite loose, but it eventually becomes quite tight as it is reinforced by the blood clotting process. Once the plug is in place, the platelets (thrombocytes) release an enzyme called thromboplastin. Thromboplastin converts prothrombin (a protein present in blood plasma) into thrombin. Vitamin K and calcium are needed for this process. Thrombin then interacts with the soluble plasma protein fibrinogen and converts it into an insoluble substance called fibrin. Fibrin consists of fibrous strands, which forms a network in which the blood cells become trapped and so a blood clot forms. The clot dries out to form a scab, which is like a natural plaster to protect the skin underneath. The function of this process is to prevent blood loss and to prevent the site from becoming infected. Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) DEFINITION OF BLOOD SHUNTING Blood shunting is the changing of blood volume in different areas of the body. The body contains a vast number of many blood vessels and there is not enough blood to fill them all at any one time. Blood is directed to an area of need according to the physical demands of that particular system or organ. Along certain circulatory pathways, such as the intestines, there are points where small arteries have direct connections with veins. Special vessels, called shunt vessels, provide a short cut and allow blood from the artery to have direct access to a vein, bypassing the capillaries in the process. These inter-connections allow for sudden and major diversions of blood volume according to the physical needs of the body. For example, after a meal, blood will circulate around the digestive system to assist with the digestion of food. This is why massage treatments are contraindicated after a heavy meal, as blood would be directed away from the digestive system to the muscles that were being worked on, causing digestive problems. It also explains why we feel tired after eating a heavy meal, as there is less blood supply in other areas of the body. During exercise, blood can be diverted from the intestines to skeletal muscles. To help the body to cool down blood is also diverted to the skin. HOW EXERCISE AFFECTS THE CIRCULATORY SYSTEM A person’s level of fitness can be improved at any age with regular exercise. Some types of exercise are more effective than others for improving the health of the cardiovascular system. Aerobic exercise – this is any activity that works large body muscles, elevates cardiac output and accelerates metabolic rate. Exercise such as brisk walking, running, cycling, crosscountry skiing and swimming are all recommended. Three to five sessions for at least 20 minutes will improve the health of the cardiovascular system. Sustained exercise increases the oxygen demand of the muscles. Whether the demand is met depends primarily on the adequacy of cardiac output and proper functioning of the respiratory system. After several weeks of training, a healthy person increases maximal cardiac output, thereby increasing the maximal rate of oxygen delivery to the tissues. Haemoglobin level increases and skeletal muscles develop more capillary networks, enhancing oxygen delivery. A physically fit person may even exhibit bradycardia i.e. a resting heart rate under 60 beats per minute. A slowly beating heart is more energy efficient than one that beats more rapidly. During strenuous activity, a well-trained athlete can achieve cardiac output double that of a sedentary person, in part because training causes hypertrophy (enlargement) of the heart. Regular exercise also helps to reduce blood pressure, anxiety, depression, control weight and increases the body’s ability to dissolve blood clots. Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) ARTERIES & VEINS OF THE SYSTEMIC CIRCULATION All systemic arteries branch from the aorta. Completing the circuit, all the veins of the systemic circulation drain into the superior vena cava, inferior vena cava, or the coronary sinus, which in turn empties into the right atrium of the heart. AORTA This is the largest artery in the body. Blood leaves the heart via one artery: the aorta. It receives oxygenated blood from the left ventricle and it has five principal divisions: ascending aorta, arch of aorta, descending aorta, thoracic aorta and abdominal aorta. Throughout its length the aorta gives off numerous branches. Some of them are paired i.e. there is a right and left branch of the same name and some are single or unpaired. 1. The right and left coronary arteries are the only branches that arise from the ascending aorta. 2. Three major arteries branch from the arch of the aorta: brachiocephalic artery left common carotid artery left subclavian artery 3. The descending aorta descends downwards behind the heart and towards the trunk. It gives off many paired branches Arteries in the thoracic cavity Bronchial arteries Oesophageal arteries Intercostal arteries Most of the venous blood from the organs in the thoracic cavity is drained into the azygos and hemiazygos vein. Some of the main veins that join them are the bronchial, oesophageal and intercostal veins. Veins in the thoracic cavity Azygos veins Hemiazygos veins Bronchial veins Oesophageal veins Intercostal veins Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) 4. It joins the thoracic aorta and continues to descend through an opening in the diaphragm (aortic hiatus) Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) 5. The abdominal aorta is the continuation of the thoracic aorta. Many arterial branches arise from the abdominal aorta. They supply the abdominal region: Arteries in the abdominal region Left & right phrenic arteries Coeliac artery Superior mesenteric artery Inferior mesenteric artery Renal arteries Ovarian / testicular arteries Left internal & external iliac arteries The coeliac artery divides into three branches: left gastric artery, the splenic artery, the hepatic artery. Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) Venous return from the abdominal organs The inferior vena cava is formed when the right and left common iliac veins join at the level th of the 5 lumbar vertebrae. The veins listed all join the inferior vena cava and their blood is returned to the right atrium of the heart. Veins in the abdominal region Phrenic veins Adrenal veins Renal veins Lumbar veins Hepatic veins Ovarian / testicular veins Left internal & external iliac veins PORTAL CIRCULATION Blood from the remaining organs in the abdominal cavity passes through the liver via the portal circulation before entering the inferior vena cava. Arteries taking blood to liver Veins taking blood from liver Splenic artery Gastric artery Hepatic artery Inferior mesenteric artery Superior mesenteric artery Splenic vein Gastric vein Cystic vein Inferior mesenteric vein Superior mesenteric vein Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) Hepatic veins are very short veins – they leave the posterior surface of the liver and almost immediately join the inferior vena cava. Blood from the systemic circulation returns to the heart via the following three veins: Superior vena cava – deoxygenated blood is emptied into the superior part of the right atrium. It receives blood from veins superior to the diaphragm. These include the head, neck, upper limbs and the thoracic wall. Inferior vena cava – this is the largest vein in the body. It ascends up through the abdomen and thorax and empties its blood into the inferior part of the right atrium. It receives blood from veins inferior to the diaphragm. These include the abdominal viscera, most of the abdominal walls and the lower limbs. Coronary sinus – this begins in the coronary sulcus, a groove which separates the atria and ventricles. It empties its blood into the right atrium. It receives blood from the cardiac veins which drain into the myocardium of the heart. CIRCULATION OF BLOOD TO THE HEAD AND NECK Arterial Supply Carotid Arteries - the blood supplying the head and neck arrives via the common carotid arteries and the vertebral arteries. There are two main carotid arteries, one either side of the neck – the right common carotid artery and the left common carotid artery. As they pass the thyroid, each divides into an internal carotid artery and an external carotid artery. External Carotid Arteries – this artery supplies the superficial tissues of the head and neck, via the following arteries: Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) Arteries to the head and neck Superior thyroid artery Lingual artery Facial artery Occipital artery Superficial temporal artery Maxillary artery Internal Carotid Artery – this is a major contributor to the Circulus arteriosus (circle of Willis) which supplies the greater part of the brain. It also has branches that supply the eyes, forehead and nose. Circulus arteriosus (circle of Willis) – 4 large arteries contribute to its formation: two internal carotid arteries two vertebral arteries – these join to form the basilar artery These arteries are found at the base of the brain. They are part of a complete circle of blood vessels that ensure that the brain has a multiple supply of blood at all times Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) Venous return from head and neck The venous blood from the head and neck is returned by deep and superficial veins. The external jugular veins and the vertebral veins feed into the subclavian vein. The internal jugular veins unite with the subclavian veins and become the brachiocephalic veins. The brachiocephalic veins are situated on each side of the neck. They both join to form the superior vena cava. The superior vena cava drains all the venous blood from the head, neck and upper limbs and carries it to the right atrium of the heart. Veins to the head and neck Middle temporal vein Left occipital vein Left superficial temporal vein Maxillary vein Anterior facial vein Common facial vein Internal jugular veins External jugular vein Posterior external jugular vein Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) CIRCULATION OF BLOOD TO THE PELVIS AND LOWER LIMBS Arterial Supply The abdominal aorta divides at the level of the 4th lumbar vertebrae and the right and left common iliac arteries are formed. Each artery further divides into the internal and external iliac arteries. Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) Arteries of the pelvis and lower limbs Femoral artery Popliteal artery Anterior tibial artery Posterior tibial artery Plantar arch artery Digital arteries Venous return from the lower limbs The veins of the lower limbs are divided into two groups: deep and superficial veins. Blood entering the superficial veins passes to the deep veins through communicating veins. Movement of blood towards the heart is partly dependent on contraction of skeletal muscles. Backward flow is prevented by numerous valves. Deep veins accompany the arteries and their branches and have the same names. They are: Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) Deep veins found in the lower leg Femoral vein Popliteal vein Anterior tibial vein Posterior tibial vein Dorsal venous arch Plantar vein Digital veins The two main superficial veins draining blood from the lower limbs are: Superficial veins found in the lower leg Great saphenous vein Small saphenous vein CIRCULATION OF BLOOD TO THE UPPER LIMBS Arterial Supply The right subclavian artery arises from the brachiocephalic artery; the left subclavian artery branches from the arch of the aorta. They pass behind the clavicles, enter the axillae and become the axillary arteries. Before entering the axilla, each subclavian artery gives off two branches: the vertebral artery which passes up and into the brain, and the internal thoracic artery which supplies the breast area. As they continue down the arm, the axillary artery becomes the brachial artery. The following arteries continue in the lower arm and hand: Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) Arteries in the lower arm Radial artery Ulnar artery Deep and superficial palmar arteries Palmar metacarpal arteries Palmar digital arteries Venous return from the upper limbs The veins of the upper limbs are divided into two groups: deep and superficial veins. The deep veins follow the same course as the arteries and have the same names. They are: Deep veins found in the lower arm Palmar metacarpal veins Deep palmar venous arch Ulnar and radial veins Brachial vein Axillary vein Subclavian vein Christina Lyne Ltd©2014 Aromalyne Training Level 3 Diploma in Aromatherapy (ABC) The superficial veins begin in the hand and consist of the following: Superficial veins found in lower arm Cephalic vein Basilic vein Median vein Median cubital vein Christina Lyne Ltd©2014