* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download The Age-Associated Alterations in Late Diastolic Function in Mice
Heart failure wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Cardiac surgery wikipedia , lookup
Electrocardiography wikipedia , lookup
Aortic stenosis wikipedia , lookup
Myocardial infarction wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Jatene procedure wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Journal of Gerontology: BIOLOGICAL SCIENCES
1997, Vol. 52A, No. 6, B285-B29O
Copyright 1997 by The Gerontological Society of America
The Age-Associated Alterations in Late Diastolic
Function in Mice Are Improved by Caloric Restriction
George E. Taffet,123 Thuy T. Pham,23 and Craig J. Hartley1
Sections of 'Cardiovascular Sciences and 2Geriatrics, Department of Medicine,
and 3Huffington Center on Aging, Baylor College of Medicine, Houston.
Caloric restriction reduces the magnitude of many age-related changes in rodents. Cardiac function is altered with
senescence in mice, rats, and healthy humans. We examined the effects of life-long caloric restriction on diastolic
and systolic cardiac function in situ using Doppler techniques in ad libitum-fed 30- to 32-month-old (AL) and
calorically restricted (CR) 32- to 3S-month-old female B6D2-F, hybrid mice. The heart weight to body weight ratio
was similar in AL (5.74 ± .24 mg/g) and CR (5.68 ± .20 mg/g) mice. Two systolic functional parameters known to
decrease with age in both humans and mice, peak aortic velocity and aortic acceleration, were unchanged by CR
compared to AL. In contrast, diastolic function was altered by caloric restriction. Although left ventricular peak
early filling velocity (E) was not different between CR andAL, peak atrial filling velocity (A) was 50% lower in CR
compared to AL (p < .001). The ratio of early diastolic filling to atrial filling (ElA ratio) was 64% higher in the CR
(2.74 ± .31) than theAL (1.55 ± .07; p = .004). The fraction of ventricular filling due to atrial systole, the atrial filling fraction, was also reduced in CR (.21 ± .04) compared to AL (.36 ± .02; p = .007). These changes occurred in
CR without alteration in E deceleration time, which is consistent with improved diastolic function in CR. Through
mechanisms that remain unknown, lifelong caloric restriction may prevent the age-related impairments in late
diastolic function but does not alter the impairments in systolic or early diastolic cardiac function.
C
ALORIC restriction increases the mean and maximum
life span of rodents. In a recent overview of caloric
restriction, Weindruch (1996) reported that dietary restriction mitigated age-related declines in function in 90% of
the measures assayed. These effects of caloric restriction
included improvements in age-related impairments in glucose tolerance, increases in lymphocyte responsiveness,
relative preservation of muscle mass, etc. However, these
findings have been primarily focused in the areas of
endocrinology and immunology (Masoro, 1993; Weindruch, 1996).
In contrast to the wealth of data relevant to the immune
system, endocrine system, etc., much less is known about
the effects of caloric restriction on the aging cardiovascular
system (Herlihy and Kim, 1994). Furthermore, much of the
data reported is contradictory. For example, in aging animals the effects of caloric restriction on blood pressure or
cardiac hypertrophy are disparate; reports of no changes,
increases, and decreases with caloric restriction exist in the
rat for these parameters (reviewed in Herlihy and Kim,
1994). The functional implications of these cardiovascular
changes induced by caloric restriction are unknown in the
rat. No information is available, to our knowledge, on the
effects of caloric restriction upon cardiovascular function in
the aging mouse.
In the absence of disease, aging alters cardiac function
during both systole and diastole. The observed extent of the
age-related change in systolic function depends upon the
parameter measured. For example, systolic function measured by ejection fraction is well preserved with age. In
contrast, the maximum rates of tension and pressure development decrease with age (Lakatta et al., 1975; Tate et al.,
1990; Lakatta, 1993). Using pulsed Doppler techniques in
people similar to those used below in mice, older humans
have decreased maximum blood flow velocity in the thoracic aorta, and aortic acceleration is also decreased (Kelly
et al., 1989). These changes in aortic velocity are thought
to have minimal functional impact on the older person, but
they provide evidence of mildly impaired contractile function in the aging human heart.
The impact of aging on diastolic function is less modest
and depends little on the parameter reported (Lakatta et al.,
1975; Gerstenblith et al., 1977). Cardiac relaxation slows,
and the extent of filling due to rapid left ventricular relaxation (diastolic suction) decreases (Kitzman et al., 1991).
Perhaps to maintain adequate left ventricular filling, the relative contribution of atrial systole increases and the left
atrium hypertrophies (Miyatake et al., 1984). Noninvasively, with pulsed Doppler ultrasonography, the increase
in reliance upon atrial systole for filling is measured by a
change in the ratio of peak early filling velocity (E) to the
late, atrial component (A). The E/A ratio decreases, or conversely, the atrial filling fraction increases with age in normal healthy humans in several studies (Miyatake et al.,
1984; Spirito and Maron, 1988; Kitzman et al., 1991). We
have found that the same is true in the aged mouse (Taffet
et al., 1996).
The age-associated impairment in diastolic function is
not benign. The E/A ratio and other diastolic functional
parameters correlate strongly with maximum oxygen consumption in normal elders (Vanoverschelde et al., 1993;
Stratton et al., 1994). Furthermore, impaired cardiac diastolic function may put elderly people at risk for congestive
heart failure (Luchi et al., 1991). Diastolic heart failure,
where the ejection of blood is normal and filling is
impaired, is very common among the elderly and lacks
B285
B286
TAFFETETAL.
adequate therapy. Diastolic heart failure is thought to result
from a combination of age- and disease-mediated changes
(Luchi et al., 1991). Therefore, methods to prevent ageassociated diastolic dysfunction, as well as that caused by
disease, are needed.
We took advantage of a newly developed technique to
perform in situ measurements of systolic and diastolic function in ad libitum-fed and calorically restricted old mice.
Caloric restriction resulted in a decrease in the age effects
on cardiac diastolic function, but without modification of
the age-related decrement in systolic function.
METHODS
Animals. — Aged female B6D2-Fi hybrid mice were
shipped from the National Center for Toxicological ReSearch laboratory in Arkansas. They were either ad libitum
fed (AL) or calorically restricted (CR) commencing at 6
weeks of age, shortly after weaning. They were a gift from
the National Institute on Aging and were 30-35 months at
time of study. These animals were reared in a pathogenfree environment, and the CR animals have an appropriately prolonged life span compared with the AL-fed animals. Upon transfer to Baylor College of Medicine, the
dietary status was maintained as was the pathogen-free
environment in a high efficiency particulate air-filtered cage
rack. The animals were continued on the same autoclaved
ad libitum or restricted diets and were studied 2-4 weeks
after arrival.
Doppler studies. — Mice were anesthetized by an intraperitoneal injection with a rodent anesthesia mixture (1.4
mg/ml acepromazine, 8.6 mg/ml xylazine, 42.8 mg/ml
ketamine) at a dose of 0.5 ul/g body weight. They were
taped to a temperature-controlled laminated plastic board
with copper electrodes placed such that all four limb leads
could be used for electrocardiographic monitoring. Body
fur at the left lower sternal border was clipped lightly, and
the skin in that area was wetted with warm water to
improve sound transmission. A 10-MHz pulsed Doppler
probe was positioned at the xiphoid applying only minimal
pressure. The pulsed Doppler range gate was set at 4-7 mm
deep to obtain optimal signals from the left ventricular
inflow and outflow tracts. An electrocardiogram (ECG) timing signal was superimposed on the Doppler display using
an R-wave trigger producing a dashed vertical line on the
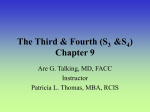
spectral display (see Figure 1). Repeated measurements
were made from each animal to allow for observation at
different heart rates and to ascertain the reproducibility of
the measurements.
Doppler outputs were captured on a personal computer
using a Computer Eyes 1024 Video Digitizing Board and
Computer Eyes Video Capture software (Digital Vision,
Dedham, MA). The images were converted to Macintoshcompatible TIFF files and were analyzed off-line using the
NIH Image program. For each study 3-6 beats were analyzed. Data were quantified in a Lotus 123 spreadsheet.
The systolic parameters shown in Table 2 were utilized
to evaluate the aortic outflow patterns (see Figure 1 for typical pulsed Doppler generated waveforms). The peak aortic
velocity was determined by measuring the peak Doppler
shift frequency in KHz multiplied by 7.5 to calculate velocity in cm/sec at 10 MHz (Taffet et al., 1996). Aortic acceleration is calculated by dividing peak aortic velocity by the
interval from time of the start of the flow to the time of
peak velocity.
The following diastolic parameters shown in Table 3
were utilized: peak early (E) filling velocity; peak late filling velocity due to atrial contraction (peak A velocity); the
E deceleration time, a linear extrapolation of the declining
flow velocities from the time of peak flow velocity to the
baseline (Nishimura et al., 1989a; Holt et al., 1995); normalized filling rate, calculated by dividing the peak E filling velocity by the area under the E wave (Bowman et al.,
1988); the E/A ratio, the ratio of peak E and A velocities;
and the atrial filling fraction, the ratio of the area under the
A wave to the sum of the areas of the A wave and E wave.
Statistics. — Student's unpaired /-tests were used to
determine if measurements were different. For all studies,
p < .05 was used to determine statistical significance. Data
are expressed as mean ± SEM.
The number of animals in this study was relatively small,
so limitations in statistical power are an important consideration. Because we found statistical differences between the
groups, the impact of the small sample size must be interpreted in light of measurements for which no differences
were found. For the systolic measurement that was not statistically different between the groups, but had the largest
difference between AL and CR values (aortic acceleration),
84 animals would be needed in each group if the means and
standard deviations remained unchanged to have an 80%
probability of finding a statistically significant difference at
p < .05. This magnitude of change is unlikely to be physiologically important, and we feel that the limited number of
animals we studied allowed for determination of major differences between the groups.
RESULTS
The body weights of the CR old animals were 25% less
than the AL-fed old animals. Heart weights were also
decreased in CR compared to AL, but the heart weight to
body weight ratio was approximately the same in AL and
CR (Table 1).
Left ventricular systolic function (Table 2) was examined
by monitoring left ventricular outflow. There was no difference in peak aortic velocity between AL and CR. Ejection
time was not significantly altered by caloric restriction.
Aortic acceleration was also similar in the two groups.
Table 1. Group Characteristics
Age (months)
Body weight (g)
Heart weight (mg)
Heart/body ratio (mg/g)
AL
(n = 6)
CR
(n = 6)
p- value
30-32
31.6±0.8
178 ± 14
5.74 ± .24
32-35
23.6 ± 1.0
134 ± 7
5.68 ± .20
<.OO1
.018
.85
Note: Data are shown as mean ± SE.
B287
CALORIC RESTRICTION AND CARDIAC FUNCTION
Table 2. Outflow Measurements
AL
(« = 6)
Peak aortic velocity
(cm/sec, 92.2 ± 5)
Ejection time (msec, 83 ± 2)
Aortic acceleration
(cm/sec2, 5454 ± 430)
Heart rate (beats/min, 265 ± 17)
73.6 ± 4
89 ±5
3134 ±327
257 ±17
CR
(« = 6)
Table 3. Transmitral Measurements
AL
CR
(n = 6)
(n = 6)
p- value
52 ±4
50 ±2
.66
43 ±3
38 ±2
.20
16.2 ± 1.0
18.1 ±0.8
.17
34 ±3
1.55 ±.07
16 ±2
2.74 ±.31
<.001
.004
.36 ± .02
.21 ±.04
.007
p- value
71.1 ± 4
83 ± 5
.67
.42
3505 ± 363
254 ± 29
.47
.93
Peak E velocity
(cm/sec, 63 ± 2)
E deceleration time
(msec, 40 ± 1)
Normalized filling rate
(SV/sec, 21.0 ±0.4)
Notes: Values in parentheses are "typical young mouse values." Data
are shown as mean ± SE.
Peak A velocity
(cm/sec, 19 ± 1)
E/A ratio (3.45 ± .28)
Atrial filling fraction
(.23 ± .02)
Typical velocity waveforms are shown in Figure 1. Importantly, there were no differences in heart rate between AL
and CR under anesthesia during the studies of aortic and
transmitral flow.
Diastolic function was significantly modified by lifelong
caloric restriction (Table 3). Typical transmitral Dopplergerterated waveforms are shown in Figure 1. Peak E velocities, average deceleration times, and normalized peak filling
rates were not different between AL and CR groups. In contrast to the early diastolic measurements, late diastolic
function was significantly altered by the caloric restriction.
Peak A velocity was decreased 50%, and atrial filling fraction was decreased 40% in the CR compared to AL. The
E/A ratio was increased in the CR compared to AL, consistent with improved diastolic function because it occurred
without any change in E deceleration time (Giannuzzi et
al., 1996).
Notes: Values in parentheses are "typical young mouse values." Data
are shown as mean ± SE. SV/sec = stroke volumes per second.
DISCUSSION
These data provide evidence that lifelong caloric restriction will prevent some, but not all, of the characteristic
aging changes in cardiac function as assessed noninvasively
by pulsed Doppler velocimetry. Left ventricular systolic
function, as measured by peak aortic velocity and aortic
acceleration, and left ventricular filling, as measured by
mitral E/A ratio, are both compromised with age (Taffet et
al., 1996). Because only diastolic function was modified by
caloric restriction, the systolic and diastolic changes likely
represent independent processes that occur with aging.
Systolic function. — Systolic function is considered to
be relatively well preserved with age. This is primarily
because left ventricular ejection fraction, the most commonly used measure of systolic function, does not change
with age (Luchi et al., 1991). Similarly, isolated rat cardiac
muscle does not reveal an effect of age on the ability to
develop tension when studied at low stimulation rates
(Lakatta et al., 1975; Spurgeon et al., 1983; Tate et al.,
1990). In contrast, more recent data from experiments performed with senescent rat papillary muscles studied at more
rapid stimulation rates revealed a significant age-related
decline in the ability to generate force (Jiang et al., 1993).
Furthermore, in all the studies where cardiac muscle isolated from old animals generated force adequately, the time
to peak tension was uniformly prolonged (Lakatta et al.,
1975; Tate et al., 1990). Slower development of tension or
Rt
4
\ll
il
Aortic
i
1
1
il
ip
1I
ti
0.5 seconds
Restricted (CR)
- 90 -
• 60 • 30 •
'ip
l
i
'i
il
il
i l - 30 -
I
\
i
0 -
I x JHi JH
•
*
- 60 -
cm/s
cm/s
-
*
Old, Caloncally
Old, Fed
Ad-libitum (AL)
Young
Control
0.5 seconds
; P
«.
IB
*4,
• B ••
JO
|1
•—
»
j|B
0.6 soconds
»
- 90 -
E
V
,'
1
E/A4.6
- 60 - E
Mitral
li,LLLi
I
i Aj
i E/A-1.6 j
•
I
j
I
| {
- 30 cm/s
-
0 .
|
- 60 -
E
|
E/A-3.7
.
- 30 -
|JL JUL.IJ
cm/s
-
0 '
I V l.|» JL_ A
Figure 1. Typical aortic and transmitral Doppler waveforms from young
(a reference control), AL-fed old and CR old mice. The first row displays
aortic Doppler images, the second row displays transmitral Doppler. The
(P) represents peak of aortic flow. The E/A shown is the ratio of peak
velocities (heights) of the E wave to the A wave. The vertical dashed line
represents the timing of the R wave from the ECG.
pressure would result in decreased aortic acceleration in the
intact animal, and decreases in the rate of aortic acceleration comparable to those we report occur with aging in
humans (Kelly et al., 1989). This age-associated change in
systolic function was not modified by lifelong caloric
restriction; however, the impact of the decrease in systolic
function is likely to be small.
Myosin isoyme changes have been implicated in the
slower development of tension in aging rat hearts. With
aging in the rat, slow myosin predominates; the slow (3myosin heavy chain cycles and develops force less rapidly.
Slow myosin is also increased after short-term caloric
restriction of young animals (Swoap et al., 1994), but the
effects of lifelong caloric restriction are uncertain. Potentially, the CR old mouse heart could have an even greater
proportion of fi-myosin than the AL-fed old mouse. Nevertheless, if the effects of short-term caloric restriction persist
in the mouse, then one would not expect caloric restriction
B288
TAFFETETAL.
to improve this aspect of the decreased cardiac function
with aging, consistent with our findings.
Diastolic function. — Peak E filling velocity is decreased
with aging (Taffet et al., 1996), and this important measure
of early diastolic filling was not improved in CR mice. In
contrast, caloric restriction profoundly decreased peak A
velocity, thus improving the E/A ratio. In humans, the
altered filling of the left ventricle with age, as measured by
E/A ratio, has been attributed to impaired cardiac diastolic
function (Spirito and Maron, 1988; Kitzman et al., 1991).
However, peak E filling velocity may also be reduced by
decreases in filling pressures, increased left ventricular wall
thickness or stiffness, or regional heterogeneity in function
among the left ventricular segments (Sys and Brutsaert,
1995). Alterations in active cardiac relaxation impact early
diastolic parameters, including peak E velocity, more
than late diastolic measurements like peak A velocity
(Nishimura et al., 1989b). With aging, there is ample evidence implicating slowed cardiac relaxation and altered
cardiac calcium handling for the impairment in diastolic
function derived from studies in the senescent rat (Tate et
al., 1990; Taffet and Tate, 1993). Consistent with the contribution of relaxation to the determination of peak E velocity,
thyroxine-treated mice had augmented sarcoplasmic reticulum calcium uptake and a significant increase in peak E
velocity (Taffet et al., 1996). The specific changes induced
by caloric restriction in the senescent mouse remain uncertain; however, they would be unlikely to include profound
effects on cardiac sarcoplasmic reticulum calcium handling
because there was no effect of CR on early diastolic function. Peak E velocity was lower than typical young mouse
values in both AL and CR.
In contrast to the lack of effect of CR on systolic and
early diastolic function, caloric restriction improved late
diastolic function as determined by peak A velocity and
atrial filling fraction. The contribution of the A wave to left
ventricular filling was significantly decreased in the CR
mice compared to the AL mice. Though it is tempting to
implicate the inadequacy of filling during early diastole in
the AL (Spirito and Maron, 1988), there are other important
determinants of the magnitude of the A wave that need be
considered. Modification of left atrial compliance or size by
age will alter A wave velocity remarkably because a more
compliant left atrium may act as a better reservoir for pulmonary venous return from the lung, but will not transmit
negative pressures generated by the left ventricle (Sun et
al., 1995). Diet restriction could therefore result in decreased left atrial hypertrophy or a stiffer atrium resulting
in a smaller A wave.
Alternatively, the increase in E/A ratio observed in CR
could actually reflect worsening cardiac function. In
humans with congestive heart failure followed serially,
worsening cardiac function may be associated with normalization of E/A ratio and a "restrictive pattern" characterized
by foreshortening of the E deceleration time (Giannuzzi et
al., 1996). It is unlikely that CR improved the E/A ratio
because of further stiffening of the left ventricle as the E
deceleration time was not different between CR and AL
mice (Table 3). Furthermore, collagen content increases
with age in the rat heart and correlates with increasing stiffness; lifelong caloric restriction decreases the cardiac connective tissue content (Berg and Simms, 1960; Maeda et al.,
1985; Thomas et al., 1992). Nevertheless, serial measurements of cardiac function in aging CR and AL mice would
more definitively rule out this possibility.
Role of cardiac hypertrophy in the diastolic dysfunction
of aging. — Cardiac hypertrophy, in response to increasing
afterload, has been implicated in causing the age-related
impairments in diastolic function (Sartori et al., 1987;
Lakatta, 1993). The data in Table 1 might be used to support or refute this hypothesis. Heart weight is clearly
greater in AL than CR mice, but the differences disappear
when heart weight is corrected for body weight. However,
CR is known to influence body composition as well as body
weight. For example, Masoro et al. (1992) found that 24month-old rats had decreases in lean body weight that were
much more modest than losses in total body weight after
lifelong CR. Therefore, if we corrected heart weight for
lean body weight, then the extent of the hypertrophy in CR
would be less than in AL. A similar conclusion might be
drawn if heart weight was corrected for tibial length (Yin et
al., 1982). We conclude that the extent and type of hypertrophy may still play a role in the impaired diastolic function associated with aging, and, depending on definition,
the extent of hypertrophy may be decreased after CR. This
finding is contrary to what has been reported in the CR old
rat (Herlihy and Kim, 1994).
Study limitations. — Most of our information on the
aging cardiovascular system is derived from studies of relatively large animals — the rat, dog, or human. Little is available from the mouse. For example, blood pressure measurement, a key to understanding the aging changes in the heart,
is a technically demanding undertaking in the mouse (Krege
et al., 1995). Furthermore, we are unaware of any technique
that will permit the noninvasive measurement of diastolic
blood pressure in the mouse. We have been unable to obtain
noninvasive determinations of blood pressure without warming the mouse, a manipulation that we have shown alters
cardiac function profoundly (Hartley et al., 1995). Because
Lakatta (1993) has hypothesized that the age-related increase in systolic blood pressure may be the primary event
triggering the maladaptive changes that ultimately result in
impaired cardiac diastolic function, an understanding of the
effects of caloric restriction on age-related changes in blood
pressure and cardiac function is important.
We did not measure systolic and diastolic function
directly in these studies. The optimal measurements of cardiac diastolic function are disputed, and even the definition
of diastolic function is under question (Sys and Brutsaert,
1995). The measurement of the E/A ratio(s) is accepted as
one of the best measures of diastolic function in situ. However, there are important other factors that can alter E/A
ratio. As noted above, these include heart rate, afterload,
preload, left ventricular mass, contractility, and nonuniformity of relaxation (Nishimura et al., 1989a, 1989b). In
healthy humans, when all these factors are taken into
account, age is still the strongest correlate of peak E veloc-
CALORIC RESTRICTION AND CARDIAC FUNCTION
ity and E/A ratio (Kitzman et al., 1991). Furthermore, the
peak E velocity and E/A ratio reflect cardiac diastolic function measured with more invasive techniques (Kitzman et
al., 1991).
Our measurements were made with the animals under
anesthesia, not in the conscious state. The combination of
anesthetic used lowers heart rate in the mouse (Taffet et al.,
1996), but heart rate under anesthesia was not different
between the groups. We have no information on the heart
rate or loading of these hearts in vivo. Whether the relationships between E/A ratio and heart rate, afterload, preload,
left ventricular mass, contractility, and nonuniformity are
preserved in the aging mouse, modified by CR, or significantly altered by the anesthetic are unknown.
We studied animals only after they had been subjected to
lifelong caloric restriction. The potential impact of a shortterm change in caloric intake for older animals is an exciting possibility that is not addressed by our findings. Because the methods utilized herein are noninvasive, the
ability to perform serial studies to document the timing of
the developing impairment in function with aging and
improvement with CR should be possible.
Finally, our data are recorded without the benefit of
visual guidance. We know that sampling from different
locations within the heart may alter the results. The normalized filling rate is essentially independent of sampling site
and reflects the early filling of the ventricle. As was seen
for peak E velocity, the normalized filling rate was not different between the AL and the CR (Table 3), giving us confidence that there was no systematic effect of sampling
upon our transmitral data (Bowman et al., 1988).
Implications. — Caloric restriction significantly modifies
diastolic function of the aging heart. We are unsure if the
rate of myocardial relaxation was altered, if the passive filling properties of the left ventricle were affected, or if the
left atrial function was modified. All of these changes and
perhaps others could result in the observed effects on transmitral flow produced by caloric restriction. Discrimination
between these possible changes is an important issue and is
under study. Nevertheless, caloric restriction now appears
to alter another hallmark of aging, the increased dependence on atrial systole for left ventricular filling. Dietary
restriction does not alter two other aging changes, the
decreased systolic function and the decrease in early diastolic filling. Whether other interventions can modify these
two processes remains uncertain. Caloric restriction appears to retard aging changes in many systems; the mechanism of this manipulation remains unclear. The protean
benefits of caloric restriction in rodents are seen in other
species, but it is possible that the specific age-related
changes in the cardiovascular system of the mouse and rat
are different.
ACKNOWLEDGMENTS
The investigators gratefully acknowledge the support of National Institute on Aging Grant RO1 AG-13251; National Institutes of Health Grants
SB1R HL52364, HL22512, and HL13870; and the Texas Advanced Technology Program.
B289
Address correspondence to Dr. George Taffet, Huffington Center on
Aging M320, Baylor College of Medicine, One Baylor Plaza, Houston,
TX 77030-3498.
REFERENCES
Berg, B.N.; Simms, H.S. Nutrition and longevity in the rat: longevity and
onset of disease with different levels of food intake. J. Nutr. 71:
255-263; 1960.
Bowman, L.K.; Lee, F.A.; Jaffe, C.C.; Materra, J.; Wackers, F.J. Th.;
Zaret, B.L. Peak filling rate normalized to mitral stroke volume: a new
Doppler echocardiographic filling index validated by radionuclide
angiographic techniques. J. Am. Coll. Cardiol. 12:937-943; 1988.
Gerstenblith, G.; Frederiksen, J.; Yin, F.C.P.; Fortuin, N.J.; Lakatta, E.G.;
Weisfeldt, M.L. Echocardiographic assessment of a normal adult aging
population. Circulation 56:273-277; 1977.
Giannuzzi, P.; Temporelli, PL.; Bosimini, E.; Silva, P.; Imparato, A.;
Corra, U.; Galli, M.; Giordano, A- Independent and incremental prognostic value of Doppler-derived mitral deceleration time of early filling
in both symptomatic and asymptomatic patients with left ventricular
dysfunction. J. Am. Coll. Cardiol. 28:383-390; 1996.
Hartley, C.J.; Michael, L.H.; Entman, M.L. Noninvasive measurement of
ascending aortic blood velocity in mice. Am. J. Physiol. 268:H499H505; 1995.
Herlihy, J.T.; Kim, S.-W. Modulation of the aging cardiovascular system
by dietary restriction. In: Yu, B.P., ed. Modulation of aging process by
dietary restriction. Boca Raton, FL: CRC Press, 1994:57-87.
Hoit, B.D.; Houry, S.F.; Kranias, E.G.; Ball, N.; Walsh, R.A. In vivo
echocardiographic detection of enhanced left ventricular function
in gene-targeted mice with phospholamban deficiency. Circ. Res.
77:632-637; 1995.
Jiang, M.T.; Moffat, M.T.; Narayanan, N. Age related alterations in the
phosphorylation of sarcoplasmic reticulum and myofibrillar proteins
and diminished contractile response to isoproterenol in intact rat ventricle. Circ. Res. 72:102-111; 1993.
Kelly, R.; Hayward, C ; Avolio, A.; O'Rourke, M. Noninvasive determination of age-related changes in the human arterial pulse. Circulation
80:1562-1569; 1989.
Kitzman, D.W.; Sheikh, K.H.; Beere, P.A.; Philips, J.L.; Higginbotham,
M.B. Age-related alterations of Doppler left ventricular filling indexes
in normal subjects are independent of left ventricular mass, heart rate,
contractility and loading conditions. J. Am. Coll. Cardiol. 18:12431250; 1991.
Krege, J.H.; Hodgin, J.B.; Hagaman, J.R.; Smithies, O. A noninvasive
computerized tail-cuff system for measuring blood pressure in mice.
Hypertension 25:1111-1115; 1995.
Lakatta, E.G. Cardiovascular regulatory mechanisms in advanced age.
Physiol. Rev. 73:413^67; 1993.
Lakatta, E.G.; Gerstenblith, G.; Angell, C.S.; Shock, N.W.; Weisfeldt,
M.L. Prolonged contraction duration in aged myocardium. J. Clin.
Invest. 55:61-68; 1975.
Luchi, R.J.; Taffet, G.E.; Teasdale, T.A. Congestive heart failure in the
elderly. J. Am. Geriatr. Soc. 39:810-825; 1991.
Maeda, H.; Gleiser, C.A.; Masoro, E.J.; Murata, I.; McMahan, C.A.; Yu,
B.P. Nutritional influences on aging of Fischer 344 rats. II. Pathology.
J.Gerontol. 40:671-688; 1985.
Masoro, E.J. Dietary restriction and aging. J. Am. Geriatr. Soc. 41:
994-999; 1993.
Masoro, E.J.; McCarter, R.J.; Katz, M.S.; McMahan, C.A. Dietary restriction alters characteristics of glucose fuel use. J. Gerontol. Biol. Sci.
47:B202-B209; 1992.
Miyatake, K.; Okamoto, M.; Kinoshita, N.; Owa, M.; Nakasone, I.; Sakakibara, H.; Nimura, Y. Augmentation of atrial contribution to left ventricular inflow with aging as assessed by intracardiac Doppler flowmetry. Am. J. Cardiol. 53:586-589; 1984.
Nishimura, R.A.; Housmans, PR.; Hatle, L.K.; Tajik, A.J. Assessment of
diastolic function of the heart: background and current applications of
Doppler echocardiography. Part I. Physiologic and pathophysiologic
features. Mayo Clin. Proc. 64:71-81; 1989a.
Nishimura, R.A.; Housmans, PR.; Hatle, L.K.; Tajik, A.J. Assessment of
diastolic function of the heart: background and current applications of
Doppler echocardiography. Part II. Clinical studies. Mayo Clin. Proc.
64:181-204; 1989b.
B290
TAFFETETAL.
Sartori, M.P.; Quinones, M.A.; Kuo, L.C. Relation of Doppler-derived left
ventricular filling parameters to age and radius/thickness ratio in normal and pathologic states. Am. J. Cardiol. 59:1179-1182; 1987.
Spirits, P.; Maron, B.J. Influence of aging on Doppler echocardiographic
indices of left ventricular diastolic function. Br. Heart J. 59:672-679;
1988.
Spurgeon, H.A.; Steinbach, M.F.; Lakatta, E.G. Chronic exercise prevents
age-related changes in rat cardiac contraction. Am. J. Physiol.
244:H5I3-H518; 1983.
Stratton, J.R.; Levy, W.C.; Cerqueria, M.D.; Schwartz, R.S.; Abrass, I.B.
Cardiovascular responses to exercise: effects of aging and exercise
training in healthy men. Circulation 89:1648-1655; 1994.
Sun, Y.; Sjoberg, B.J.; Ask, P.; Loyd, D.; Wranne, B. Mathematical model
that characterizes transmitral and pulmonary venous flow velocity patterns. Am. J. Physiol. 268:H476-H489; 1995.
Swoap S.J.; Haddad, F.; Bodell, P.; Baldwin, K.M. Effect of chronic
energy deprivation on cardiac thyroid hormone receptor and myosin
isoform expression. Am. J. Physiol. 266:E254-E260; 1994.
Sys, S.U.; Brutsaert, D.L. Diagnostic significance of impaired LV systolic
relaxation in heart failure. Circulation 92:3377-3380; 1995.
Taffet, G.E.; Tate, C.A. CaATPase content is lower in cardiac sarcoplasmic
reticulum isolated from old rats. Am. J. Physiol. 264:H1609-H1614;
1993.
Taffet, G.E.; Hartley, C.J.; Wen, X.; Pham, T.; Michael, L.H.; Entman,
M.L. Noninvasive indexes of cardiac systolic and diastolic function in
hyperthyroid and senescent mouse. Am. J. Physiol. 270:H2204H2209; 1996.
Tate, C.A.; Taffet, G.E.; Hudson, E.K.; Blaylock, S.L.; McBride, R.P.;
Michael, L.H. Enhanced calcium uptake of cardiac sarcoplasmic reticulum in exercise-trained old rats. Am. J. Physiol. 258:H431-H435;
1990.
Thomas, D.P.; McCormick, R.J.; Zimmerman, S.D.; Vadlamudi, R.K.;
Gosselin, L.E. Aging- and training-induced alterations in collagen
characteristics of rat left ventricle and papillary muscle. Am. J. Physiol. 263:H778-H783; 1992.
Vanoverschelde, J.J.; Essamri, B.; Vanbutsele, R.; d'Hondt, A.; Cosyns,
J.R.; Detry, J.R.; Melin, J.A. Contribution of left ventricular diastolic
function to exercise capacity in normal subjects. J. Appl. Physiol.
74:2225-2233; 1993.
Weindruch, R. Caloric restriction and aging. Sci. Am. 40:46-52; 1996.
Yin, F.C.; Spurgeon, H.A.; Rakusan, K.; Weisfeldt, M.L.; Lakatta, E.G.
Use of tibial length to quantify cardiac hypertrophy: application in the
aging rat. Am. J. Physiol. 243:H941-H947; 1982.
Received June 28, 1996
Accepted June 27, 1997
Reach the best in the field by
advertising in The Gerontologist
for academic and research position openings.
To place ads by phone, fax, or mail, contact:
Elizabeth Borgen
Director of Advertising
The Gerontological Society of America
Suite 350
1275 K Street NW
Washington, DC 20005
202/842-1275 (Tel) 202/842-1150 (Fax) [email protected] (Email)