* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download GENERAL INTRODUCTION Bacillus anthracis
Bacterial morphological plasticity wikipedia , lookup
Human microbiota wikipedia , lookup
Neonatal infection wikipedia , lookup
Molecular mimicry wikipedia , lookup
Hepatitis B wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Infection control wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Bioterrorism wikipedia , lookup
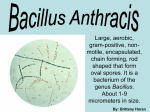
Chapter 1: General Introduction GENERAL INTRODUCTION Bacillus anthracis (First bacterium conclusively demonstrated to cause disease in 1876 - by Robert Koch) TAXONOMY Kingdom : Bacteria Phylum : Firmicutes Class : Bacilli Order : Bacillales Family : Bacillaceae Genus : Bacillus Species : anthracis BASIC FACTS • Bacillus anthracis causes anthrax, a deadly zoonotic disease, usually transmitted from animals to human hosts under natural conditions. • Rod-shaped. • Monomorphic. • Endospore-forming, remains viable in soil and animal products for decades. • Gram-positive. • Aerobic respiration. • Exotoxin producing. • Grows best at 24-40 °C. • Incubation period: 1 to 15 days. • Causes three forms of anthrax: cutaneous, gastrointestinal, inhalational. 1 Chapter 1: General Introduction 1. 1 ANTHRAX Anthrax is an acute disease caused by Bacillus anthracis, a Gram positive, sporeforming bacterial pathogen of both humans and animals (Dixon et al., 1999; Mock and Fouet, 2001). The bacilli are covered by an anti-phagocytic, polyglutamic capsule that helps to evade host immunity and mediates the early invasive stage of infection (Mock and Fouet, 2001). Virulent B. anthracis harbors two plasmids, designated pXO1 and pXO2 (Mikesell et al., 1983). The pXO1 plasmid contains a 44.8-kb pathogenicity island that carries the three toxin genes, pagA, lef and cya encoding protective antigen (PA), lethal factor (LF) and edema factor (EF), respectively (Okinaka et al., 1999). The pXO2 plasmid carries three capsule genes, capA, capB, and capC, encoding bacterial capsule and a gene (dep) associated with depolymerization of the capsule (Koehler, 2002). Thus, the anthrax toxins are secreted as three distinct proteins, namely protective antigen (PA), lethal factor (LF) and edema factor (EF). Vegetative B. anthracis cells produce two binary exotoxins, composed of an A (enzymatically active) protein and a B (binding protein). PA acts as B component and combines with EF and LF to form the edema toxin (ETx) and lethal toxin (LTx), respectively (Singh et al., 1999). LF is a zinc metalloprotease that inactivates mitogen-activated protein kinase kinases, MAPKK (Duesbery et al., 1998). The cleavage of MAPKKs prevents activation of p38 mitogen-activated protein kinase (MAPK), which subsequently prevents the induction of certain NFĸB target genes including genes necessary to prevent apoptosis of activated macrophages (Park et al., 2002). NF-ĸB activation is also important for the upregulation of cytokine genes involved in early innate immune responses (Gao et al., 2002). EF is an adenylate cyclase that increases intracellular cyclic AMP (cAMP) levels in susceptible cells. ETx alters water homeostasis and is responsible for the edema that frequently occurs in patients with B. anthracis infection (Dixon et al., 1999; Tippetts and Robertson, 1988; Ulmer et al., 2003). By increasing cAMP concentration in neutrophils, ETx inhibits phagocytosis and blocks particulate as well as phorbol myristate acetate-induced respiratory burst responses (O'Brien et al., 1985). ETx also differentially regulates macrophage responsiveness to lipopolysaccharide-induced production of tumor necrosis factor alpha (TNF-α) and interleukin-6 (IL-6) (Hoover et al., 1994). 2 Chapter 1: General Introduction 1.1.1 History of Bacillus anthracis: In 1950, Casimir Davaine, a French physician and Pierre Francois Olive Rayer, a French dermatologist discovered certain microorganisms (B. anthracis) in the blood of diseased and dying sheep (Tomes, 1999). In 1863 Davaine demonstrated that the anthrax bacillus could be directly transmitted from one animal to another. He could identify the causative organism but was unaware of its true etiology. In 1876, Robert Koch, a German microbiologist researched the etiology of B. anthracis, and discovered its ability to produce "resting spores" that could stay alive in the soil for a long period of time to serve as a future source of infection (Theodorides, 1994). The species name anthracis is from the Greek anthrakis, meaning "coal" and referring to the most common form of the disease, cutaneous anthrax, in which large, black skin lesions are formed. 1.1.2 Pathogenicity of Bacillus anthracis: Anthrax infection can occur in three forms: cutaneous (skin), inhalational (Pulmonary), and gastrointestinal. Cutaneous (on the skin) anthrax infection in humans shows up as a boil-like skin lesion that eventually forms an ulcer with a black center (eschar). The black eschar often shows up as a large, painless necrotic ulcer (beginning as an irritating and itchy skin lesion or blister that is dark and usually concentrated as a black dot, somewhat resembling bread mold) at the site of infection. In general, cutaneous infections form within the site of spore penetration between 2 and 5 days after exposure. Unlike bruises or most other lesions, cutaneous anthrax infections normally do not cause pain. Respiratory infection in humans initially presents with cold or flu-like symptom for several days, followed by severe (and often fatal) respiratory collapse. Historical, mortality was 92%, but, it can be reduced significantly if treated early as only 45% mortality was observed during the 2001 anthrax attack in USA. Gastrointestinal infection in humans is most often caused by eating anthrax-infected meat and is characterized by serious gastrointestinal difficulty, vomiting of blood, severe diarrhea, acute inflammation of the intestinal tract, and loss of appetite. Some lesions have been found in the intestines and in the mouth and throat. After the bacterium invades the bowel system, it spreads through the bloodstream throughout the body, making even more toxins on the way. This form of anthrax is the rarest form. 3 Chapter 1: General Introduction 1.2 MODE OF ACTION OF BACILLUS ANTHRACIS: The bacterium normally rests in endospore form in the soil, and can survive for decades in this state. B. anthracis spores enter the body through lungs, skin lesion or gastrointestinal route and germinate to yield vegetative form. In case of cutaneous infections, B. anthracis comes into contact with a skin lesion, or cut. In inhalational cases, infection of herbivores (and occasionally humans) occurs via inhalational route and normally proceeds when spores are inhaled, and transported through the air passages into the tiny air particles sacs (alveoli) in the lungs. Herbivores are often infected whilst grazing or browsing, especially when eating rough, irritant, or spiky vegetation: the vegetation has been hypothesized to cause wounds within the gastrointestinal tract permitting entry of the bacterial endospores into the tissues (though this has not been proven) and causes gastrointestinal anthrax. The lethality of the anthrax disease owes itself to the bacterium's two principal virulence factors: (i) the poly-D-glutamic acid capsule, which protects the bacterium from phagocytosis by host neutrophils, and (ii) the tripartite protein toxin, called anthrax toxin. Once ingested or placed in an open wound, the bacterium begins multiplying inside the animal or human and typically kills the host within a few days or weeks. The endospores germinate at the site of entry into the tissues and then spread via the circulation to the lymphatics, where the bacteria multiply. The spores are then picked up by scavenger cells (macrophages) and are transported through small vessels (lymphatics) to the lympnodes. Once in the lymph nodes, the spores germinate into active bacilli that multiply and eventually burst the macrophages, releasing many more bacilli into the bloodstream to be transferred to the entire body. Once in the blood stream, these bacilli release three proteins named lethal factor, edema factor, and protective antigen. All three are non-toxic by themselves, but the combination is incredibly lethal to humans. Protective antigen combines with these other two factors LF and EF to form lethal toxin and edema toxin, respectively. These toxins are the primary agents of tissue destruction, bleeding and death of the host (Pimental et al., 2004; Suffin et al., 1978). In clinical cases as infection progresses inside the host body, fatal bacteremia develops and the vegetative bacilli can reach the concentrations upto 109cells/mL in the blood (Smith, 2000). The LF and EF enter into the cell through protective antigen. Protective antigen binds to two surface receptors on the host cell. A cell protease then cleaves PA into 4 Chapter 1: General Introduction two fragments: PA20 and PA63. PA20 dissociates into the extracellular medium, playing no further role in the toxic cycle. PA63 then oligomerizes with six other PA63 fragments forming a heptameric ring-shaped structure named a prepore. It has been well demonstrated how the PA63 pore allows the EF and LF into the cytoplasm with its very small lumen. The lumen on the PA63 pore is only 15 Å (1.5 nm) across, which is much smaller than the diameter of LF or EF. Translocation occurs through a series of events which begins in the endosome as it acidifies. LF and EF are pH sensitive, and as the pH drops, their structures lose stability. Below a pH of 6.0 (the pH in an endosome), both LF and EF become disordered molten globules. When a molecule is in this conformation, the N-terminus is freed and drawn into the pore by the proton gradient and positive transmembrane potential. A ring of seven phenylalanines at the mouth endosome side of the pore (phenylalanine clamp) assists in the unfolding of LF or EF by interacting with the hydrophobic residues found in LF or EF. The proton gradient then begins to lace the protein though the pore. The lacing mechanism is driven by the gradient, but requires the phenylalanine clamp for a ratcheting motion. The first 250 residues of EF and LF have an irregular alternating sequence of basic, acidic, and hydrophobic residues. The interplay between the phenylalanine clamp and the protonation state causes a ratcheting effect that drives the protein though until enough has crossed into the cytoplasm to drag the rest through the pore as the N-terminus refolds (Pimental et al., 2004; Suffin et al., 1978). Edema factor is a calmodulin-dependent adenylate cyclase. Adenylate cyclase catalyzes and pyrophosphate. the The conversion of complexation ATP into cyclic of AMP (cAMP) adenylate cyclase with calmodulin removes calmodulin from stimulating calcium-triggered signaling, thus inhibiting the immune response. To be specific, LF inactivates neutrophils (a type of phagocytic cell) by the process just described so that they cannot phagocytose bacteria (Figure 1). Throughout history, it was believed that lethal factor caused macrophages to make TNF-alpha and interleukin 1- beta (IL1-beta). TNF-alpha is a cytokine whose primary role is to regulate immune cells as well as to induce inflammation and apoptosis or programmed cell death. IL1- beta is another cytokine that also regulates inflammation and apoptosis. The over-production of TNF-alpha and IL1-beta ultimately leads to septic shock and death. However, recent evidence indicates that anthrax also targets endothelial cells (cells that line serous cavities such as the pericardial cavity, pleural cavity, and the peritoneal cavity, 5 Chapter 1: General Introduction lymph vessels, and blood vessels), causing vascular leakage of fluid and cells, and ultimately hypovolemic shock (low blood volume), and septic shock (Pimental et al., 2004; Suffin et al., 1978). It is well known that both lethal (PA + LF) and edema (PA + EF) toxins are able to suppress key parts of the innate immune response to the developing infection (Duesbery et al., 1998; Erwin et al., 2001; Kalns et al., 2002; Moayeri et al., 2003; O'Brien et al., 1985; Pellizzari et al., 1999; Popov et al., 2002; Wright and Mandell, 1986). Fig 1: Mechanism of action of Anthrax Toxin (www.biocarta.com/pathfiles/h_anthraxPathway.asp) 1.3 ENVIRONMENTAL SURVIVALITY, CLINICAL PATHOGENECITY AND DIAGNOSIS OF BACILLUS ANTHRACIS: Soil is the main reservoir of B. anthracis spores. In India, various types of soils are found. The most common types of soil are: Red soil (widely spread in Andhra Pradesh, Kerala and Karnataka, the Red color is due to diffusion of iron in the profile), Black soil (distributed in Madhya Pradesh and Tamil Nadu and contains a high proportion of Calcium and Magnesium carbonate), Alluvial Soil (covers most parts of the West Bengal, Uttar Pradesh and Tamil Nadu and also classified as calcareous soils, saline and alkaline soil and coastal soils). Alkaline soil containing adequate nitrogen, calcium and organic matter is required in conjugation with extreme weather changes, such as drought followed by heavy rain, when these conditions are met, the organisms are thought to undergo a vegetative cycle in soil and then multiply. This process could generate high concentration of anthrax spores in soil causing disease in grazing animals and the occasional outbreaks separated by 6 Chapter 1: General Introduction long disease-free intervals (Kanffman, 1990). Recurrent anthrax outbreaks have been associated with calcareous, neutral or slightly alkaline soils rich in organic matter which encourage survival of spores (Moazein et al., 2004; Van Ness, 1971). Along with natural reservoir, talcum powder and other environmental samples for instance, clay, sand, wheat flour and chalk powder can also be used for spiking of anthrax spores. There are several publications on the sample preparation for molecular detection of microorganism in soil samples. However, it is obvious from most publications on the subject that purification of nucleic acids from soil is not as easy as with samples of other environmental origin (Bayer et al., 1995; Picard et al., 1992; Pillai et al., 1991; Smalla et al., 1993; Tebbe and Vahjen, 1993; Volossoiuk et al., 1995). Numerous substances present in the most types of soil e.g. humic and phenolic compounds and metal ions, seriously affect the specificity and activity of the Taq polymerase. To overcome the problems with these inhibitors, several protocols for the detection of B. anthracis spores were optimized in the present study. As these inhibitors are potent interfering agents in PCR, various sample processing steps are included before the detection of spores (Volossoiuk et al., 1995). Various methods have been developed for the detection of B. anthracis and many more are still in the development phase. Most of the assays are based on detecting the i) whole organism, ii) bacterial antigens, and/or iii) the nucleic acid. Anthrax is still enzootic in several parts of India. The clinical diagnosis of cutaneous anthrax is traditionally established by conventional microbiological methods, such as culture and Gram staining. However, these methods often yield negative results when patients have received antibiotics. Hence, blood culture is recommended only if the patient has evidence of systemic anthrax and has not received antibiotic therapy (Shieh et al., 2003). Molecular tests, including PCR and real-time PCR also do not work well for detection of cutaneous anthrax cases after antibiotic therapy and when wounds are super infected by several other pathogens, most often with staphylococcus or streptococcus (Edwards, 1992). Hence, the main objectives of this study include the development of indirect ELISA for detection of anti-PA and anti-LF serological response in human for early diagnosis of anthrax as well as on development of surface plasmon resonance (SPR) biosensor and sandwich ELISA for detection of anthrax spores in environmental and spiked matrices. 7 Chapter 1: General Introduction 1.4 THE STUDY WAS CARRIED OUT WITH THE FOLLOWING OBJECTIVES: 1. Cloning and expression of different toxin genes of Bacillus anthracis in suitable host for production of antibodies and their subsequent use in development of diagnostic assays. 2. Development of various immunological detection systems for sero-diagnosis of anthrax. 3. Development of various detection systems for detection and differentiation of Bacillus anthracis spores in environmental samples. 8