* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download pdf
Survey
Document related concepts
Transcript
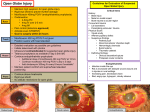
Spectrum of Globe Abnormalities on MRI and CT
Poster No.:
C-2594
Congress:
ECR 2013
Type:
Educational Exhibit
Authors:
J. T. P. D. Hallinan, P. G. Pillay, H. L. L. Koh, K. Y. Goh, W. Y. Yu;
Singapore/SG
Keywords:
Eyes, CT, MR, Diagnostic procedure, Education, Pathology,
Education and training, Trauma
DOI:
10.1594/ecr2013/C-2594
Any information contained in this pdf file is automatically generated from digital material
submitted to EPOS by third parties in the form of scientific presentations. References
to any names, marks, products, or services of third parties or hypertext links to thirdparty sites or information are provided solely as a convenience to you and do not in
any way constitute or imply ECR's endorsement, sponsorship or recommendation of the
third party, information, product or service. ECR is not responsible for the content of
these pages and does not make any representations regarding the content or accuracy
of material in this file.
As per copyright regulations, any unauthorised use of the material or parts thereof as
well as commercial reproduction or multiple distribution by any traditional or electronically
based reproduction/publication method ist strictly prohibited.
You agree to defend, indemnify, and hold ECR harmless from and against any and all
claims, damages, costs, and expenses, including attorneys' fees, arising from or related
to your use of these pages.
Please note: Links to movies, ppt slideshows and any other multimedia files are not
available in the pdf version of presentations.
www.myESR.org
Page 1 of 28
Learning objectives
Globe abnormalities can be readily detected on both dedicated and non-dedicated
CT and MRI studies. Accurate interpretation of the imaging requires an in depth
understanding of the anatomy of the globe. In fact, this poster will provide a novel
approach to the subject by classifying diagnoses based on the anatomical location. We
hope this will reinforce an understanding of the topic from first principals rather than
pattern recognition. We therefore propose the following learning objectives:
•
•
•
Outline the cross-sectional anatomy of the globe.
Illustrate the spectrum of globe abnormalities detected on CT and MR using
fundamental anatomical knowledge.
Illustrate additional CT or MRI characteristics of globe abnormalities to
narrow the differential diagnosis. A wide range of cases will be provided with
fundoscopic correlation as appropriate.
Background
Background:
The majority of globe imaging is performed secondary to CT and MRI imaging of the
brain for a multitude of indications ranging from trauma to neoplasia. Incidental detection
of an abnormality is commonplace, especially given recent advances in MR and CT
technology, which allows for the globe to be visualised in ever finer detail. In order to
interpret the globe abnormality a primary understanding of the globe anatomy is key.
Knowledge of the imaging features of both traumatic and non-traumatic globe
abnormalities is necessary to provide appropriate ophthalmology referral and accurate
diagnosis, thereby preventing devastating consequences such as vision loss. In addition
knowledge of incidental degenerative changes, globe implants and fillers is important to
prevent unnecessary work-up.
Globe anatomy overview (Figs 1 and 2)
•
•
•
Globe occupies one third of the volume of the orbit (~6.5 mls).
The vitreous humour represents two-thirds of the volume.
The wall of the globe comprises three layers;
•
•
•
Fibrous coat (outer) enveloped by Tenon's capsule.
Uvea (middle)
Retina (inner layer)
Page 2 of 28
1. Fibrous coat (outer layer)
Constitutes the sclera and transparent cornea anteriorly.
1.1 Tenon's capsule
•
•
•
The sclera is enveloped by the fibroelastic Tenon's capsule, which fuses
with the bulbar conjunctiva.
A potential space, termed the episcleral space can extend between the
fascia and the sclera.
Effusions due to infection or inflammation of adjacent structures and
haemorrhage due to trauma or neoplasms can distend the episcleral space
(Figs 3, 4 & 5).
1.2 Cornea
•
•
•
Protects the anterior chamber and is a key component of the refractive
system.
90% of the thickness provided by the stroma.
On MRI the cornea is a predominantly low intensity structure. On T1W
images (T1WI) can be highlighted by an overlying, thin, slightly hyperintense
tear film.
1.3 Sclera
•
•
•
•
•
•
•
•
•
Merges with cornea at the limbus, composed of collagen and is hypointense
on MRI.
Maintains intraocular pressure and protects the globe.
Disruption of the sclera can result from trauma (globe rupture; Figs 6 & 7) or
secondary to degeneration, infection or inflammation.
Sclera alters in thickness and shape throughout life.
Sustained intraocular pressure in childhood can lead to diffused increased
size of the globe termed buphthalmos.
In adults the more rigid scleral structure results in more focal thinning and
protrusions termed staphylomas (Fig 8).
Other globe shape abnormalities include colobomas (congenital defects
in the layers of the globe including the optic disc) and phthisis bulbi
representing an end-stage atrophic globe (Figs 9 & 10).
Other scleral lesions include calcifications, which form at the insertions of
the recti in elderly patients (Fig 11) and iatrogenic causes such as scleral
buckles for treatment of retinal detachment (Fig 12).
Episcleritis is typically a self-limiting idiopathic disorder, where as scleritis is
a more serious condition associated with connective tissue diseases such as
Page 3 of 28
rheumatoid arthritis. Scleritis may be complicated by exudative chorioretinal
detachment and glaucoma (Fig 5).
2. Uveal tract (middle layer) and retina (inner layer)
2.1 Uveal tract
•
•
•
•
•
Consists of the iris, ciliary body and choroid. Highly vascular and contains
pigmented melanocytes.
Iris is a pigmented circular structure controlling the size of the pupil and
attaches to the ciliary body.
The ciliary body consists of the anterior pars plicata (produces aqueous
humour) and posterior pars plana. Ciliary musculature attaches to the lens
via the zonules of Zinn and are important for accommodation.
The choroid merges with the ciliary body at the ora serrata and extends
posteriorly to the optic nerve head. Provides retinal nourishment and
absorbs reflected light.
Choroid attaches firmly to the sclera at the optic disk and where the vortex
veins exit the globe.
2.2 Retina
•
•
•
•
Innermost sensory layer consists of:
•
Outer retinal pigment epithelium (RPE)
•
Inner sensory retina containing photoreceptors.
Layers tightly bound at the optic disc and ora serrata where the RPE
becomes continuous with the ciliary body.
Otherwise only weak apposition of the two retinal layers.
2.3 MRI appearance of the uveal tract and retina
•
•
T1WI: Hyperintense (likely related to melanocytes)
T2WI: Hypointense
•
Provides good contrast between the hypointense outer sclera and
hyperintense inner vitreous.
2.4 Retinal and Ciliochoroidal detachment
Potential spaces for fluid accumulation resulting in detachment:
•
•
•
Between the retinal layers (subretinal space).
Ciliary body/choroid and sclera (suprachoroidal space)
Hyaloid base and retina (posterior hyaloid space).
Page 4 of 28
Ciliochoroidal detachments (Figs 13, 14 & 15) occur due to haemorrhage (trauma, prior
intervention, underlying neoplasm) or serous effusions (ocular hypotony or inflammation).
Retinal detachments (Figs 3 and 15) commonly associated with a hole (regma) classified
as rhegmatogenous versus nonrhegmatogenous.
Fundoscopy readily allows for detection of retinal detachments with MRI useful for
detection of an underlying cause, e.g. neoplasm.
•
MRI distinction of ciliochoroidal from retinal detachment not always possible
although several patterns exist.
•
Anteriorly, ciliochoroidal detachments commonly extend into the ciliary body
where as retinal detachments are limited by the ora serrata.
Posteriorly, ciliochoroidal detachments are limited by the insertions of the
vortex veins where as retinal detachments are limited by the optic disc
producing a characteristic V shape.
•
Retinal detachments can be treated using scleral buckling, pneumatic retinopexy, pars
plana vitrectomy or injection of intraocular silicone oil (Figs 16 and 17).
2.5 Ocular neoplasms
Malignant melanoma represents the most common intraocular malignancy in adults and
occurs in the pigmented uveal tract. Other neoplasms involving the highly vascular uveal
tract include metastases and benign neoplasms such as haemangiomas.
2.51 Malignant melanoma (Fig 18)
•
•
•
•
•
•
•
•
Commonly unilateral, less common than the cutaneous form, and may
present with pain or decreased vision.
On MRI typically seen as a focal mass at the periphery of the globe with
propensity for chorioretinal detachment
Appearance is non-uniform on imaging due to varying melanin:
•
Melanocytic: CT; Slightly hyperdense, MRI; #T1WI, iso/# on T2WI.
Enhancement on both.
In exudative/haemorrhagic retinal detachment difficult to distuinguish a
melanocytic melanoma.
Contrast enhancement is a key discriminator.
•
Amelanotic: Similar to other ocular neoplasms.
MRI is the technique of choice for asessing episcleral extension (occurs in ~
13% and is an important prognostic feature).
Page 5 of 28
2.52 Ocular metastases (Fig 19)
•
•
•
•
Highly vascular uveal tract most common site.
Breast and lung primaries most common.
Can lead to chorioretinal detachment with accompanying haemorrhage or
exudates.
T1WI useful to distinguish from melanocytic melanoma with the exception of
hyperintense haemorrhagic or mucinous adenocarcinomas.
2.53 Retinoblastoma
•
•
•
•
•
•
Most common intraocular childhood malignancy (Rb gene mutation; 13q14).
Typically in children < 5 years of age who present with leucocoria. Other
causes of leucocoria include Coat's disease and persistent hyperplastic
primary vitreous (PHPV).
CT is useful in establishing bilateral disease due to calcifications in 90%.
Other differential diagnoses for this finding includes cytomegalovirus
choreoretinitis and coloboma.
MRI useful for optic nerve and intracranial extension:
Retinoblastoma typically appears as hyperintense on T1WI images to
normal vitreous and hypointense on T2WI with mild to intense post-contrast
enhancement.
Fat-suppressed, post contrast T1WI is the best imaging method for optic
nerve and episcleral extension.
2.54 Vascular neoplasms and phakomatoses/neurocutaneous syndromes (Figs 20
and 21)
•
•
•
Vascular neoplasms of the choroid uncommon benign lesions.
Cavernous malformations associated with Sturge-Weber syndrome; can be
complicated by retinal tears and detachment.
Capillary haemangiomas of the retina occur in a quarter to half of patients
with Von Hippel-Lindau syndrome:
•
Usually supplied by large feeder vessels with propensity for leakage
and subsequent exudative/haemorrhagic retinal detachment.
•
Often small but sometimes visualised on MRI as hyperintense
on T1WI, and hyperintense on T2WI allowing distinction from
melanocytic melanomas.
2.6 Uveitis (Fig 22)
Inflammation of the uveal tract commonly involves the adjacent retina and sclera.
•
Often idiopathic with numerous infective and inflammatory causes described
in the literature including sarcoidosis, rheumatoid arthritis, and toxoplasma.
Page 6 of 28
•
CT or MR evaluation may be useful in posterior uveitis for assessment of
chorioretinal detachment, abscesses or foreign bodies providing a nidus for
infection.
3. Vitreous body
•
•
•
•
Gel-like fluid consisting of 99% water.
Bounded by the posterior and anterior hyaloid membranes and provides
support to the posterior lens and pressure to ensure apposition of the retinal
layers.
In old age the vitreous may shrink and thicken forming clumps of material
('floaters'). This process may result in traction causing separation of the
posterior hyaloid membrane from the sensory retina (posterior vitreous
detachment).
Accelerated vitreous degeneration may result from trauma, surgery,
inflammation or significant myopia.
3.1 Posterior vitreous detachment
On MR and CT posterior vitreous detachment can be seen as a membrane within the
vitreous cavity detached from the optic disc and attached at the ora serrata.
3.2 Endophthalmitis
•
•
•
•
•
Inflammation/infection predominantly involving the anterior chamber and
vitreous humour.
Despite aggressive therapy the outcome remains poor.
Causative organisms may enter the globe haematogenously or exogenously
secondary to penetrating trauma or surgery.
•
Most common organisms include skin commensals such as
staphylococcus epidermis, candida and parasites including
cysticercosis and toxocariasis.
CT and MRI may demonstrate uveal thickening and enhancement,
chrorioretinal or vitreous detachment and increased density or T1W intensity
of the vitreous due to proteinaceous exudates.
4. Lens (Fig 23)
•
•
•
•
Forms the posterior boundary of the anterior chamber.
Transparent ovoid crystalline structure hypointense on T2WI.
Prostheses are readily identifiable on CT and MRI.
Dislocation also identified secondary to trauma or degeneration of the
zonular fibers.
Page 7 of 28
Images for this section:
Fig. 1: Globe anatomy illustration
Fig. 2: Normal globe MRI anatomy. The lens shows hypointense signal on all sequences,
(a) On axial T2W images, the vitreous and aqueous humour are diffusely hyperintense;
Page 8 of 28
(b) Axial T1W image of the right globe. The retina, choroid and ciliary bodies are
hyperintense and show enhancement on the fat suppressed axial T1W post gadolinium
images (c).
Fig. 3: Axial T2W images (a) following direct left globe trauma. There is iso to hypointense
episcleral material consistent with a haematoma. Choroidal and retinal detachment is
seen in the left globe with underlying suprachoroidal and subretinal fluid respectively.
Figure (b) shows a corresponding photograph with extensive periorbital swelling and
subconjunctival haemorrhage.
Fig. 4: An axial non-contrast image from a CT brain for assessment of traumatic head
and facial injuries (a). An episcleral hyperdense haematoma is seen in conjunction with a
periorbital haematoma. The globe appears intact. Extension of the haematoma posterior
to the globe, likely in the intra-conal space is seen. The corresponding photograph (b)
shows marked periorbital swelling and bruising with subconjunctival haemorrhage. This
patient also had an orbital floor fracture (not shown)with limited left upgaze.
Page 9 of 28
Fig. 5: An axial non-contrast enhanced image from a CT orbits (a). This patient had a
history of Wegener's granulomatosis with posterior scleritis. There are bilateral episcleral
fluid collections with distortion of the globes likely due to scleral degeneration or necrosis.
Corresponding fundoscopy (b) and a photograph (c) show engorged scleral vessels.
Additional fundoscopic images (d) and (e) show bilateral choroid detachments with a
characteristic orange-brown, solid appearing elevation with a smooth, convex surface.
This is not well visualised on the CT images.
Page 10 of 28
Fig. 6: Axial (a,b) non-contrast images from a CT brain for assessment of traumatic head
injury. There is right globe rupture with loss of the normal scleral contour, hyperdense
material consistent with haemorrhage in the vitreous, and surrounding periorbital and
episcleral haematomas. There is traumatic lens dislocation seen protruding through a
scleral defect in the lateral globe (b). Another coronal non-contrast CT image in a different
patient shows left globe rupture with a superolateral lens dislocation and protrusion
through a scleral defect (c).
Page 11 of 28
Fig. 7: Axial (a) and coronal (b) non-contrast images from a CT brain for assessment of
direct globe injury. There is left globe rupture with complete loss of the normal scleral
contour, vitreous haemorrhage and surrounding periorbital and episcleral haematomas.
The lens is dislocated and seen outside the globe in the left inferolateral orbit.
Page 12 of 28
Fig. 8: An axial non-contrast image (a) from a CT orbits for assessment of homonymous
hemianopia. There are bilateral focal protrusions through the thinned sclera posteriorly
consistent with staphylomas. Corresponding fundoscopic images from the right (b) and
left (c) eyes show bilateral myopic degeneration, peri-papillary atrophy, and bilateral
staphylomas.
Fig. 9: An axial non-contrast image from a CT brain for assessment of altered mental
state. There is right phthisis bulbi with an irregular, scarred, shrunken right globe and
dense internal calcification.
Page 13 of 28
Fig. 10: An axial non-contrast image from a CT brain for assessment of traumatic head
injury. There is left phthisis bulbi with an irregular, scarred, shrunken globe and left optic
disc calcification. Incidental right scleral calcifications are seen at the insertions of the
medial and lateral recti.
Page 14 of 28
Fig. 11: Axial non-contrast images from a CT brain for assessment of altered mental
state. There are bilateral lens prostheses with incidental scleral calcifications at the
insertion of the medial rectus on the right and both the medial and lateral recti on the left.
These calcifications represent a normal part of aging.
Fig. 12: Axial (a) and coronal (b) non-contrast images from a CT brain for assessment
of frequent falls. There are bilateral bands of hyperdensity, which do not conform to the
insertions of the extra-ocular muscles. These are consistent with prior bilateral, scleral
buckles for treatment of retinal detachment, although the characteristic concavity at the
site of banding is not seen in this case.
Page 15 of 28
Fig. 13: Axial T1W (a) T1W post gadolinium (b) and coronal (T2W) images for suspected
chorioretinal detachment and evaluation for an underlying lesion. There is ciliochoroidal
detachment (a) and underlying suprachoroidal fluid (c) seen extending anterior to the
expected location of the ora serrata (a). Enhancement of the choroid is noted, which
is expected in detachment due to an inflammatory response. No enhancing lesion is
detected to suggest a neoplastic cause.
Page 16 of 28
Fig. 14: Coronal T1W post gadolinium (a) and axial T1W post gadolinium images (b)
from an MRI orbits for right sided visual loss. There is right choroidal detachment seen
limited posteriorly at the expected location of the vortex vein insertion. Enhancement of
the detached choroid is also apparent as seen in the prior case.
Page 17 of 28
Fig. 15: Axial T2W (a) gradient echo (b) T1W (c) and sagittal T2W images (d,e) from
an MRI orbits were performed following trauma to assess for globe rupture. There is
retinal and choroidal detachment noted, the latter involving the ciliary body medially
(a). An underlying subretinal/suprachoroidal collection is noted with T1W shortening
and foci of susceptibility. These findings are consistent with traumatic haemorrhagic
chorioretinal detachment. There are additional episcleral and periorbital haematomata
which are hyperintense on T1W images. (d) On the sagittal view the retinal detachment
is well demonstrated limited anteriorly by the ora serrata. Buckling of the superior sclera
and loss of globe volume is consistent with globe rupture. The hypointense material in
the vitreous is also likely consistent with haemorrhage. (e) Coronal T2W images also
show the scleral defect.
Fig. 16: Axial non-contrast images from a CT brain for assessment of altered mental
state. Hyperdense material is seen filling the vitreous cavity on the right with no evidence
of overlying trauma or a periorbital haematoma. This patient had undergone silicone oil
injection for treatment of retinal detachment.
Page 18 of 28
Fig. 17: Axial non-contrast images from a CT brain for assessment of altered
mental state. Gas is noted in the anterior vitreous compartment consistent with
pneumatic retinopexy typically used in the treatment of superior rhegmatogenous retinal
detachments.
Page 19 of 28
Page 20 of 28
Fig. 18: Dedicated MRI orbits for gradual left visual loss. (a) Axial T2WI: There is
a lobulated hypointense lesion arising in the anteromedial left globe with endophytic
extension into the vitreous. (b) T1WI: The lesion is hyperintense and (c) T1WI post
gadolinium shows enhancement. A corresponding photograph (d) shows a pigmented
lesion arising from the inferomedial globe wall with surrounding haemorrhage. This lesion
was consistent with an uveal melanoma on histology.
Fig. 19: A gentleman with a known primary lung adenocarcinoma presenting with left
sided blindness. Axial T2W(a) and axial T1W(b) post gadolinium images from an MRI
orbits. There are hypointense intraocular lesions arising adjacent to the sclera in the left
medial globe and close to the left optic nerve head. The medial lesion shows contrast
enhancement. These lesions are consistent with choroidal metastases with no choroidal
detachment detected.
Page 21 of 28
Fig. 20: Coronal T2W (a) and T1W post gadolinium (b) images from an MRI orbits
performed for a suspected intra-ocular tumour. There is a small hypointense, enhancing
lesion in the inferior globe forming a broad base against the sclera. This is likely to
arise from the choroid given the enhancement and is most likely consistent with a
haemangioma or haemangioblastoma. A metastasis is unlikely as there was no history
of a primary malignancy. An amelanocytic melanoma is another consideration.
Page 22 of 28
Fig. 21: Axial T1W post gadolinium MRI images of the posterior fossa (a) and the orbits
(b). This patient had presented with headaches. A markedly enhancing lesion is seen
arising in the region of the fourth ventricle complicated by hydrocephalus (not shown).
An additional avidly enhancing lesion is seen arising from the choroidal layer of the left
lateral globe with suggestion of an associated chorioretinal detachment. These findings
are suggestive of cerebellar and retinal/choroidal haemangioblastomas, although an
associated cystic component for the cerebellar lesion is more typical. Underlying Von
Hippel-Lindau disease should be considered. Resection of the cerebellar lesion was
performed with confirmation of a haemangioblastoma on histology.
Page 23 of 28
Fig. 22: Axial T1WI (a) T1WI post gadolinium (b) from an MRI orbits performed for
orbital pain and acute visual loss. On the T1WI there is isointense thickening and
enhancement of the retina, posterior choroid and optic disc. These features are likely
consistent with posterior uveitis, which may be associated with inflammatory conditions
such as sarcoidosis or infections such as toxoplasma or cytomegalovirus. The patient
did not attend for follow-up.
Page 24 of 28
Fig. 23: An axial T2W image from an MRI orbits for evaluation of left visual loss. Left
sided lens dislocation (lens luxation) is seen with the hypointense lens lying dependently
adjacent to the retina in the posterior vitreous humour. No history of trauma or prior ocular
inflammation was noted. A right-sided lens prosthesis is noted.
Page 25 of 28
Imaging findings OR Procedure details
CT
CT scans were obtained on a 32 or 320-row scanner. Non-contrast scans are typically
performed for initial assessment of trauma or suspected cerebrovascular accident, with
incidental imaging of the orbits.
CT is useful in the initial evaluation of orbital and globe trauma for the assessment
of fractures, extra-ocular muscle herniation and suspected globe rupture. CT is the
technique of choice for evaluating for metallic or paramagnetic foreign bodies, where
MRI is contraindicated due to potential migration and local heating. CT is also useful for
evaluation of globe calcifications, especially in the case of retinoblastoma as described
in the prior section.
MRI
MRI scans of the brain or dedicated studies of the orbits were performed on a 1.5 or
3 Tesla platform. For the dedicated protocol the following sequences are commonly
performed; axial and coronal T1WI with and without fat suppression, axial and coronal
STIR or fat suppressed T2WI, and multiplanar fat suppressed T1W images post
gadolinium.
High resolution MRI allows depiction of the sclera from the choroid and retina. Table
1 shows the common MRI characteristics of the various structures in the globe. MRI
provides exquisite soft tissue contrast for the evaluation of chorioretinal detachments
and potential underlying neoplasms. The technique is limited by lengthy scanning time,
increased cost compared to CT and requirements for sedation in children and other noncompliant patient groups.
Table 1: T1W and T2W characteristics of the globe structures.
MRI sequences
Layer
T1W
T2W
Tenon's capsule
Not usually visible. Can be distended by fluid/
haemorrhage accumulating in the potential episcleral
space.
Page 26 of 28
Cornea
Hypointense- but can be Hypointense
highlighted by an overlying
hyperintense tear film on
T1WI
Sclera
Hypointense
Hypointense
Uveal tract, choroid
Hyperintense
Hypointense
Retina
Hyperintense- Not usually Hypointense
seen separately from the
underlying choroid
Aqueous/vitreous
humour
Hypointense
Hyperintense
Lens
Hypointense
Hypointense
Conclusion
A multitude of globe abnormalities can be detected and characterised on CT and MRI
studies. Understanding the anatomy is a key component in the structured approach
to producing a differential diagnosis. An understanding of the CT attenuation and MRI
signal characteristics can also help characterise lesions, especially in the case of uveal
melanoma.
The radiologist fulfils an important role in the primary diagnosis of clinically significant
and potentially treatable globe abnormalities contributing to rapid referral and improved
outcomes.
References
References
1.
2.
3.
Van Tassel P, Mafee MF, Atlas Sw, Galetta S. Chapter 23: Eye, orbit and
visual system. In: Atlas S, editor. Magnetic Resonance Imaging Of The Brain
And Spine, Volume 2. 4th ed. Philadelphia: Lippincott, Williams & Wilkins;
2009. p. 1268-1282.
Mafee MF, Karimi A, Shah J, Rapoport M, Ansari SA. Anatomy and
pathology of the eye: role of MR imaging and CT. Neuroimaging Clin N Am.
2005 Feb;15(1):23-47.
Roy AA, Davagnanam I, Evanson J. Abnormalities of the globe. Clin Radiol.
2012 Oct;67(10):1011-22.
Page 27 of 28
4.
5.
Smoker WR, Gentry LR, Yee NK, Reede DL, Nerad JA. Vascular
lesions of the orbit: more than meets the eye. Radiographics. 2008 JanFeb;28(1):185-204.
LeBedis CA, Sakai O. Nontraumatic orbital conditions: diagnosis with
CT and MR imaging in the emergent setting. Radiographics. 2008
Oct;28(6):1741-53.
Personal Information
Page 28 of 28