* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Remel Clostridium difficile Toxin A/B Fact Sheet
Survey
Document related concepts
Chagas disease wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Onchocerciasis wikipedia , lookup
Meningococcal disease wikipedia , lookup
Schistosomiasis wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Leptospirosis wikipedia , lookup
Gastroenteritis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Oesophagostomum wikipedia , lookup
Botulinum toxin wikipedia , lookup
Transcript
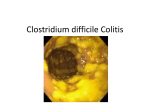
Clostridium difficile Toxin A/B Fact Sheet Clostridium difficile is an anaerobic, spore-forming, gram-positive rod that produces toxins A and B. Changing Epidemiology: Community-Acquired Clostridium difficile-Associated Disease (CDAD) •More than 90% of healthcare associated C. difficile infections occur after or during antimicrobial therapy. However, C. difficile strains are changing, moving into the community and affecting non-traditional populations, even children. • Cases have been reported in otherwise healthy patients with minimal or no exposure to a healthcare setting: peripartum women, small children, and people taking heartburn medications. • Changing implications include close-contact transmission, high recurrence rate, young patient age, bloody diarrhea, and lack of antimicrobial exposure. • Clinicians should consider the diagnosis of CDAD in patients with severe diarrhea even if the patients do not necessarily have traditional risk factors such as recent hospitalization or antimicrobial use. Variant Strains Exist: Toxin A Negative, Toxin B Positive • Most pathogenic strains of C. difficile produce both toxin A and B. • Strains that are A-B+ are fully pathogenic and capable of producing the full spectrum of disease. • Prevalence of Toxin A-B+ strains varies widely. • Toxin A-B+ strains are not detected by toxin A specific tests. Emerging Epidemic Strain: Toxinotype III or BI, NAP1, 027 • The epidemic C. difficile strain causes more severe disease and increased mortality. The strain has been responsible for thousands of deaths in North America alone. • Early diagnosis and treatment is critical to reducing severe outcomes. • The epidemic strain produces a third toxin, binary toxin; its role in human disease is not yet defined, but it is suggested that it may contribute to the pathogenesis of CDAD. • Mutation of a regulator gene tcdC may lead to increased toxin production: 16x more toxin A and 23x more toxin B than other strains. • This strain has increased antimicrobial resistance, notably to clindamycin and fluoroquinolones [gatifloxin and moxifloxacin]. • Research to date shows that the epidemic strain produces toxins A and B and common antigen (glutamate dehydrogenase) and reacts in commercial C. difficile tests specific for the toxins or for antigen. Prevalence is Increasing • Incidence rates and the severity of CDAD have increased significantly in U.S., Canadian, and European hospitals during the past few years. National rates have more than doubled. •Elderly and immunocompromised patients are at increased risk for developing complications. • Early diagnosis results in improved patient care and reduces the likelihood of nosocomial outbreaks. • CDAD is the 4th most common nosocomial disease reported to the CDC with 3 million cases annually in the U.S. Transmission / Financial Burden • Spores of C. difficile may persist on surfaces for years and remain a problematic source of environmental contamination and infection. The epidemic strain hyper produces spores exacerbating the situation. • Alcohol is not sporicidal and is not efficient in removing C. difficile from the hands. Healthcare workers should wash their hands with soap and water instead of using alcohol-based waterless hand sanitizers during outbreaks. •CDAD can increase length of stay by 1 to 2 weeks AND can cost an additional $3,669 to $7,234 per patient hospitalization. • Restraint in the use of epidemiologically implicated antimicrobial agents is required to control the epidemics. Treatment / Patient Management • CDAD is toxin mediated but treatment is not based on the toxin present. • First step in CDAD management is to discontinue antibiotics combined with implementation of supportive therapy with rehydration and electrolyte replacement. • CDAD usually resolves within 10-12 days. • Can treat with metronidazole or oral vancomycin. Typically, oral metronidazole for mild disease; vancomycin for severe disease. • In rare cases, surgery may be required. •Relapse or reinfections occurs in 12-24% of patients. To learn more about Healthcare-Associated Infection solutions from Remel, visit www.remel.com/hai or contact your Remel Technical Sales Representative. Sources: l l l l l CDC. Severe Clostridium difficile-Associated Disease in Populations Previously at Low Risk — Four States. 2005. MMWR. 2005:54(47); 1201-1205. Kyne, L., et. al. 2002. Health Care Costs and Mortality Associated with Nosocomial Diarrhea Due to Clostridium difficile. Clinical Infectious Diseases. 2002;34:346-353. McDonald, L., 2005. Clostridium difficile: Responding to a New Threat From an Old Enemy. Infection Control and Hospital Epidemiology. 2005;26:672-675. Owens, R., 2006. Clostridium difficile-Associated Disease: An Emerging Threat to Patient Safety. Pharmacotherapy. 2006;26(3):299-311. Sunenshine, R.H., et. al., 2006. Clostridium difficile-associated disease: New Challenges from an Established Pathogen. Cleveland Clinic Journal of Medicine. Vol. 73. No. 2:187-197. 12076 Santa Fe Drive 800-255-6730 Lenexa, KS 66215 remel.com 991- 366