* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Myocardial perfusion scintigraphy using rubidium
Survey
Document related concepts
Transcript
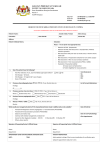
Published Online August 21, 2013 Myocardial perfusion scintigraphy using rubidium-82 positron emission tomography Parthiban Arumugam*, Deborah Tout, and Christine Tonge Nuclear Medicine Centre, Central Manchester NHS Foundation Trust, Manchester, UK Introduction: Myocardial perfusion scintigraphy (MPS) is an established noninvasive technique for the diagnosis and management of patients with suspected or known coronary artery disease. Because of the wealth of prognostic data, MPS single photon emission computed tomography (SPECT) is the most commonly used functional test to detect inducible ischaemia. However, the increasing availability of positron emission tomography (PET) scanners for oncology along with the introduction of the generator-produced PET tracer rubidium-82 (82Rb) has helped the growth of MPS PET. Sources of data: Relevant review articles, primary literature and clinical guidelines identified through medical literature search engines. Areas of agreement: PET offers advantages over SPECT, including increased patient throughput because of rapid scanning protocols, reduced radiation exposure to patients and the ability to quantify tracer distribution accurately and hence measure myocardial perfusion in millilitre per gram per minute and hence myocardial perfusion reserve (MPR). Areas of controversy: Although PET has advantages over SPECT, there are no largescale prognostic or cost-effectiveness data to support it use as the primary MPS technique. Growing points: A wider use of absolute measurements of perfusion has the potential to improve diagnostic accuracy and to add prognostic value over relative assessment of myocardial perfusion. Areas timely for developing research: Assessment of absolute myocardial perfusion may provide insight into the effects of traditional risk factors on perfusion reserve and the impact of risk factor modifications on progression of coronary artery disease. *Correspondence address. Nuclear Medicine Centre, Manchester Royal Infirmary, Oxford Road, Manchester M13 9WL, UK. E-mail: parthiban. [email protected] Keywords: PET perfusion/myocardial blood flow/myocardial perfusion scintigraphy Accepted: July 24, 2013 British Medical Bulletin 2013; 107: 87–100 DOI:10.1093/bmb/ldt026 & The Author 2013. Published by Oxford University Press. All rights reserved. For permissions, please e-mail: [email protected] P. Arumugam et al. Introduction As the evidence accumulates for the benefits of managing coronary artery disease (CAD) based upon its functional significance, there has been a shift from an approach based upon the coronary anatomy.1,2 Although fractional flow reserve (FFR) provides an invasive assessment of coronary function, non-invasive imaging in the form of MPS, stress echocardiography and cardiac magnetic resonance (CMR) can provide similar information. Myocardial perfusion scintigraphy (MPS) single photon emission computed tomography (SPECT) is the most commonly used technique and there is extensive and robust data on its diagnostic accuracy, prognostic power and its cost-effectiveness.3 However, the limitations of SPECT include image artefacts, especially due to soft tissue attenuation, and the lack of quantification. The images are displayed using a colour scale that shows the myocardium with highest (but not necessarily normal) uptake at the top of the scale and the rest of the myocardium scaled down accordingly. The display is therefore relative to the region with highest tracer uptake and it is possible to underestimate the severity of ischaemia if all areas have abnormal perfusion reserve.4 Although there have been significant developments in SPECT technology including attenuation correction, resolution recovery and dynamic solid state cameras, positron emission tomography (PET) can provide all of this and more. Almost all oncology PET cameras are combined with high-resolution X-ray computed tomography (CT) and, for the heart, these can provide multimodality images combining anatomical and functional information. This review will however focus on the functional component using 82Rb. Imaging principles of MPS PET Tracer characteristics Cardiac PET requires the intravenous administration of a radionuclide tracer, which is taken up by the myocardium. The PET tracers in clinical use are either produced in a cyclotron or locally in a generator. A cyclotron is a particle accelerator capable of rapidly accelerating charged particles, which can be made to bombard a target to produce positron-emitting isotopes. An on-site cyclotron is not available in the majority of PET centres because of its cost and complexity and this limits the use of the very short half-life positron-emitting isotopes. Generator-produced isotopes are simpler and more convenient as the generator can provide continuous on-site production for its lifetime, which will depend on the half-life of the parent isotope. The characteristics of the most commonly used cardiac 88 British Medical Bulletin 2013;107 MPS using rubidium-82 PET PET tracers are shown in Table 1. Tracer delivery is proportional to blood flow, but myocardial uptake depends also on its extraction from the blood. The most physiological tracer is oxygen-15 (15O) water, which is freely diffusible and has a first pass extraction of 100% with rapid equilibrium between the vascular and tissue compartments. Accurate measurements of myocardial perfusion can be made but high-quality images of myocardial perfusion are not possible. Instead mathematical models must be used to produce parametric images of perfusion but these are often noisy and of poor quality.5 Nitrogen-13 (13N) ammonia enters the myocyte by passive diffusion or active transport with a first pass extraction of 80%, and it is rapidly metabolized to glutamine and retained in the myocyte. Because of its short half-life its use is restricted to centres with a cyclotron. It provides images of relative perfusion and cardiac function similar to SPECT and measurements of myocardial perfusion are well validated.5 82 Rb is produced from an 82Sr–82Rb generator, which has a clinical life of 4–6 weeks. The 82Rb is administered by remote intravenous infusion and the generator can be eluted with >90% yield every 10 min. 82Rb is a potassium analogue and it crosses the capillary membrane rapidly, partly using the sodium–potassium exchange transporter. It has a first pass extraction of 65%, which is higher than the 99mTc SPECT tracers but similar to thallium-201. At high values of perfusion the extraction becomes rate limiting and the linearity of uptake falls.6 The half-life of 82 Rb of 75 s allows rapid serial imaging at rest and during stress and it also leads to a lower radiation exposure for the patient than with the SPECT tracers. A fluorine-18 (18F) labeled perfusion tracer, flurpiridaz, is undergoing phase 3 clinical trials. It is a mitochondrial agent that has high myocardial extraction over a wide range of perfusion and good tracer retention without significant redistribution.7 It does not require a generator or an Table 1 The characteristics of the most commonly used cardiac PET tracers 15 13 82 9.96 Cyclotron Excellent (0.57 mm) 1.3 Generator Good (2.60 mm) Uptake 2.03 Cyclotron Very good (1.02 mm) Free diffusion Metabolic trapping (Na+/K+ ATPase) First pass extraction fraction Exercise stress Relationship with blood flow Perfusion images? Absolute measurement of perfusion? ∼100% No Linear No Yes Free diffusion and metabolic trapping (Na+/K+ ATPase) ∼80% Yes Non-linear Yes Yes O-Water Half-life (min) Production Resolution (RMS β+ range in water) British Medical Bulletin 2013;107 N-Ammonia Rb-Chloride ∼65% No Non-linear Yes yes 89 P. Arumugam et al. on-site cyclotron because the 110 min half-life of 18F means that it can be produced remotely. If the tracer is approved for clinical use and is affordable, the quality of its images and its versatility are likely to lead to a more widespread use of MPS PET. Physical characteristics Lead collimators are required in SPECT to form images only from photons that travel perpendicularly to the detector face. This leads to relatively low sensitivity but the PET technique does not require a collimator and has higher sensitivity, typically by two to three orders of magnitude (Fig. 1). The spatial resolution of PET is also superior to SPECT, although resolution recovery can improve the resolution of SPECT. The typical resolution of PET is 5–7 mm compared with 10–14 mm for SPECT. The finite distance travelled by an emitted positron before annihilation to produce two 511 keV photons travelling in opposite directions can limit PET resolution, and this is highest with 82Rb (see Table 1). Attenuation (absorption) of photons occurs as they traverse the patient. The amount of attenuation depends on the distance and the density of tissue involved. Scatter occurs when a photon is deflected from its original course by an object within its path and the photon is detected in a different part of the detector from its origin. Both attenuation and scatter artefacts can degrade image quality and lead to erroneous estimation of tracer distribution. This is a particular problem in obese patients. Both attenuation correction (AC) and scatter correction (SC) are much more accurate for PET than for SPECT, and attenuation artefact is less commonly encountered. Therefore this also gives PET the potential for absolute quantitation of tissue tracer concentration and hence kinetic modelling for the measurement of absolute myocardial perfusion. Fig. 1 Effect of collimation on detector sensitivity. Absolute perfusion measurement PET is the most accurate non-invasive method of measuring myocardial perfusion and perfusion reserve (MPR: the ratio of stress to rest 90 British Medical Bulletin 2013;107 MPS using rubidium-82 PET blood flow).5 FFR and myocardial perfusion and perfusion reserve measurements probably represent different pathophysiological processes — the former is influenced by epicardial disease processes, both focal and diffuse and the latter in addition is affected by changes in the microcirculation. A detailed discussion of the difference between FFR and MPR is beyond the scope of this article and further reading of the article by Lance Gould is recommended.8 15O water is the ideal perfusion tracer because of the linear relationship between perfusion and tracer uptake but, because it does not produce images, 13N-ammonia is a more practical standard. Both require an on-site cyclotron and so the generator produced 82 Rb is now more commonly used.9 Various software applications are available for the quantification of myocardial perfusion using 82Rb PET and the results compare favorably with other validated methods.10–12 The normal ranges for stress and rest perfusion vary according to the technique used and resting perfusion is dependent upon heart rate, systolic blood pressure and vascular resistance. The values for 82Rb tend to be lower than that for 13N-ammonia and 15O-water. Imaging protocol The protocol used in our centre for adenosine 82Rb PET is shown in Fig. 2. The patient is positioned with arms above the head and is inside the scanner for the duration of the protocol, ∼30 min. Staff are outside the scan room and the patient is monitored remotely using CCTV, two-way intercom, electrocardiogram (ECG) and blood pressure monitoring. A CT scout view is acquired to localize the left ventricle, followed by a low-dose CT for AC of the emission data (CTAC). Two emission images are acquired, typically rest followed by stress, with intravenous 82 Rb infusion from the generator using a semi-automated process. Exercise is difficult within the scanner (Fig. 3) and so stress is exclusively pharmacological using adenosine or regadenoson. The procedure is short compared with 4–6 h for a 1-day stress/rest 99m Tc protocol or two separate visits of ∼90 min for a 2-day 99mTc protocol. There are therefore significant benefits for patient time, and staff equipment contact time is also reduced. Fig. 2 Routine clinical imaging protocol for 82Rb cardiac PET. British Medical Bulletin 2013;107 91 P. Arumugam et al. Fig. 3 Patient positioning during the stress test and PET imaging. Image interpretation PET perfusion images from 13N-ammonia and 82Rb are displayed in the same way as SPECT and hence reflect relative tracer distribution. However, the stress images are acquired during stress and so the information on left ventricle (LV) function from the ECG-gated acquisition reflects peak stress rather than the post-stress state for SPECT. Image interpretation is similar to SPECT, although the higher resolution and attenuation correction mean that normal appearances differ. Normal values for myocardial perfusion depend upon the software used but normal resting perfusion range is 0.6–1.2 ml/g/min with a normal vasodilator perfusion reserve >2.13 Clinical application Comparison with SPECT Both SPECT and PET images show relative tracer uptake but PET has better resolution, higher counts and more accurate attenuation and scatter correction. Bateman et al.14 compared 82Rb PET with 99mTc-MIBI SPECT in patients who were well matched for physical and clinical variables. Image quality was better with PET than SPECT and they were 92 British Medical Bulletin 2013;107 MPS using rubidium-82 PET interpreted with greater certainty as either normal or abnormal. The diagnostic accuracy for 50 and 70% coronary artery stenosis was better with PET irrespective of gender or BMI, and the identification of multivessel disease was also improved. While this study confirmed the superiority of PET, there were some limitations. SPECT attenuation correction was not used and image reconstruction was with filtered back projection, whereas PET images were reconstructed iteratively. The short half-life of 82Rb means reduced radiation exposure for patients. In our institution, the estimated effective dose for 2 × 1110 MBq 82 Rb is 2.8 mSv (using published dosimetry data15 and International Commission on Radiological Protection 103 tissue weighting factors). After including the CTAC dose, the total effective dose of 3.6 mSv is similar to a CT coronary angiogram and lower than 99mTc SPECT performed with the current ARSAC maximum diagnostic reference levels16 (12 mSv for 2 × 800 MBq 99mTc-tetrofosmin and 16 mSv for 99m Tc-MIBI, plus any additional dose from CTAC, although individual centers may administer less than the recommended maximum).82Rb MPS also offers considerable reductions in staff dose due to the short half-life of 82Rb and reduced patient contact during administration.17 Diagnostic accuracy of perfusion PET The sensitivity and specificityfor the detection of angiographically defined coronary stenosis in the study by Al-Mallah et al was 89% and 90% respectively in 877 patients studied by both 13N-ammonia and 82Rb MPS.18 In the study by Bateman et al., the accuracy of 82Rb MPSfor the detection of a 70% coronary stenosis was 89%, and for a 50% stenosis it was 87%, which was superior to SPECT (79% and 71% respectively).14 A meta-analysis by Jaarsma et al.19 compared the diagnostic accuracy of myocardial perfusion imaging using SPECT, PET and CMR from 166 studies (114 SPECT, 15 PET and 37 CMR. The pooled sensitivities were 88%, 84% and 89% specificities 61%, 81% and 76%, and diagnostic odds ratios 15.3, 36.5 and 26.4 respectively. However this review compared PET and SPECT using all tracers and protocols. Perhaps the most comprehensive review of the diagnostic accuracy of 82RbMPS was published by Mc Ardle et al.20 who included 15 82Rb and 8 99mTc studiesbut SPECT studies only with recent technical developments. The pooled sensitivities were 85% and 90% for SPECT and PET, specificities 85% and 88%, and DOR 28.8 and 56.7. The conclusion was that 82Rb MPS is more accurate than modern SPECT MPS. British Medical Bulletin 2013;107 93 P. Arumugam et al. Prognostic value of PET MPS The prognostic value of SPECT MPS has been established in tens of thousands of patients and a normal scan is associated with an annual hard cardiac event rate of less than 1%. The number of patients included in the PET MPS data is currently in the thousands but data is accumulating and the hard cardiac event rate in a setting of a normal PET MPS is also quoted to be less than 1%.21 A recent multicentre trial included >7000 patients who underwent 82Rb MPS and were followed for a mean of 2.2 years. The extent and severity of ischaemia and scar added incremental prognostic value compared with CAD risk factors (age, female sex, BMI, hypertension, diabetes, dyslipidaemia, smoking, angina, beta blocker use, prior revascularization and resting heart rate).22 PET MPS reclassified risk in terms of cardiac death in 11.6% of patients compared with risk factors and hence potentially changed patient management. The peak stress ejection fraction also adds prognostic value as does the ejection fraction reserve (increase in ejection fraction points during peak stress compared with rest) as reported by Dorbala et al.23 Clinical application of absolute myocardial blood flow with PET Quantitative PET is likely to be helpful in two groups of patients with multivessel disease—balanced ischaemia (Fig. 4) and estimating ischaemia in a territory supplied by less severe stenosis (Fig. 5). Two studies involving a small number of patients showed the diagnostic role of myocardial perfusion and perfusion reserve in patients with multivessel disease. Parkash et al.4 compared relative perfusion with quantification of 82Rb retention at stress and at rest. Of the 23 patients, 13 had multivessel disease and the defect size was significantly larger with quantification than with qualitative imaging. In 10 patients with single vessel disease, quantification underestimated defect size slightly. A study assessing 82Rb myocardial perfusion reserve (MPR) and qualitative imaging in multivessel disease showed that a global perfusion reserve of <2 predicted threevessel disease and a reserve of >2 virtually excluded three-vessel disease.24 Ziadi et al.25 demonstrated the independent and incremental prognostic value of MPR using 82Rb MPS. This prospective study included nearly 700 patients and those with abnormal perfusion reserve had more hard cardiac events than those with a normal perfusion reserve. In addition, all cardiac deaths were in patients with the perfusion reserve <1.5, and a reduced perfusion reserve in a single territory was associated with a higher event rate than with a normal perfusion reserve in all three territories. A larger study by Murthy et al.26 followed 2783 patients referred for 82Rb MPS for a 94 British Medical Bulletin 2013;107 MPS using rubidium-82 PET Fig. 4 A 77-year-old male presented with NSTEMI (troponin rise but no localizing ECG changes). Coronary angiography showed proximal RCA disease and a probable LMS stenosis. Relative perfusion PET images on the bottom left showed homogenous tracer uptake. However, quantification showed globally impaired MPR in agreement with the angiographic findings. Image reproduced with permission from Cardiology News 2012;15(5). Copyright 2013 Pinpoint Scotland Ltd. median of 1.4 years. Compared with perfusion reserve >2, a perfusion reserve between 1.5 and 2 was associated with a 5.7-fold increased risk and a perfusion reserve <1.5 with a 16-fold increased risk for cardiac death. The addition of perfusion reserve led to the reclassification of 34.8% intermediate-risk patients, and corresponding improvements in risk assessment for mortality from any cause were also seen. The points to deduce from these studies are that a perfusion reserve <2 carries an adverse prognosis even in the presence of normal or mildly abnormal images and a perfusion reserve <1.5 is associated with higher likelihood of cardiac death. PET can also be useful when coronary anatomy is known, because quantification provides accurate information on the functional significance of a coronary lesion and this can be used for management decisions. In patients with CAD, both the hyperaemic response and perfusion reserve are inversely and non-linearly related to stenosis severity.27 British Medical Bulletin 2013;107 95 P. Arumugam et al. Fig. 5 A 57-year-old obese male presented with typical angina. 82Rb images showed inducible ischaemia in the inferior and inferolateral myocardium (arrow). Quantification however showed global reduction in perfusion reserve including the apparently normally perfused LAD territory (anterior wall and the septum arrowhead). Interestingly, there is evidence of reduced perfusion during adenosine stress compared with rest suggesting coronary steal in the area that is most ischaemic (RCA and LCx territories). Angiography showed chronic occlusion of the RCA, stenosis in the LAD and diffuse LCx disease. Image reproduced with permission from Cardiology News 2012;15(5). Copyright 2013 Pinpoint Scotland Ltd. Another clinical situation where quantification is useful is in heart failure where perfusion reserve can be reduced by microvascular dysfunction. When perfusion reserve is normal, this excludes an ischaemic aetiology for LV dysfunction and confers a better prognosis than when it is reduced28 (Figs 6 and 7). Cost-effectiveness data An early paper comparing the cost-effectiveness of exercise ECG, SPECT, PET and coronary angiography concluded that in patients with an intermediate pre-test likelihood of CAD, PET is the most cost-effective strategy and in high likelihood patients it is invasive coronary angiography.29 In a more recent study of intermediate likelihood patients that assessed the impact of 82Rb MPS compared with SPECT on subsequent invasive 96 British Medical Bulletin 2013;107 MPS using rubidium-82 PET Fig. 6 Dilated cardiomyopathy with globally reduced MPR. However, it is difficult to distinguish between balanced three-vessel ischaemia and microvascular dysfunction because of abnormal left ventricle (LV) remodelling. Reduced perfusion reserve is associated with a poor prognosis. Fig. 7 A patient with renal impairment and progressively declining LV systolic function (LVEF 34%). PET perfusion images show hypertrophy with no inducible perfusion abnormality. MPR is normal, which signifies a better prognosis and invasive angiography was avoided. procedures and outcomes, PET reduced the need for invasive angiography and coronary artery bypass grafting by 50% with a 30% cost saving.30 Disadvantages and limitations of cardiac PET PET cameras are expensive, as are cyclotrons and the 82Rb generator. This makes it economically non-viable to set up a pure MPS PET service. However, availability of oncology PET scanners has made it feasible to consider MPS PET in departments with a high demand for MPS SPECT. Due to the short half-life of current PET tracers, it is challenging to British Medical Bulletin 2013;107 97 P. Arumugam et al. perform exercise studies and hence the majority of patients are stressed pharmacologically. The normal ranges for quantitative stress and rest MBF [and hence myocardial flow reserve (MFR)] vary depending on the tracer used due to the difference in tracer kinetics. Although there is emerging data on how MFR could potentially impact patient management, there is as yet limited cost-effectiveness and outcome data on MPS PET. Clinical MPS PET services in the UK In the USA, there are procedure guidelines and appropriateness criteria for PET MPS with >200 centres routinely using the technique.31,32 82Rb and 13N-ammonia MPS have class I indications for diagnosis and prognostication in patients with intermediate or high likelihood of CAD and a previous inconclusive SPECT study. It has a class IIa indication for patients who are able to exercise or patients with an interpretable ECG as the initial diagnostic non-invasive test.33 The ‘Evidence based indications for the use of PET CT in the United Kingdom’, recommend the use of both 13N-ammonia and 82Rb MPS as alternatives to SPECT.34 Against this 82Rb MPS is currently available in only two centres: at our institution and at University College Hospital, London. The limiting factor for more widespread use is lack of access to PET scanners because of the high demand for oncology PET scans and the expense of installing a cyclotron or purchasing an 82Rb generator. Conclusion PET MPS is an emerging technique for non-invasive assessment of myocardial ischaemia with excellent imaging characteristics and tracer kinetics and the ability to quantify myocardial perfusion. 82Rb MPS is accurate for diagnosis of CAD and there is prognostic benefit from the addition of measurements of perfusion reserve. However, most of the evidence is from single centres with relatively short-term follow-up and it remains to be seen whether these results can be reproduced in larger multicentre trials. For PET MPS, or for any new technique to become main stream, it is not just enough to establish equivalent diagnostic accuracy but also to prove that the test is cost-effective and improves patient outcome. Conflict of interest Parthiban Arumugam has received speakers fee from Siemens Healthcare. The Nuclear Medicine Department at Central Manchester Hospitals has received funding for a PhD student from Siemens Healthcare. 98 British Medical Bulletin 2013;107 MPS using rubidium-82 PET References 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 British Medical Bulletin 2013;107 Pijls NHJ, Fearon WF, Tonino PAL et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the FAME (fractional flow reserve versus angiography for multivessel evaluation) study. J Am Coll Cardiol 2010;56:177–84. De Bruyne B, Pijls NHJ, Kalesan B et al. Fractional flow reserve—guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012;367:991–1001. Shaw LJ, Narula J. Risk assessment and predictive value of coronary artery disease testing. J Nucl Med 2009;50:1296–306. Parkash R, deKemp RA, Ruddy TD et al. Potential utility of rubidium 82 PET quantification in patients with 3-vessel coronary artery disease. J Nucl Cardiol 2004;11:440–49. Knuuti J, Kajander S, Maki M. Quantification of myocardial blood flow will reform the detection of CAD. J Nucl Cardiol 2009;16:497–506. Klein R, Beanlands RSB, deKemp RA. Quantification of myocardial blood flow and flow reserve: technical aspects. J Nuc Cardiol 2010;17:555–70. Yu M, Nekolla SG, Schwaiger M et al. The next generation of cardiac positron emission tomography imaging agents: discovery of flurpiridaz F-18 for detection of coronary disease. Semin Nucl Med 2011;41:305–13. Gould L. Does coronary flow trump coronary anatomy? JACC 2009;2:1009–23. Ziadiand MC, Beanlands RSB. The clinical utility of assessing myocardial blood flow using positron emission tomography. J Nucl Cardiol 2010;17:571–81. El Fakhri G, Kardan A, Sitek A et al. Reproducibility and accuracy of quantitative myocardial blood flow assessment with 82Rb PET: comparison with 13Nammonia PET. J Nucl Med 2009;50:1062–71. Manabe O, Yoshinaga K, Katoh C et al. Repeatability of rest and hyperemic myocardial blood flow measurements with 82Rb dynamic PET. J Nucl Med 2009;50:68–71. Klein R, Renaud JM, Ziadi MC et al. Intra- and inter-operator repeatability of myocardial blood flow and myocardial flow reserve measurements using rubidium-82 PET and a highly automated analysis program. J Nucl Cardiol 2010;17:600–16. Ghosh P. A clinical review of myocardial blood flow and coronary flow reserve with dynamic myocardial perfusion PET/CT. www.siemens.com/mi. Bateman TM, Heller GV, McGhie A. Diagnostic accuracy of rest/stress ECG-gated Rb-82 myocardial perfusion PET: comparison with ECG-gated Tc-99 m sestamibi SPECT. J Nucl Cardiol 2006;13:24–33. Senthamizhchelvan S, Bravo PE, Lodge MA et al. Radiation dosimetry of Rb-82 in humans under pharmacological stress. J Nuc Med 2011;52:485–91. Notes for guidance on the clinical administration of radiopharmaceuticals and use of sealed radioactive sources. Administration of Radioactive Substances Advisory Committee March 2006 (Rev. 2011). www.arsac.org.uk. Davidson G, Tout D, Hurley C et al. Comparative evaluation of staff dose from myocardial perfusion imaging using 82Rb PET-CT and 99mTc SPECT-CT. Eur J Nucl Med 2011;38(Suppl. 2):93–228. Al-Mallah MH, Sitek A, Moore SC et al. Assessment of myocardial perfusion and function with PET and PET/CT. J Nucl Cardiol 2010;17:498–513. Jaarsma C, Leiner T, Bekkers SC et al. Diagnostic performance of non-invasive myocardial perfusion imaging using single photon emission computed tomography, cardiac magnetic resonance, and positron emission tomography imaging for the detection of obstructive coronary artery disease: a meta-analysis. JACC 2012;59:1719–28. Mc Ardle BA, Dowsley TF, deKemp RA et al. Does rubidium-82 PET have superior accuracy to SPECT perfusion imaging for the diagnosis of obstructive coronary disease? JACC 2012;60:1828–37. Beanlands RSB, Youssef G. Diagnosis and prognosis of coronary artery disease: PET is superior to SPECT: Pro. J Nucl Cardiol 2010;17:683–95. 99 P. Arumugam et al. 22 Dorbala S, Di Carli MF, Beanlands RSB et al. Prognostic value of stress myocardial perfusion positron emission tomography results from a multicenter observational registry. JACC 2013;61:176–84. 23 Dorbala S, Vangala D, Sampson U et al. Value of vasodilator left ventricular ejection fraction reserve in evaluating the magnitude of myocardium at risk and the extent of angiographic coronary artery disease: a 82Rb PET/CT study. J Nucl Med 2007;48:349–58. 24 Ziadi MC, deKemp RA, Williams K et al. Does quantification of myocardial flow reserve using rubidium-82 positron emission tomography facilitate detection of multivessel coronary artery disease? J Nucl Cardiol 2012;19:670–80. 25 Ziadi MC, deKemp RA, Williams K et al. Impaired myocardial flow reserve on rubidium-82 positron emission tomography imaging predicts adverse outcomes in patients assessed for myocardial ischemia. JACC 2011;58:740–8. 26 Murthy VL, Naya M, Foster CR et al. Improved cardiac risk assessment with noninvasive measures of coronary flow reserve. Circulation 2011;124:2215–2224. 27 Anagnostopoulos C, Almonacid A, El Fakhri G et al. Quantitative relationship between coronary vasodilator reserve assessed by Rb-82 PET imaging and coronary artery stenosis severity. Eur J Nucl Med Mol Imaging 2008;35:1593–601. 28 Neglia D, Michelassi C, Trivieri MG et al. Prognostic role of myocardial blood flow impairment in idiopathic left ventricular dysfunction. Circulation 2002;105:186–93. 29 Patterson RE, Eisner RL, Horowitz SF. Comparison of cost-effectiveness and utility of exercise ECG, single photon emission computed tomography, positron emission tomography, and coronary angiography for diagnosis of coronary artery disease. Circulation 1995;91:54–65. 30 Merhige ME, Breen WJ, Shelton V et al. Impact of myocardial perfusion imaging with PET and Rb-82 on downstream invasive procedure utilization, costs, and outcomes in coronary disease management. J Nucl Med 2007;48:1069–76. 31 Dilsizian V, Bacharach SL, Beanlands RSB et al. ASNC imaging guidelines for nuclear cardiology procedures. PET myocardial perfusion and metabolism clinical imaging. J Nucl Cardiol 2009;16. http://www.asnc.org/imageuploads/ImagingGuidelinesPETJuly2009.pdf. 32 Hendel RC, Berman DS, Di Carli MF et al., American Society of Nuclear Cardiology. Appropriate use criteria for cardiac radionuclide imaging. Circulation 2009;119:e561–587. 33 Hendel RC, Berman DS, Di Carli MF et al. Appropriate use criteria for cardiac radionuclide imaging. JACC 2009;53:2201–29. 34 Barrington S, Scarsbrook A. Evidence based indications for the use of PET CT in the United Kingdom, 2012. http://www.rcr.ac.uk/docs/radiology/pdf/BFCR(12)3_PETCT.pdf. 100 British Medical Bulletin 2013;107