* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download File
Coronary artery disease wikipedia , lookup
Jatene procedure wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Myocardial infarction wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
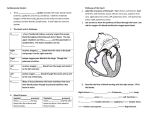
Chapter 8: The Cardiovascular & Respiratory Systems The Heart The Structure of the Heart The cardiovascular system is composed of the heart, blood vessels, and blood. The heart acts as a “pump” of the system, pushing blood through the vessels. The blood carries oxygen (O2) and nutrients to the tissues and it also carries carbon dioxide (CO2) and waste products away from the tissues. The heart if formed from specialized muscle tissue called cardiac muscle, or myocardium. The heart is about the size of a closed fist and it weighs about 250-350 grams. The heart is considered a “double pump” that is divided into a right and a left side. The two sides are separated by the interventricular septum. The main function of the right side of the heart is to pump deoxygenated blood, which has just returned from the body, to the lungs. This is known as pulmonary circulation. The main function of the left side of the heart is to pump oxygenated blood, which has just returned from the lungs, to the rest of the body. This is known as systemic circulation. Oxygenated blood is bright red in colour, while deoxygenated blood is much darker. Within the chest, a tough protective sac called the pericardium, fits loosely over the heart (since it must expand to allow the heart to expand and contract). The outer layer of the heart that lies against the pericardium is called the epicardium. Directly under the epicardium is the myocardium. Finally, the layer of tissue that lines the inside of the heart is called the endocardium. The Chambers of the Heart The heart is made up of 4 separate chambers. The upper chambers are called the atria, while the lower chambers are called the ventricles. The atria are separated from the ventricles by specialized valves that allow blood to flow only form the atria to the ventricles. These valves are called atrioventricular (AV) valves. On the right side of the heart, the atrioventricular valve is called the tricuspid valve, because it is made up of three special flaps, while on the left side of the heart, the valve is called the bicuspid (or mitral) valve since it is composed of two special flaps. These valves are attached to special muscular extensions of the ventricle walls (the papillary muscles) by strands of strong specialized tissue known as chordae tendinae. The chordae tendinae and the papillary muscles help to prevent the AV vales form being turned inside out. The pulmonary semilunar valve is located on right side of the heart where the blood leaves the ventricles to head toward the lungs. This valve prevents blood from flowing back from the pulmonary arteries into the right ventricle. On the left side of the heart, the aortic semilunar valve separates the left ventricle and the aorta. 1 The Circulation of Blood through the Heart Deoxygenated blood is delivered to the right atrium from the superior and inferior vena cava. The superior vena cava returns blood to the heart from the upper body, while the inferior vena cava returns blood from the lower body. Once the blood is in the right atrium, it passes through the tricuspid valve and enters the right ventricle. From the right ventricle, the blood is pumped through the pulmonary semilunar valve and leaves the heart through the pulmonary arteries as it heads toward the lungs. This is pulmonary circulation. Once in the lungs, the blood is now oxygenated. Now, the oxygenated blood travels from the lungs toward the heart through the pulmonary veins and re-enters the left atrium. From the left atrium, the blood travels through the bicuspid (mitral) valve and enters the left ventricle. From the left ventricle, the blood leaves the heart through the aortic semilunar valve and enters the aorta. This is systemic circulation. From the aorta, the blood is pumped throughout the body until it returns once again through the superior and inferior vena cava. Arteries are vessels that carry blood away from the heart, while veins are vessels that carry blood toward the heart. In systemic circulation, arteries carry oxygenated blood from the heart to toward body tissues, while veins carry deoxygenated blood back to the heart. In pulmonary circulation, pulmonary arteries carry deoxygenated blood from the heart to the lungs (so still exiting the heart), while the pulmonary veins carry oxygenated blood from the lungs back to the heart (so still going back into the heart). Electrical Excitation of the Heart The cardiac muscle cells are interconnected and allow the passage of electrical signals from cell to cell. The ability of these cells to transmit electrical signals allows the myocardium to contract as a single unit. The term, syncytium is used to describe this ability. 2 The SA Node and Its Functions The cardiac muscle cells that make up the myocardium are excitable, meaning that with electrical stimulation they will contract. Within the heart, there are areas of specialized tissue that are important in the regulation and coordination of this electrical activity. One specialized region of tissue is found in the wall of the right atrium and is called the sinoatrial node (SA node). The SA node is also called the heart’s pacemaker because it is the location where electrical signals are initiated which then leads to the contraction of the heart. The base rate of contraction of the heart is set by the SA node and is modulated by the autonomic nervous system. The SA node, without any input from the nervous system, will cause the heart to contract at approximately 60-80 beats per minute. In situations where the SA node is damaged, the AV node takes control and becomes the pacemaker of the heart. The AV Node and Its Functions The electrical signal then travels to the bottom of the atria and passes into another specialized region of tissue called the atrioventricular node (AV node). The AV node transmits the electrical signal from the atria into the ventricles. It transmits this electrical signal down specialized tissue that runs down the ventricular septum (the tissue that separates the two ventricles). This specialized tissue within the ventricular septum is called the bundle and left bundle branches. The bundle branches pass the signal on to the Purkinje fibres, which in turn pass the electrical signal to the myocardium that forms the ventricles. This arrangement of specialized tissue allows the contraction of the heart to be initiated in the atria from the top downward, pushing blood into the ventricles. The ventricles then contract from the bottom up, forcing blood into the pulmonary arteries and the aorta. The electrical activity of the heart can be measured using an instrument known as an electrocardiogram of His, which splits to form right (ECG). The ECG provides a graphical representation of the electrical sequence of events that occurs with each contraction of the heart. Contractions are represented as depolarizations (i.e.: the P wave shows atrial depolarization which means that the atria are contracting). Relaxations are represented as polarizations (i.e.: the T wave shows ventricle repolarization which means that the ventricle is relaxing). 3 The Vascular System and Blood Flow The vascular system is formed by a network of vessels that transport blodo throughout the body. Arteries are vessels with very thick muscular walls, and carry oxygenated blood from the heart to the different tissues and organs of the body. The walls of the arteries are very elastic and can stretch and then recoil back to their original diameter. This ability to stretch and recoil assists in the movement of blood during. Systolic blood pressure is the pressure caused by the contraction of the heart (and is the upper number in our blood pressure reading), while distolic blood pressure is the pressure caused by the recoiling of the arteries (and is the lower number in our blood pressure reading). Normal blood pressure should be around 120/80. Arterioles are smaller than the arteries and are important in the regulation of blood distribution to the various tissues of the body. They are surrounded by rings of smooth muscle which can contract and relax. These rings of smooth muscle are controlled by the nervous system as well as chemical factors released by tissues that are supplied by the arterioles. For example, during exercise, the arterioles that supply the muscles involved in the exercise would be open therefore increasing blood flow to the muscle. At the same time, the arterioles that supply the intestines would be constricted therefore reducing blood flow to this organ. In general, blood flow is influenced by a process known as autoregulation. Capillaries are the smallest vessels within the body, and are very thin (only one cell thick). Once blood travels through the capillaries, it then enters the venules (smaller sized veins) which lead to the veins. Veins are blood vessels that carry deoxygenated blood from the body back to the heart (leading to the superior Despite being so small, there are millions of capillaries within the body – all body tissues have an extensive supply of capillaries. All of our capillaries lined up would be more than 40 000 km long! Capillaries are responsible for gas exchange as well as exchange of all waste and nutrients. For example, if the concentration of oxygen gas is high in the blood but low in the cells of our tissue, oxygen gas will diffuse from our capillaries into our tissues, while carbon dioxide will diffuse from our cells into our capillaries where it will be carried back to our lungs to be exhaled. and inferior vena cava). The walls of veins contain smooth muscle which allows the veins to dilate and contract, similar to arterioles. Veins also have one-way valves to aide blood in travelling back up toward the heart. The low pressure within the veins creates a problem for the cardiovascular system. So, our cardiovascular system has three tools to help the blood continue to pump: The skeletal muscle pump – with each contraction of a skeletal muscle, blood is pushed or massaged back to the heart. 4 The thoracic pump – this is related to breathing. With each breath taken, pressure in the chest cavity is very low for a few short seconds, while the pressure in the abdominal cavity increases – this change in pressure pushes blood form the veins in the abdominal cavity into the veins of the thoracic cavity. The nervous system – it will send signals to the veins, causing them to slightly restrict (venoconstriction) which allows more blood to return to the heart. Blood and Its Components Blood is the specialized fluid that is found in the heart and all of the vessels. Blood’s main role is to act as a transport medium for O2, CO2, and nutrients. Blood is made up of two components: plasma and blood cells. Plasma is the fluid component of blood and is mainly composed of water. Plasma makes up 55% of blood. Within the plasma there are dissolved substances such as nutrients, proteins, ions, and gases. The blood cells make up the other 45% of blood. Red blood cells (erythrocytes) make up most of this amount. Erythrocytes are specialized cells that transport O2 and CO2 in the blood. They contain a specialized protein called hemoglobin, which can bind O2 and CO2. White blood cells (leukocytes) make up less than 1% of our blood and play an important part of the body’s immune system. They help to protect the body against disease. Platelets are the 3rd type of blood cell found in our blood. Platelets are actually fragments of cells and are important in the regulation of blood clotting. Cardiovascular Dynamics The heart and the vessels must constantly adapt to accommodate the ever-changing requirements of the body. Cardiac Output (Q) Cardiac output (Q) is the volume of blood pumped out of the left ventricle in one minute. It is measured in L/min. At rest, a typical person’s cardiac output will be approximately 5-6 L/min, but during heavy exercise, cardiac output can increase to more than 30 L/min. Two factors affect cardiac output: stroke volume (SV) x heart rate (HR). For example, if an individual’s HR at rest was 72 beats/minute and the stroke volume was 71 mL, the cardiac output (Q) would be 72 x 71 = 5.04 L/min. 5 Stroke volume is the amount of blood that is ejected from the left ventricle in a single beat and is measured in mL. Stroke volume is regulated by three main factors: left ventricular end-diastolic volume (LVEDV – it is the amount of blood that is returned to the ventricle before it contracts); aortic blood pressure; and the strength of the ventricular contraction. During exercise, venous return increases as the result of four main factors: constriction of the veins (venoconstriction); the skeletal muscle pump; the thoracic pump; and the nervous simulation of the heart. The efficiency of an individual’s stroke volume is measured through the calculation of ejection fraction (EF) which is the proportion of blood that is ejected from the left ventricle during a single heartbeat. On average, EF at rest is 50-60% and it increases during exercise to a maximum of 85%. Heart rate (HR) is the number of times the heart contracts in a minute (beats per minute). The healthier (fitter) an individual, the higher his/her stroke volume as the heart is better and more effective at pumping large amounts of blood each time it contracts. This also means that the fitter individual will also have a lower resting heart rate as his/her heart does not need to beat as often since each contraction of the ventricle allows so much blood to move through the body. During exercise, cardiac output can increase to 15-20 L/min, or more. The increase in Q occurs very early in the exercise and then becomes constant at the new higher level. These increases are mediated by the SV and the HR increasing. If the exercise is prolonged, there might be a slight decline in SV and Q. This decline is due to excessive fluid loss from the body due to sweating. Despite the slight decline in SV, Q is maintained with a gradual increase in HR. These changes in SV and HR, while Q is maintained, are known as the cardiovascular drift. The cardiovascular drift is characterized by a slow and steady rise in HR and a corresponding decline in SV. It is results from the physiological changes associated with the increase in body temperature that occurs during exercise. Some of these changes include a decline in plasma volume, redistribution of blood flow to the skin, and dehydration. Blood Pressure The cardiac cycle is the series of events that occurs through one heartbeat. During this cycle, there is both a phase of relaxation (diastole) in which the ventricle is filling with blood, and a phase of contraction (systole), in which the heart contracts and ejects the blood. Blood pressure in each of these phases is measured in millimetres of mercury (mmHg). Systolic blood pressure is the maximum pressure observed in the arteries during the contraction phase of the ventricle (for example, 120 mmHg). Diastolic blood pressure is the minimum pressure observed in the arteries during the relaxation phase of the ventricle (for example, 80 mmHg). Blood pressure is the force exerted by the blood against the walls of the arteries and other vascular vessels. During the cardiac cycle, the dramatic changes in pressures propel the blood through the circulation. The changes create pressure waves that are measured in the arteries. When blood pressure readings are taken, it is reported as systolic blood pressure over diastolic blood pressure. On average, people should have blood pressure readings between 90/60 to 120/80 mmHg. During exercise, large changes can occur to blood pressure. During acute aerobic or endurance exercise, there tends to be a sustained increase in systolic blood pressure, but no change in diastolic blood pressure. The increase in systolic blood pressure is often proportional to the exercise intensity – the greater the exercise intensity, the greater the rise in systolic blood pressure. 6 Resistance exercise (like weightlifting) can result in very short, but very large increases in both systolic and diastolic blood pressures. And, just like with endurance exercise, the greater the intensity of the resistance exercise, the greater the increase in both types of blood pressures. Following exercise (both endurance and resistance) there is a prolonged period where blood pressure drops below normal resting values. This is known as post-exercise hypotension. Persistently elevated blood pressure is known as hypertension and is pressure greater than 140/90 mmHg, and it is a major risk factor for cardiovascular disease. Hypertension can be caused by obesity, smoking, aging, kidney disease, and genetic factors. Aerobic exercise leads to improvements in resting blood pressure in people with moderate to high blood pressure within 3 weeks. Blood Flow Distribution During exercise, the working skeletal muscle has an increased need for O2, and the cardiovascular system attempts to match the delivery of O2 to meet this need by altering the blood flow distribution. This increase in the delivery of O2 is met in two ways: An increase in cardiac output (Q), and a redistribution of blood flow. The system increases the amount of blood flow that is directed to the working muscle while blood flow to less active organs (like the stomach, intestine, and kidneys) decreases. The Cardiovascular Effects of Training Regular aerobic exercise has been shown to result in improvements in efficiency in the cardiovascular system at rest, during submaximal exercise, and during maximal exercise. The most influential changes that occur with aerobic training and exercise are alterations in the structure of the heart. The heart increases in mass and dimensions. As well, there are increases in ventricular volume and the thickness of the ventricle wall. This increase in ventricular volume leads to an increase in SV (stroke volume), while the increase in ventricular wall thickness leads to an increased force of contraction of the ventricle. Both of these factors contribute to an increase in SV and therefore Q (cardiac output) during exercise. There is also an increase in the number of capillaries that deliver blood to the myocardium. This is in response to the increase in O2 demands of the heart during prolonged exercise. There is also an increase in blood volume. The total volume of plasma can actually increase by 15% within 2 days of starting a training program. HR (heart rate) is decreased at rest and during submaximal exercise. This decrease in HR is referred to as bradycardia, which is characterized by a heart rate of 60 beats per minute or less at rest. Tachycardia is a heart rate of 100 or more beats per minute at rest. 7 The Respiratory System The respiratory system is composed of structures that allow the passage of air from outside the body to the lungs. The three main functions of the respiratory system are to: Supply O2 to the blood Remove CO2 from the blood Regulate blood pH (acid-base balance) External respiration is the process that occurs within the lungs involving the exchange of O2 and CO2. Internal respiration is the process that occurs at the tissue level, where O2 is delivered and CO2 is removed. Cellular respiration is the process in which the cells use O2 to generate energy through the different metabolic pathways found in the mitochondria of the cells. The actual structure of the respiratory system can be divided into two main zones: The Conductive Zone is made up of all of the structures that convey air from the outside of the body through to the lungs. It includes the mouth, nose, pharynx, larynx, trachea, bronchi, and bronchioles. By the time air reaches the respiratory zone, it is at body temperature (37°C) and is almost completely saturated with moisture. Another role of the conductive zone is that it filters air that is taken in with each breath – the nasal cavity is lined with hairs to trap foreign bodies and prevent them from being inspired. The Respiratory Zone is composed of the respiratory bronchioles, alveolar ducts and sacs. All of these structures are involved in the exchange of gases between inspired air and the blood. The alveolar sacs provide a large surface area and are surrounded by capillaries (that provide a large surface area for blood). It is here that the diffusion of gases into and out of the blood occurs. As well, all respiratory organs have moist surfaces in which the gases can dissolve and diffuse. This is known as gas exchange. On average, an adult has approximately 300 million alveolar sacs. If stretched out, all of these alveolar sacs would cover an entire tennis court. The Mechanisms of Breathing 8 In response to stimulation from the brain (at the start of a breath), the diaphragm contracts, pulling downward and enlarging the thoracic (chest) cavity. At the same time, the intercostal muscles between the ribs contract, moving the chest upward and outward. This also helps to increase the thoracic cavity. As the chest expands, the lungs expand as well. The pressure in the lungs becomes negative relative to the air outside. The lower air pressure causes air to rush into the lungs. This is known as inhalation and it allows the pressure to become equalized (both inside the lungs and outside of the body). Inspiration is an active process, requiring the contraction of various respiratory muscles (it requires energy). Once the lungs are inflated with air, the chest muscles and diaphragm relax and recoil to their original positions. This decreases the size of the thoracic cavity and increases the pressure within the lungs which forces air out of the lungs into our external environment. This is known as expiration. Expiration is a passive process, and requires very little energy to occur. Ventilation (VE) is the combination of inspiration and expiration. Ventilation is the volume of air that is moved by the lungs in one minute. Ventilation is influenced by two factors: the volume of air in each breath; and the number of breaths taken per minute. The volume of air in each breath is known as the tidal volume (VT). At rest, VT is about 0.5 L/breath, while during exercise, VT can increase to 3-4 L/breath. The number of breaths taken per minute is known as the respiratory frequency (f). At rest, a typical respiratory frequency is around 12 breaths/minute, and during exercise, it can increase to approximately 40 breaths/minute. Gas Exchange and O2 and CO2 Transport Diffusion is the main factor that mediates gas exchange at both the lung and at the tissue levels. Diffusion is the movement of a gas, liquid, or solid from a region of high concentration to a region of low concentration. Such a difference in concentrations is called a concentration gradient. The rates of diffusion of a gas between two different areas depend on a number of factors. The 1st factor is the size of the concentration gradient – as the concentration gradient increases, so does the rate of diffusion. The partial pressure (meaning that the relative percentage of each gas stays the same in the air, but the actual partial pressure of each gas is dependent upon changes in air pressure) of oxygen within the alveoli is a PO2 of 105 mmHg, while the PO2 in the deoxygenated blood as it enters the lungs is only 40 mmHg. This creates a diffusion gradient, which mediates the diffusion of O2 into the blood. The 2nd factor is the thickness of the barrier between the two areas where diffusion occurs. Within the lungs, the distance between the alveoli and the capillaries that surround them is extremely small (only two cells thick) which optimizes diffusion. The 3rd factor is the surface area between the two areas where diffusion occurs. Our lungs have a huge surface area for diffusion – both the alveoli and the capillaries are built to provide an extremely large surface area so that diffusion can occur as quickly as possible. Oxygen Transport O2 transport is the process by which oxygen is absorbed in the lungs by the hemoglobin in circulating deoxygenated erythrocytes (red blood cells) and carried to the peripheral tissues. 9 O2 transport is achieved in two ways: The 1st way is a small amount of O2 is actually dissolved in the plasma (about 2% of the O2 found in blood). The 2nd way in which O2 is transported is by binding to hemoglobin (specialized protein found in erythrocytes). Each gram of hemoglobin has the ability to bind to 1.34 mL of O2. The average concentration of hemoglobin in blood is -16 mg/100 mL of blood. This means that the average O2 carrying capacity for blood is -21.4 mL O2/100 mL of blood. Carbon dioxide Transport CO2 transport is the process in which carbon dioxide is moved from body tissues, where it is produced, back to the lungs where it can be moved into the alveoli and then exhaled and removed from the body. CO2 transport happens in three ways: The 1st way is a small amount of CO2 is found dissolved in the plasma (about 5-10% of CO2 is transported dissolved in the plasma). The 2nd way is by binding to hemoglobin (about 20%) forming what is known as carbaminohemoglobin. Once the blood arrives at the lungs, the elevated concentrations of O2 stimulate the hemoglobin to release the CO2, when then diffuses out into the alveoli and is exhaled. The 3rd way is through the bicarbonate system. The remaining 70-75% diffuses into the erythrocytes, but undergoes a chemical reaction with water to form a weak acid called carbonic acid. This chemical reaction occurs because of a specialized enzyme found in the erythrocytes called carbonic anhydrase. Once formed, the carbonic acid then dissociates, forming a hydrogen ion and a bicarbonate ion. The resulting H+ ions bind to hemoglobin, while the bicarbonate ions diffuse into the plasma. Ventilation and the Regulation of Blood pH Ventilation plays an important role in the regulation of the pH of the blood. Generally, blood pH is maintained very close to a pH of 6.4. However, in situations in which large amounts of acid are released into the blood, such as during exercise (the release of lactic acid), results in a decrease in blood pH. A decrease in pH (an increase in acidity) means that there is an increase in the accumulation of H+ ions in the blood. When ventilation is increased, it increases the amount of CO2 expelled. This means that now more H+ ions can combine with bicarbonate to form carbonic acid, and eventually CO2 and H2O. This will lower the concentration of H+ions, therefore increasing pH levels. Respiratory Dynamics During exercise, the body responds to the increased need for oxygen at the working muscles through a series of responses that attempt to match oxygen delivery with oxygen demand. Exercise results in increases in pulmonary ventilation, external and internal respiration, and cellular respiration. Pulmonary Ventilation (VE) Pulmonary ventilation (VE) is the exchange of air between the lungs and the environment, including inhalation and exhalation. 10 It is closely matched to the rate and/or intensity of the work being done. The increases in V E that occur with submaximal exercise can be divided into three phases: The 1st phase is terms the rapid on phase. VE is increased at a very rapid rate, almost immediately upon the onset of activity. The 2nd phase is characterized by a slower exponential increases from the rapid increase observed in the 1st phase. The 3rd phase is characterized by a levelling off of VE at a new steady-state level. The increases in VE are due initially to a rise in VT (tidal volume), and then, as exercise continues, a rise in f (breathing frequency). With more intense exercise, f will increase to a greater extent to accommodate the increased demands for VE. External Respiration External respiration is the total gas exchange at the lungs. It increases as a result of two main factors: The increase in VE. The increase in VE serves to maintain the necessary gradient in the partial pressures of both O2 and CO2, to maintain gas exchange. The increase in blood flow to the lungs. The increase in gas exchange is closely matched to the increase in requirements of the working skeletal muscles. Internal Respiration Internal respiration involves the exchange of gases at the level of the tissues. It is the extraction of O2 at the tissues increasing due to an increase in exercise levels. It occurs as a result of 4 main factors: a) an increase in in the PO2 gradient, b) an increase in PCO2, c) a decrease in pH, and d) an increase in temperature. During exercise, the skeletal muscle increases cellular respiration, and O2 is used to generate ATP. This increase in the use of O2 results in a decline in the PO2 within the skeletal muscle, and increases the gradient between the PO2 within the blood and the muscle. The increase in the gradient further enhances the diffusion of O2 out of the blood into the working muscle. The increase in muscle activity results in an increase in CO2 production, a decline in pH (resulting from increases in CO2 and lactic acid), and an increase in temperature. These three factors influence the binding of O2 with hemoglobin and result in an increase in the uploading of O2. Essentially, the alteration in CO2, pH, and temperature contribute to what is known as the Bohr shift. It is the enhanced uploading of O2 at the working muscle, contributing to the increase in internal respiration that occurs during exercise. Respiratory Disease Asthma is a disease characterized by spasm of the smooth muscles that line the respiratory system, an oversecretion of mucous, and swelling of the cells lining the respiratory tract. Together, these changes result in shortness of breath (known as dyspnea), and wheezing sounds during breathing. Many factors can lead to an asthma attack such as, exercise, allergic reactions, contaminates, and stress. 11 Chronic obstructive pulmonary disease (COPD) is a general term that describes a family of disease that lead to a dramatic reduction in airflow through the respiratory system. The conditions are persistent and cannot be relieved with medications. Treatment includes medications, supplemental oxygen therapy, and respiratory muscle training. The Integration of Cardiovascular and Respiratory Functions The amount of O2 taken up and consumed by the body for metabolic processes is called oxygen consumption (VO2). It is equal to the amount of O2 inspired minus the amount of O2 expired. VO2 is proportional to workload. This means that the greater the workload, the greater the VO2 (the greater the amount of O2 used by the body). Maximal rate of oxygen consumption (VO2max) is defined at the maximal amount of O2 that can be takin in and used for metabolic production of ATP during exercise. It occurs at maximum SV (stroke volume) and HR (heart rate). VO2max is used as a measure of aerobic fitness, and is indicative of aerobic exercise performance. VCO2 is calculated by measuring the difference between the amounts of CO2 expired and the amount of CO2 inspired. The ratio between VO2 and VCO2 is used to calculate the respiratory exchange ratio (RER). RER is indicative of what metabolic systems are being used within the working muscle. The amount of CO2 produced and O2 consumed varies, depending on what fuels are being used by the working muscle. When fat is being oxidized and used to produce ATP, more O2 is consumed as compared to the amount of CO2 produced. When carbohydrates are the major fuel source, not as much O2 is consumed relative to the amount of CO2 produced. It is believed that the biggest limiting factor for VO2max is the cardiovascular system. If the cardiovascular system is unable to meet the demands of the working muscle and deliver adequate amounts of O2, then Q (cardiac output) becomes the main limiting factor to VO2max. The Rest-to Exercise Transition The delivery of O2 to the working skeletal muscle is achieved through a combination of physiological mechanisms – the delivery of O2 is matched by the demand of O2. However, the physiological mechanisms are not instantaneous – there is a “lag” between the initiation of exercise and the achievement of a new steady state. “Steady state” means sub-maximal exercise levels, where oxygen uptake and heart rate level off, and where energy demands and energy production are evenly balanced. The body can maintain a steady state of exertion for a fairly extended period of time. Eventually, all systems will be in used and O2 delivery will be matched again with O2 demand. However, during this “lag” phenomenon called oxygen deficit (O2 deficit) occurs. Oxygen deficit is the amount of oxygen taken in during stressful exercise minus the amount of oxygen that would otherwise have been required for steady-state aerobic exercise. During this time, the working muscles must partially rely on metabolic systems that do not require O2. 12 The trained individual will reach this steady-state plateau faster than an untrained individual, and therefore, will have a smaller oxygen deficit for an exercise of a given duration. Individuals can increase their aerobic capacity through proper aerobic training. Blood Lactate Accumulation During incremental exercise, pulmonary ventilation initially increases at a rate proportional to the increase in workload. However, eventually a point is reached where ventilation increases much more rapidly than workload. This point is called the ventilatory threshold, and it normally occurs at an exercise intensity that corresponds to 65-85% of VO2max, depending on one’s level of aerobic fitness. This increase in ventilation is due to an increase in the accumulation of lactic acid within the blood. The body increases ventilation to deal with the accumulation of the lactic acid in the blood and the corresponding drop in pH. Initially, blood lactate remains low, but will reach a point in which the concentrations rise exponentially. This point is referred to as the lactate threshold. The lactate threshold is closely associated with the ventilatory threshold. When lactate levels begin to accumulate rapidly (shortly after the lactic acid threshold is reached), this is referred to as the onset of blood lactate accumulation (OBLA). With proper aerobic training, the OBLA curve can be shifted to the right so that OBLA occurs later and during higher levels of intense exercise. 13