* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Acute pericarditis is the most common disease state affecting the
Survey
Document related concepts
Transcript
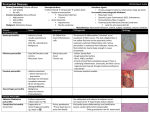
Acute Pericarditis Is the most common disease state affecting the pericardium. Most cases of acute pericarditis are idiopathic or have a viral aetiology. Other potential aetiologies include bacterial and fungal infections, rheumatologic conditions, inflammatory bowel disease, drug reactions, malignancies, uraemia, pregnancy and immunologic disorders. Patients typically complain of sharp central chest pain that worsens with recumbency during swallowing and with body motion. and is relieved by leaning forward. The pain associated with acute pericarditis may be pleuritic in nature and may radiate to the ridge of the trapezius, a sign very specific for pericardial inflammation. Physical examination may reveal the pathognomonic finding for pericarditis: the pericardial friction rub. Classically, this rub occurs in three phases. They are composed of (1) an atrial systolic rub that precedes S1, (2) a ventricular systolic rub between S1 and S2 and coincident with the peak carotid pulse, and (3) an early diastolic rub after S2 (usually the faintest). corresponding with atrial systole, ventricular systole and ventricular diastole. However, it is uncommon for all three phases to be heard clinically and, at times, the rub may be evanescent The friction rub is best appreciated by firmly applying the diaphragm to the left lower sternal border with the patient leaning forward after an exhalation. The Beck triad (ie, hypotension; elevated systemic venous pressure, often with jugular venous distention; and muffled heart sounds) may be observed in patients with cardiac tamponade, especially from sudden intrapericardial hemorrhage. Pulsus paradoxus is defined as 10 mm Hg decrease in arterial systolic pressure with inspiration. It is important in patients with more slowly developing tamponade because they may lack findings of the Beck triad. TABLE 2 Stages of Acute Pericarditis on ECG Stage Changes on ECG Stage I: Diffuse concave-upward ST-segment elevation with concordance of T waves; ST-segment depression in aVR or V1; PR-segment depression best demonstrated in leads II and V3; low voltage; absence of reciprocal ST-segment changes. ST/T ratio is greater than 0.25. Stage II: ST segments return to baseline; T-wave flattening Stage III: T-wave inversion Stage IV: Gradual resolution of T-wave inversion Classic acute or "dry" pericarditis usually results in deposition of a fibrinous material with a characteristic "bread-and-butter" appearance likened to pulling two pieces of buttered bread apart. The vascularity of the pericardium is increased, which may impart a gross red appearance with diffuse fibrin deposition and neutrophils present on microscopic examination. It is this inflammation that creates the characteristic friction rub heard on auscultation, which has been described as being "like the squeak of leather on a new saddle under a rider" Pericardium Anatomy The pericardium consists of an outer fibrous layer called the parietal pericardium and an inner serosal membrane overlying the epicardial surface called the visceral pericardium. Between these layers is a potential space normally containing approximately 20 mL of fluid, an ultrafiltrate of plasma. Drainage occurs via the thoracic duct and the right lymphatic duct into the right pleural space. Important functions of the pericardium include limiting acute distention of the heart, especially in states of volume overload, maintaining the heart in an optimal shape and position, and acting as a buttress against inflammation to prevent it from spreading to adjacent structures. It also creates a closed chamber with subatmospheric pressure that aids atrial filling and lowers transmural cardiac pressures. TABLE 1 Aetiologies of Acute Pericarditis * more common Infectious Viral. 1-10% of cases. See idiopathic Coxsackievirus* Echovirus Epstein-Barr virus Influenza virus Human immunodeficiency virus Mumps virus Bacterial. 1-8% of cases and causes purulent pericarditis Staphylococcus Hemophilus Pneumococcus. Common in pre-antibiotic era. Salmonella Meningococcus Syphilis Tuberculosis 4% of cases. Approximately half the patients develop constrictive pericarditis Miscellaneous Histoplasmosis Blastomycosis Coccidioidomycosis Aspergillosis Echinococcosis Amebiasis Rickettsia Rheumatologic Sarcoidosis Lupus* Rheumatoid arthritis Dermatomyositis Scleroderma Polyarteritis nodosa Vasculitis Ankylosing spondylitis Neoplastic Metastatic Breast Lung Lymphoma Melanoma Leukemia Primary Sarcomas Mesothelioma Drugs Hydralazine* (Apresoline) Procainamide* (Pronestyl) Others Immunologic Celiac sprue Inflammatory bowel disease Other Chest trauma Uremia* Myxedema Aortic dissection Radiation therapy Myocardial infarction* Postmyocardial infarction syndrome (i.e., Dressler's syndrome, postpericardiotomy*) Idiopathic* 26% and 86% of cases are idiopathic in nature. No clinical features distinguish these from viral pericarditis. Most likely, the majority of idiopathic cases are undiagnosed viral infections. Differential Diagnosis of Acute Pericarditis by ECG Myocardial infarction, Early repolarization, Myocarditis Pulmonary embolus, Cerebrovascular accident, Pneumothorax Hyperkalemia, Pneumopericardium, Subepicardial hemorrhage, Ventricular aneurysm Prognosis Most cases of acute idiopathic or viral pericarditis do not recur; however, acute pericarditis may recur if it is associated with an ongoing underlying illness such as an autoimmune disease or uraemia. Symptoms usually subside within two weeks; however, up to 15 percent of patients may experience a recurrence in the first few months following the initial episode. On occasion, idiopathic acute pericarditis may recur several times but will rarely lead to effusion and cardiac tamponade or constrictive pericarditis necessitating pericardectomy. Typically, physicians should schedule a follow-up visit with these patients two weeks after the onset of their illness unless problems arise sooner. An ECG should be considered at four weeks, bearing in mind that residual T-wave inversion may be present for several weeks during stage III of acute pericarditis. http://www.aafp.org/afp/980215ap/marinell.html