* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiovascular Responses
Survey
Document related concepts
Transcript
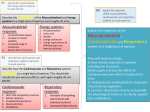
Cardiovascular Responses to Exercise Chapter Learning Outcomes • Graph and explain the pattern of response for the major cardiovascular variables during short and long-term, light to moderate submaximal aerobic exercise. • Graph and explain the pattern of response for the major cardiovascular variables during incremental aerobic exercise to maximum and during dynamic resistance exercise • Discuss the similarities and differences between the sexes in the cardiovascular response to the various classifications of exercise. Cardiovascular Responses to Acute Aerobic Exercise • Increases blood flow to working muscle • Involves altered heart function, peripheral circulatory adaptations – Cardiac output (A) • Heart rate (C) • Stroke volume (B) – Blood pressure (D) – Total peripheral resistance (TPR) (E) – Rate pressure product (RPP) (F) Figure 12.1, 12.4 & 12.7 Acute Responses to Submaximal Aerobic Ex Light to Moderate Moderate to Vigorous Steady State Exercise output = requirements • When the body can meet the metabolic and physiological demands during submaximal exercise, a “steady state” of equilibrium is achieved at values above resting. Acute Maximal Aerobic Ex Cardiovascular Responses: Cardiac Output (Q) • Q = HR x SV •Normal values – Resting Q ~5 L/min – Untrained Qmax ~20 L/min – Trained Qmax 40 L/min • Qmax a function of body size and aerobic fitness Cardiovascular Responses: Heart Rate (HR) • Normal ranges – Untrained RHR: 60 to 80 beats/min – Trained RHR: as low as 30 to 40 beats/min – Affected by neural tone, temperature, altitude • Anticipatory response: HR above RHR just before start of exercise – Vagal tone – Norepinephrine, epinephrine Cardiovascular Responses: Heart Rate During Exercise • Directly proportional to exercise intensity • Maximum HR (HRmax): highest HR achieved in all-out effort to volitional fatigue – – – – Highly reproducible Declines slightly with age Estimated HRmax = 220 – age in years Better estimated HRmax = 208 – (0.7 x age in years) Cardiovascular Responses: Heart Rate During Exercise • Steady-state HR: point of plateau, optimal HR for meeting circulatory demands at a given submaximal intensity – If intensity , so does steady-state HR – Adjustment to new intensity takes 2 to 3 min • Steady-state HR basis for simple exercise tests that estimate aerobic fitness and HRmax Cardiovascular Responses: Stroke Volume (SV) • With intensity up to 40 to 60% VO2max – Beyond this, SV plateaus to exhaustion – Possible exception: elite endurance athletes • SV during maximal exercise ≈ double standing SV • But, SV during maximal exercise only slightly higher than supine SV – Supine SV much higher versus standing – Supine EDV > standing EDV Cardiovascular Responses: Factors That Increase Stroke Volume • Preload: end-diastolic ventricular stretch – Stretch (i.e., EDV) contraction strength – Frank-Starling mechanism • Contractility: inherent ventricle property – Norepinephrine or epinephrine contractility – Independent of EDV ( ejection fraction instead) • Afterload: aortic resistance (R) Cardiovascular Responses: Stroke Volume Changes During Exercise • Preload at lower intensities SV – Venous return EDV preload – Muscle and respiratory pumps, venous reserves • Increase in HR filling time slight in EDV SV • Contractility at higher intensities SV • Afterload via vasodilation SV Ventricular Contractility Cardiovascular Responses: Blood Pressure • During endurance exercise, mean arterial pressure (MAP) increases – Systolic BP proportional to exercise intensity – Diastolic BP slight or slight (at max exercise) • MAP = Q x total peripheral resistance (TPR) – Q , TPR slightly – Muscle vasodilation versus sympatholysis Cardiovascular Responses: Blood Flow Redistribution • Cardiac output available blood flow • Must redirect blood flow to areas with greatest metabolic need (exercising muscle) • Sympathetic vasoconstriction shunts blood away from less-active regions – Splanchnic circulation (liver, pancreas, GI) – Kidneys Cardiovascular Responses: Blood Flow Redistribution • Local vasodilation permits additional blood flow in exercising muscle – Local VD triggered by metabolic, endothelial products – Sympathetic vasoconstriction in muscle offset by sympatholysis – Local VD > neural VC • As temperature rises, skin VD also occurs – Sympathetic VC, sympathetic VD – Permits heat loss through skin Blood Flow Redistribution Cardiovascular Responses: Cardiovascular Drift • Associated with core temperature and dehydration • SV drifts – Skin blood flow – Plasma volume (sweating) – Venous return/preload • HR drifts to • Compensate • (Q maintained) Cardiovascular Responses: Fick** Principle • Calculation of tissue O2 consumption depends on blood flow, O2 extraction • VO2 = Q x (a-v)O2 difference • VO2 = HR x SV x (a-v)O2 difference • VO2max = Qmax [(a-v)O2 diffmax] **ExPhysRules (who IS Fick?) Cardiovascular Responses: Blood Oxygen Content • (a-v)O2 difference (mL O2/100 mL blood) – Arterial O2 content – mixed venous O2 content – Resting: ~6 mL O2/100 mL blood – Max exercise: ~16 to 17 mL O2/100 mL blood • Mixed venous O2 ≥4 mL O2/100 mL blood – Venous O2 from active muscle ~0 mL – Venous O2 from inactive tissue > active muscle – Increases mixed venous O2 content VO2max • The highest amount of oxygen a person can take in, transport and utilize to produce AP aerobically while breathing air during heavy exercise. – – – – Blood lactate value > 8-9mmol/L HR + 12bpm of predicted MHR (220-age) Respiratory exchange ratio of 1.0-1.1 A plateau in oxygen consumption during incremental exercise (rise < 2.1ml/kg/min in VO2 with an increase in workload that represents a change in grade of 2.5% while running at 7mph with 3 min stages). VO2max • • • • THE measure of aerobic fitness Laboratory assessment Performance-based concept Possible limitations of VO2max: – Ventilation – Blood flow – Metabolic functions • Lactic acid • pH • ATP availability Respiratory Responses: Ventilation During Exercise • Immediate in ventilation – Begins before muscle contractions – Anticipatory response from central command • Gradual second phase of in ventilation – Driven by chemical changes in arterial blood – CO2, H+ sensed by chemoreceptors – Right atrial stretch receptors Respiratory Responses: Ventilation During Exercise • Ventilation increase proportional to metabolic needs of muscle – At low-exercise intensity, only tidal volume – At high-exercise intensity, rate also • Ventilation recovery after exercise delayed – Recovery takes several minutes – May be regulated by blood pH, PCO2, temperature Figure 8.14 Respiratory Responses: Estimating Lactate Threshold • Ventilatory threshold as surrogate measure? – Excess lactic acid + sodium bicarbonate – Result: excess sodium lactate, H2O, CO2 – Lactic acid, CO2 accumulate simultaneously • Refined to better estimate lactate threshold – Anaerobic threshold – Monitor both VE/VO2, VE/VCO2 Ventilatory Equivalents During Exercise Respiratory Responses: Limitations to Performance • Ventilation normally not limiting factor – Respiratory muscles account for 10% of VO2, 15% of Q during heavy exercise – Respiratory muscles very fatigue resistant • Airway resistance and gas diffusion normally not limiting factors at sea level • Restrictive or obstructive respiratory disorders can be limiting Respiratory Responses: Limitations to Performance • Exception: elite endurance-trained athletes exercising at high intensities – Ventilation may be limiting – Ventilation-perfusion mismatch – Exercise-induced arterial hypoxemia (EIAH) Respiratory Responses: Acid-Base Balance • Metabolic processes produce H+ pH • H+ + buffer H-buffer • At rest, body slightly alkaline – 7.1 to 7.4 – Higher pH = Alkalosis • During exercise, body slightly acidic – 6.6 to 6.9 – Lower pH = Acidosis Respiratory Responses: Acid-Base Balance • Physiological mechanisms to control pH – Chemical buffers: bicarbonate, phosphates, proteins, hemoglobin – Ventilation helps H+ bind to bicarbonate – Kidneys remove H+ from buffers, excrete H+ • Active recovery facilitates pH recovery – Passive recovery: 60 to 120 min – Active recovery: 30 to 60 min Figure 8.16 Sex differences in CV responses • FFM • Blood volume & Heart Size • O2 carrying capacity