* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Cardiac Care in DMD The Heart is a Muscle Too
Survey
Document related concepts
Remote ischemic conditioning wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Rheumatic fever wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Electrocardiography wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Transcript
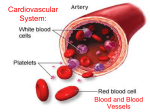
Cardiac Care in DMD The Heart is a Muscle Too Linda H. Cripe, M.D. Professor of Pediatrics Na7onwide Children’s Hospital The Ohio State University Columbus, Ohio USA 1. 2. 3. 4. 5. 6. 7. 8. What does “cardiomyopathy” mean? What does “heart failure mean”? Who should care for the heart? When should cardiac care begin? How will the heart be checked? What should I watch for? What treatment is available? Should carriers have their hearts checked? ………………..…………………………………………………………………………………………………………………………………….. What does cardiomyopathy mean? The normal heart ………………..…………………………………………………………………………………………………………………………………….. What does “cardiomyopathy” mean? Disease of heart muscle Normal Dilated 1) Muscle cell injury -‐ cell death 2) Chamber enlarges 3) Walls become thin 4) Scar forma7on or fibrosis 5) Func7on declines What does cardiomyopathy mean? DMD heart showing evidence of extensive fibrosis. Dystrophin is located inside the cell and is bound to actin at its N-terminus and to a large oligomeric complex of membrane glycoproteins at its C-terminus. Verhaert D et al. Circ Cardiovasc Imaging 2011;4:67-76 Copyright © American Heart Association What does “Heart Failure” mean? • Complicated • The heart fails to meet the demands of the body • Does NOT mean the heart has failed (stopped working)’ • Occurs when cardiac func7on is poor but can occur with good func7on and increased demand • Body’s response at first helpful but eventually causes harm PEOPLE LIVE WITH LONG LIVES WITH HEART FAILURE Who should care for the heart? • Cardiologist is a “heart doctor” • Pediatric cardiologists • Pediatrics and cardiology • Adult cardiologists • Adult medicine and cardiology • Some cardiologists have special interests • Heart failure/transplanta7on • Neuromuscular disorders • Talk to your sons doctor about finding an expert in trea7ng “heart failure” When should cardiac care start? Stage 1 2 Early Ambulatory Baseline visit, echo and ECG at diagnosis or by age 6 yrs Max interval 24 months between visits un7l the age of 10 yrs then yearly Pre-‐ symptoma0c 3 Late Ambulatory 4 Early Non-‐ ambulatory Yearly or more frequently dependent on symptoms and test results 5 Late Non-‐ ambulatory When should cardiac care begin? • Summary of Consensus Statements • Cardiac inves7ga7on should: • Begin at diagnosis (ideally) • Repeat inves7ga7on: • At least biannually un7l age 10 • Or with the onset of cardiac signs and symptoms • Annually aeer the age of 10 • Or more frequently based on cardiac signs and symptoms • Prior to any surgery (especially spine surgery) *****Minimum recommenda7ons ………………..…………………………………………………………………………………………………………………………………….. How will the heart be checked? 1. Electrocardiogram -‐(ECG) a. Heart Rate b. Heart Rhythm Electrocardiogram (ECG) Holter or Event Monitor ………………..…………………………………………………………………………………………………………………………………….. How will the heart be checked? 100 % Abnormal ECG • Electrocardiogram (ECG) • Abnormal at young age • Type of abnormality changes with age • No predictors of outcome found • Heart rate oeen elevated 10-‐15 bpm above “normal” • Changes over 7me important • Have copy of baseline ECG available 84 80 60 67 91 75 53 40 20 0 N = 105 ECGs 503 <5 5-10 10-15 15-20 20+ Age in years How will the heart be checked ? • Images of the heart will be ahained to evaluate structure and func7on How will the heart be checked? Two common ways to obtain images of the heart: Echocardiogram Cardiac MRI ………………..…………………………………………………………………………………………………………………………………….. How will the heart be checked? • Echocardiogram • Ultrasound evalua7on of heart • Evaluate anatomy and func7on • Contrac7on (systole) • Relaxa7on (diastole) • Advantages: • Readily available • Quick • Disadvantages: • Image quality unreliable • Scoliosis • Weight and posi7on • Not accurate for RV func7on How will the heart be checked? • Cardiac MRI • Advantages: • No radia7on exposure • Detailed cardiac informa7on • Accurate measurements • Addi7onal informa7on • Fibrosis • Metabolism • Disadvantages: • May involve IV placement • One hour in dura7on • Claustrophobic • Expensive • Seda7on (younger children) CMR findings in DMD in patients with different degrees of cardiac involvement. Verhaert D et al. Circ Cardiovasc Imaging 2011;4:67-76 Copyright © American Heart Association What signs and symptoms should I watch for? • Know your sons baseline • Learn to take his pulse • At rest • While busy • Sleeping • Buy a stethoscope • Develop a rela7onship with your care provider before you need them What should I watch for? • Rapid weight gain (or loss) • Swelling of feet or overall puffiness • Heart racing/skipping beats or fain7ng (syncope) • Learn to take your son’s pulse • Buy a stethoscope • Chest pain (common) • Usually musculoskeletal v BUT …….if severe seek medical help What treatment is available? Currently, standard heart failure treatment • – Informa7on taken from adult HF experience Treatment not based • • • Not based on pediatric data Not dystrophin specific Goals: • • • • Improve survival Slow disease progression Alleviate symptoms ………………..…………………………………………………………………………………………………………………………………….. What treatment is available? • Heart failure drugs • ACE inhibitors • enalapril, lisinopril, perindopril • Angiotensin-‐ receptor blockers • Losartan • β-‐blockers • metoprolol, carvedilol • Diure7cs • furosemide, thiazides – Aldosterone receptor antagonists • spironolactone • An7-‐coagula7on • Coumadin, Aspirin ………………..…………………………………………………………………………………………………………………………………….. NEJM 2003 What treatment is available? Best evidence: All e7ologies of cardiomyopathy with abnormal func7on, regardless of symptoms should be treated with ACE inhibitors (Evidence Class IA) with considera7on for β-‐ blockers if progression – Delays heart failure – Reduces symptoms, if present – Improves prognosis No reason this established HF prac7ce should not be applied to DMD/BMD ACC/AHA HF Guidelines Circula7on 2005 ………………..…………………………………………………………………………………………………………………………………….. Does steroid treatment benefit the heart? ………………..…………………………………………………………………………………………………………………………………….. Steroid Treatment ………………..…………………………………………………………………………………………………………………………………….. What treatment is available? • Always an individualized risk/benefit analysis • Benefits: • Abnormal func7on (+/-‐ symptoms) • well established • Normal func7on – unclear • Role for research to answer: when, what agent, what dose, how long? • Risks: • All drugs have side effects • Drugs untested in pa7ents with DMD ………………..…………………………………………………………………………………………………………………………………….. What treatment is available? • Pacemakers • Cardiac re-‐synchroniza7on therapy • Successful in adult heart failure popula7on • Preliminary data suggest DMD popula7on may not be good candidates What treatment is available? • Ventricular Assist Devices • Cutng edge technology • Many devices currently under development • Possible benefit for sub-‐ popula7on of DMD/BMD pa7ents • Useful as: • Bridge to transplanta7on • Des7na7on therapy What treatment is available? • Cardiac Transplanta7on • Few DMD pa7ents transplanted • More BMD pa7ents transplanted • Problems • Limited donor availability • Trading one disease for another • Quality of life issues • • Should carriers have their hearts checked? • Oeen cardiac disease only manifesta7on • Cardiomyopathy risk increases with age • Approximately 350 DMD/BMD carriers • age < 16 yrs: all normal • age 16-‐30 yrs: 6%; 31-‐50 yrs: 9%; > 50 yrs: 16% DCM • Baseline evalua7on as young adult • Frequency unclear (? every 5 years) • Be aware of symptoms • Take care of yourself • minimize other CV risks • smoking, HTN, cholesterol NMD 1999, 2003; Lancet 1999; JAMA 1996 ………………..…………………………………………………………………………………………………………………………………….. Conclusions • Cardiac evalua7on should begin at diagnosis Conclusions • Ongoing cardiac follow-‐up is important and the best way to insure long term cardiac health Conclusions • When there is evidence of abnormal func7on treatment is recommended Conclusions • Early treatment prior to onset of dysfunc7on is unproven and controversial – Important to consider risks and benefits Conclusions • Need to use common sense AT ALL TIMES Conclusions • Maintain an open dialog with all care providers – They are working FOR YOU Conclusions YOU AND YOUR FAMILY are the most important members of the health care team THANK YOU