* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Guidelines for the Diagnosis and Management of
Remote ischemic conditioning wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiac surgery wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
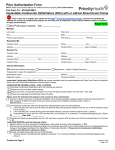
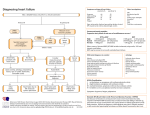
Guidelines for the Diagnosis and Management of Heart Failure 7/1/14 This guideline has been developed to assist clinicians and staff in providing evidence-based therapy for patients presenting with signs and symptoms of systolic or diastolic heart failure, excluding isolated cor pulmonale, who do not require hospitalization in the intensive care unit. This guideline is not meant to substitute for clinical judgment and may not meet the needs of each individual patient. This guideline is intended for use for patients 18 years of age and older only. American College of Cardiology Foundation/American Heart Association (ACCF/AHA) Guidelines The recommendations in this CPM are derived from the ACCF/AHA Guidelines Executive Summary: Guidelines for the Management of Heart Failure, published in 2013. Basic principles of management of Heart Failure: Key References: •Recognition of the condition and precipitating factors •Classification by type of Heart Failure, severity of symptoms and clinical stage •Guideline Directed Medical Therapy (GDMT) •Patient engagement and education •Discharge planning •Follow-up care •Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJV, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WHW, Tsai EJ, Wilkoff BL. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;62:e147–239. •Guideline for the Management of Patients With Atrial Fibrillation: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J AM Coll Cardiol. 2014;doi:10.1016/j.jacc.2014.03.021 •Intermountain Health Care CPMs Recognize common factors that precipitate HF requiring hospitalization and during hospitalization and treat promptly (I,C) • Non-adherence to medication regimen, sodium and/or fluid restriction •Acute myocardial ischemia •Uncorrected high blood pressure •AF and other arrhythmias •Recent addition of negative inotropic drugs (e.g., steroids, thiazolidinediones, NSAIDs) •Pulmonary Embolus •Initiation of drugs that increase salt retention (e.g., steroids, thiazolidinediones, NSAIDs) •Excessive alcohol or illicit drug use •Endocrine abnormalities (e.g., diabetes mellitus, hyperthyroidism, hypothyroidism) •Concurrent infections (e.g., pneumonia, viral illnesses) •Additional acute cardiovascular disorders (e.g., valve disease endocarditis, myopericarditis, aortic dissection Key to Classification of Recommendation & Level of Evidence Class I Benefit>>>Risk Should be done Class IIa Benefit>>Risk Reasonable to do Level A Multiple populations Multiple RCTs or meta-analyses Level B Limited populations Single RCT or nonrandomized studies The inside pages of this tool provide an algorithm and associated quick reference tables, and can be posted in your office or clinic. The medications referenced include Flagstaff Medical Center and IHS formulary. Final Version 11.2014 Class IIb Benefit≥Risk May be considered Level C Very limited populations Only consensus, case studies, or standard of care Class III Risk≥Benefit or No Benefit Do not do 1 Guidelines for the Diagnosis and Management of Heart Failure 7/1/14 Tip Box Suspect Diagnosis of HF Echo I,C/BNP I,A Heart Failure Confirmed If isolated Cor Pulmonale, refer to Cor Pulmonale CPM Consider Cardiology Consult for all HF patients Mandatory Cardiology Consult: •Newly diagnosed HF •When prescribing spironolactone •Ischemic Evaluation •Consideration for device therapy •Consideration of changes to anti-arrhythmics or requiring two diuretics Labs , EKG, CXR review (class I,A) If suspected ischemic disease: •Cardiology consult •Consider cardiac cath if angina present (IIa,C) or no known CAD (IIa,C) •Non-invasive cardiac imaging if h/o CAD and angina absent unless not eligible for cath/stent or CABG in which case NO imaging (IIa,C) Indicate cause of HF , if known (valvular, ischemic, non-ischemic) Classify Type of HF a •Known heart failure with acute exacerbation •New signs or symptoms of heart failure including: dyspnea, fatigue, exercise intolerance, weight gain, pulmonary edema, orthopnea, peripheral edema, elevated BNP, hyponatremia with volume overload Tip Box In ambulatory patients with dyspnea, measurement of BNP or N-terminal pro-B-type natriuretic peptide (NT-proBNP) is useful to support clinical decision making regarding the diagnosis of HF, especially in the setting of clinical uncertainty. (I,A) *ECHO indicated for initial evaluation of pts presenting with HF, pts who have had significant change in clinical status, pts who have received treatment that might affect cardiac function or for consideration of device therapy. (I,C) Repeat ECHO in the absence of clinical status change or treatment interventions should NOT be performed (III,B) Tip Box Labs: fasting lipids (only if new onset HF), CBC,CMET, Troponin, Mg, U/A, TSH (all are class I,A) Table b Table a ACCF/AHA Stages of HF (37) Classification Systolic heart failure, specify acute/chronic I. Heart failure with reduced ejection ≤40 fraction (HFrEF) Also referred to as systolic HF. Randomized controlled trials have mainly enrolled patients with HFrEF, and it is only in these patients that efficacious therapies have been demonstrated to date A At high risk for HF but without structural heart disease or symptoms of HF None Diastolic Heart Failure, specify acute/chronic II. Heart failure with preserved ejection fraction (HFpEF) Also referred to as diastolic HF. Several different criteria have been used to further define HFpEF. The diagnosis of HFpEF is challenging because it is largely one of excluding other potential noncardiac causes of symptoms suggestive of HF. To date, efficacious therapies have not been identified. B Structural heart disease but without signs or symptoms of HF I No limitation of physical activity. Ordinary physical activity does not cause symptoms of HF. These patients fall into a borderline or intermediate group. Their characteristics, treatment patterns, and outcomes appear similar to those of patients with HFpEF. C Structural heart disease with prior or current symptoms of HF I No limitation of physical activity. Ordinary physical activity does not cause symptoms of HF. II Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in symptoms of HF. III Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity causes symptoms of HF. IV Unable to carry on any physical activity without symptoms of HF, or symptoms of HF at rest. Diastolic heart failure combined a. HFpEF, with systolic heart failure, borderline specify acute/chronic No ICD-10 dx, consider systolic heart failure, chronic/improved, +/- acute exacerbation b. HFpEF, improved EF (%) ≥50 41 to 49 >40 Description It has been recognized that a subset of patients with HFpEF previously had HFrEF. These patients with improvement or recovery in EF may be clinically distinct from those with persistently preserved or reduced EF. Further research is needed to better characterize these patients. Classify HF based on stage and NYHA symptom severity b Obtain prior Dry Weight (I,A) Management NYHA Functional Classification (38) ICD 10 diagnoses Justification of classification: Correct recognition of the type of heart failure (preserved EF vs. reduced EF rEF) allows appropriate tailoring of guidelinedirected medical therapy and, as a result, better clinical outcomes with the potential for reduced morbidity and mortality and improved HRQOL D Refractory HF requiring specialized interventions Final Version 11.2014 TIP: Dry Weight can be obtained from patient, PCP, Cardiologist, Dialysis unit, or on Health Summary for all IHS pt’s. **Use recent lowest value** 2 Guidelines for the Diagnosis and Management of Heart Failure 7/1/14 Management STAGE A e.g., Patients with: •HTN •Atherosclerotic disease •DM •Obesity •Metabolic Syndrome Or Patients •Cardiotoxins (meth) •with family h/o cardiomyopathy THERAPY Drugs •ACEi or ARB in appropriate patients for vascular disease/HTN or DM •Statins as indicated(I,A for h/o MI) •Control conditions that contribute to development of HF (DM2, HTN, obesity, smoking, cardiotoxin exposure) (I,A-C) STAGE C STAGE B At high risk for HF but w/o structural heart disease or symptoms of HF e.g., Patients with: •Previous MI •LV remodeling including LVH and Low EF •Asymptomatic valvular disease THERAPY Drugs •ACEi for all reduced EF, ARB if ACEi intolerant (I,A) •ACEi or ARB for all patients with MI+ reduced EF (I,A) •evidence-based beta blockers for low EF+/- h/o MI (I,A) •Avoid verapamil & diltiazem after MI or low EF (III,C) •Statin if CAD or hyperlipidemia Selected Patients: CRTg ICD h STAGE D Structural heart disease w/prior or current symptoms of HF Structural heart disease w/o signs or symptoms of HF Structural Heart Dz Symptomatic Heart Failure New sxs of HF e.g., Patients with: •Known structural heart disease and •HF signs and symptoms Refractory HF Refractory symptoms of HF at rest, despite GDMT Treatment for ALL Stage C and D pts: •Dry weight teaching (I,B) •Continue outpatient medications unless •Exercise training or regular physical new contraindication identified(I,B) activity • Low Sodium Diet (IIa,C) •Cardiac rehab referral inpatient (IIa,B) •Daily weights (I,C) •Aggressive Care Coordination (IIa,B) HFpEF HFrEF diastolic systolic THERAPY Strategies •Identification of comorbidities •Control sbp and dbp(I,B) •Coronary intervention if indicated (IIa,C) •Guideline-directed care for Afib (IIa,C) Treatment •Diuresis as needed (I,C) •Use beta blockers, ACEi or ARBs to control BP •ARB may decrease hospitalizations(IIb,B) •Omega 3 fatty acids if NYHA II-III and no ESLD, eGFR>30, no chronic lung dz, no PAD (IIa,B) e.g., Patients with: •Marked HF symptoms at rest •Recurrent hospitalizations despite GDMT •HF specific educational Components •Appropriate treatment for OSA •Statins if ischemic HF or other indication THERAPY Drugs for all patients •DC all potentially harmful medications including all NSAIDS, thiazolidinediones,most anti-arrhythmics (cards c/s required prior to cessation),calcium channel blockers (III harm, B/C) except amlodipine •Diuretics for fluid retention (I,B) f •ACEi or ARB if ACEi intolerant(I,A) f •Evidence-based Beta Blockers if stable (carvedilol, metoprolol succinate (I,A) f Drugs used for selected patients •Aldosterone antagonists* (Spironolactone) both THERAPY Goals Fluid restriction 1.5L/day esp if hyponatremic (IIa,C) •Control symptoms •Improve HRQOL* •Reduce hospital readmissions •Establish patient's end of life goals (I,B) Options for select pts •Advanced care measures •Heart transplant •Chronic inotropes(IIb,B) •Temporary or permanent MCS(IIa,B) •Experimental surgery or drugs •Palliative care/hospice (I,B) •ICD deactivation •Isosorbide dinitrate+hydral(NYHA III-IV, AfricanAm w/persistent sxs in spite of ACEi &beta blocker)(I,A) •Isosorbide dinitrate+hydral for any pt who cannot get ACEi *Aldosterone receptor antagonist or ARB (IIa,B) (spironolactone) is recommended in pt’s •Digoxin (can reduce hospitalizations)(IIa,B) with NYHA class II-IV HF with LVEF of •Omega 3 fatty acid (same caveats as for HFpEF) 35% or less, unless contraindicated, to •Add ARB to ACEI if persistent symptoms (non-African reduce morbidity and mortality, American) if no aldosterone antagonist is indicated. (IIb,A) provided estimated GFR>30mL/min and **Do NOT use ACE-I +ARB +aldo antagonist (III:Harm, B) K+<5.0 mEq/dl (I,A) •Add IV NTG, nitroprusside or nesiritide if dyspnea persists Also indicated for post acute MI w/ (IIb,A) EF≤40% w/DM or symptoms of HF (I,B) Treatment In Selected patients CRTg Final Version 11.2014 3 ICD h *HRQOL, health-related quality of life Revascularization or valvular surgery as appropriate Table f Drug Recommendations: **NOT on most IHS Formularies: Captopril,Valsartan, Isosorbide mononitrate, Metoprolol succinate** Medication choices Start Dose Clinical Trial Dose Max ACE INHIBITORS (ACE-I) lisinopril (Prinivil, Zestril): **captopril (Capoten): 2.5-5mg PO daily 6.25mg PO TID 32mg 40mg/dose 40mg PO daily or divided BID 50mg PO TID Labs and other notes Obtain BMP to check K+ and creatinine. If K+ >5.0, decrease or discontinue K+ supplementation, aldosterone antagonists, or modify target dose of ACE-I. **Captopril NOT on most IHS Formularies** Use ACE-I with caution in patients with renal impairment (creatinine >3.0). † Not FDA-approved for heart failure. ARBs (if ACE-I intolerant) losartan (Cozaar)† 25-50mg PO daily 129mg/day 150mg/day At FMC, valsartan only available for high dose therapy, >320mg **valsartan (Diovan): 20-40mg PO BID 127mg/dose 160mg PO BID **Valsartan NOT on most IHS Formularies** Combination isosorbide dinitrate and hydralazine is recommended for African Americans with persistent symptoms on ACE-I and beta blocker therapy. If ACE-I and ARB intolerant use COMBINATION isosorbide and hydralazine isosorbide dinitrate (Isordil, Sorbitrate): 20-30mg PO TID or QID 30mg PO TID or 22.5mg PO QID 40mg PO TID 30mg PO QID hydralazine HCl (Apresoline) 25-50mg PO TID or QID 58mg PO TID or 44mg PO QID 300mg/day isosorbide mononitrate (Imdur): 30mg PO daily 240mg/day BETA BLOCKERS carvedilol (Coreg): 3.125mg PO BID 18.5mg PO BID 50mg PO BID **metoprolol succinate (Toprol XL) 12.5-25mg PO daily 159mg/day 200mg/day This combination is preferred for control of BP, over non-dihydropyridine CCBs **isosorbide mononitrate NOT on most IHS Formularies** Before starting or titrating beta blockers, ensure patient is euvolemic (with HR >55 bpm and systolic BP >90) and off vasodilators and inotropes. Use caution if pt has required inotropes this hospitalization (I,b) Educate about initial side effects (fatigue, hypervolemia) **Metoprolol succinate NOT on most IHS Formularies** Use caution to avoid dig toxicity with following meds: Thiazides, Spironolactone, Metolazone, Loop Diuretics (less serious), Metoprolol (brady), Amiodarone DIGOXIN digoxin (Lanoxin): 0.125mg PO daily ALDOSTERONE ANTAGONISTS (requires cardiology consult & labs 72hrs after starting therapy) spironolactone (Aldactone): Combination also indicated for all patients for whom ACEI/ARB/Aldosterone antagonist are contraindicated. 12.5-25mg daily 26mg/day 25mg daily or BID Consider Reducing/stopping potassium supplements. Monitor serum K+ 3 days after starting therapy, at 1 week, then monthly for the first 3 months, and with changes in renal function eGFR ≥50, K ≤5:start 12.5-25mg/day, max 25mg/day or BID after 4 wks if K ≤5 eFGR 30-49: K ≤5: start 12.5mg daily or QOD, max 12.5-25mg daily after 4 wks if K ≤5 eGFR <30: do not use Diuretics (IV) Initial Dose oral Maximum Dose give metolazone 30min prior to IV lasix, cardiology c/s required Furosemide Bumetanide Metolazone 20-80mg IV Q8 or 2.5-10mg/hr 0.5-1mg IV daily 20-40mg daily or BID 0.5-1mg daily or BID 2.5-10mg daily w/loop 600mg/24hrs 10mg/24hrs n/a Hydrochlorothiazide (oral) Chlorothiazide (IV) 25-50mg once or twice + loop 500-1000mg once + loop diuretic use IV loop diuretics at or above usual outpatient dose (I,B) . No difference in efficacy between divided doses vs drip. (I,B) Daily BMET, Mg, weights, assessment of volume status. Inadequate response to diuresis: consult cardiology for addition of 2nd diuretic vs higher doses. (IIa,B for increasing dose or adding a second diuretic) Q12-24hrs Q24hrs Final Version 11.2014 4 Guidelines for the Diagnosis and Management of Heart Failure 7/1/14 Indications for Cardiac Resynchronization Therapy (CRT) Indications for ICD (Implantable Cardioverter-Defibrillator)(I,A) for PRIMARY prevention of sudden cardiac death (see separate recs for history of VT/Vfib which are NOT covered here) Patient with cardiomyopathy on GDMT for ≥40d post MI or with implantation of pacing or defibrillation Table h All ICD patients should have > 1year life expectancy device for special indications Table g If LVEF ≤35%, evaluate non-cardiac health If comorbidities and/or frailty DO NOT limit survival with good functional capacity to <1 year: EVALUATE NYHA class and refer to table below. If comorbidities/frailty limit survival to <1 yr, cont GDMT alone NYHA Class I NYHA Class II Special CRT Indications LVEF≤35% QRS≥150ms LBBB pattern Sinus rhythm NYHA Class III & Ambulatory Class IV LVEF≤35% QRS≥150ms LBBB pattern Sinus rhythm LVEF≤30% QRS≥150ms LBBB pattern Ischemic CM Sinus rhythm QRS≤150ms Non-LBBB pattern LVEF≤35% QRS 120-149ms LBBB pattern Sinus rhythm LVEF≤35% QRS 120-149ms LBBB pattern Sinus rhythm Atrial fibrillation, if ventricular pacing is required and rate control will result in near 100% V pacing with CRT LVEF≤35% QRS≥150ms Non-LBBB pattern Sinus rhythm QRS≤150ms Non-LBBB pattern LVEF≤35% QRS≥150ms Non-LBBB pattern Sinus rhythm LVEF≤35% QRS 120-149ms Non-LBBB pattern Sinus rhythm EF NYHA Ischemic (at least 90d post revascularization (PCI or CABG)) <30% I-III Indicated if on GDMT at least 40d post MI (IIa,B) <35% II-III Indicated if on GDMT at least 40d post MI (I,A) Nonischemic Indicated if on GDMT at least 90 days (I,A) Anticipated to require frequent ventricular pacing (>40%) If patient meets criteria for ICD or CRT Class I-IIb, consult Electrophysiologist Color Evidence Class I IIa IIb III If patient needs Pacemaker for non-HF indication, consult Electrophysiologist for evaluation for possible CRT Recommendation Should be done Reasonable to do May be considered Do not do Final Version 11.2014 5 Guidelines for the Diagnosis and Management of Heart Failure 7/1/14 TIP: Control of Afib in patients with HF (This algorithm does NOT apply to patients in Afib without evidence of heart failure) •Prevalence of atrial fibrillation in patients with HF by NYHA class: Class I: 4% Class IV 40% •Afib is present in 30% of patients presenting with acute HF ~AF causes HF and HF causes AF~ Heart Failure with Atrial Fibrillation* Anti-coagulation for AFib/Flutter Rhythm control Rate Control *if the HF is new, assume it is a rate-related cardiomyopathy. Rate related cardiomyopathies can recover with adequate treatment • • • • • • Amiodarone + anticoagulation with plans for future cardioversion FAILED, rhythm or rate control Try opposite method; rhythm or rate Select anti-thrombotic based on risk of thromboembolism regardless of Afib pattern (paroxysmal, persistent or permanent) (I,B) Indications for anti-coagulation of Aflutter are the same as for Afib(I,C) For non-valvular Afib, CHA2DS2-VASc is recommended to assess stroke risk (I,B) For Afib with mechanical heart valve, use warfarin (I,B) For pts with non-valvular AF & prior CVA/TIA or CHA2DS2-VASc≥2, use oral anticoagulant (I,B) Consider anticoagulation for patients with chronic HF who have Afib and NO additional cardioembolic risk factors. (IIa,B) Treatment suggestions HFpEF Diastolic •Beta blocker or verapamil or diltiazem •+/- digoxin as adjunct HFrEF Systolic •Beta blocker +/- digoxin (transition to evidence-based beta blocker when transition to oral) compensated FAILED both Decompensated •Cardioversion •Amiodarone can be useful to enhance the efficacy of cardioversion •Start Heparin concurrently if AF of >48hrs duration AV node ablation and CRT Dronedarone should not be administered to patients with class IV heart failure or patients who have had an episode of decompensated heart failure in the past 4 weeks, especially if they have depressed left ventricular function (left ventricular ejection fraction < 35%). (III harm, B) Final Version 11.2014 6 Guidelines for the Diagnosis and Management of Heart Failure 7/1/14 Interdisciplinary team: •Dietician •Cardiac Rehab Team, •Care Coordination •Outpatient Care Managers •Pharmacy • RT • Primary care RN Discharge Checklist Readiness for DC: RED •Identify patient •CPM enrollment •BOOST assessment (risk prediction) •Begin DC Checklist Yellow •Transitional Care Plan •Assistance with practical needs •BH integration •Care Processes, structured •Support for life instabilities Green •DC Checklist complete •Meds in Hand •DC HF Education and Patient Activation •Sodium restricted diet •Fluid restriction (if indicated) •Monitoring of daily weights •What to do if HF symptoms worsen/whom to call •Physical activity level counseling (next phase of Cardiac rehab/exercise plan) •Treatment and adherence education •Smoking cessation counseling if indicated •Weight reduction counseling if indicated •Review of Medications HF education needs to be specific to facilitate self care with at least 60minutes by trained HF educator Discharge Checklist must be complete before patient is considered for hospital discharge. Final Version 11.2014 7 Final Version 11.2014 8










![[ Insert Title Here ]](http://s1.studyres.com/store/data/008479268_1-03ff748536c27aeae665c17a72e89ec4-150x150.png)