* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Chapter 20 - ltcconline.net
Human microbiota wikipedia , lookup
Neonatal infection wikipedia , lookup
Urinary tract infection wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Schistosomiasis wikipedia , lookup
Triclocarban wikipedia , lookup
Anaerobic infection wikipedia , lookup
Globalization and disease wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Germ theory of disease wikipedia , lookup
Yersinia pestis wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
Typhoid fever wikipedia , lookup
Gastroenteritis wikipedia , lookup
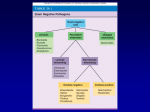
Lecture PowerPoint to accompany Foundations in Microbiology Seventh Edition Talaro Chapter 20 The Gram-Negative Bacilli of Medical Importance Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. 20.1 Aerobic Gram-Negative Nonenteric Bacilli • Large, diverse group of non-spore-forming bacteria • Wide range of habitats – large intestines (enteric), zoonotic, respiratory, soil, water • Most are not medically important; some are true pathogens, some are opportunists • All have a lipopolysaccharide outer membrane of cell wall – endotoxin 2 3 Aerobic Gram-Negative Nonenteric Bacilli • Pseudomonas and Burkholderia – an opportunistic pathogen • Brucella and Francisella – zoonotic pathogens • Bordetella and Legionella – mainly human pathogens 4 Pseudomonas: The Pseudomonads • Small gram-negative rods with a single polar flagellum • Free living – Primarily in soil, sea water, and fresh water; also colonize plants and animals • • • • • Important decomposers and bioremediators Frequent contaminants in homes and clinical settings Use aerobic respiration; do not ferment carbohydrates Produce oxidase and catalase Many produce water soluble pigments 5 Figure 20.1 Pseudomonas aeruginosa 6 Pseudomonas Aeruginosa • Common inhabitant of soil and water • Intestinal resident in 10% normal people • Resistant to soaps, dyes, quaternary ammonium disinfectants, drugs, drying • Frequent contaminant of ventilators, IV solutions, anesthesia equipment • Opportunistic pathogen 7 Figure 20.2 Skin rash from Pseudomonas 8 Pseudomonas Aeruginosa • Common cause of nosocomial infections in hosts with burns, neoplastic disease, cystic fibrosis • Complications include pneumonia, UTI, abscesses, otitis, and corneal disease • Endocarditis, meningitis, bronchopneumonia • Grapelike odor • Greenish-blue pigment (pyocyanin) • Multidrug resistant • Cephalosporins, aminoglycosides, carbenicillin, polymixin, quinolones, and monobactams 9 Figure 20.3 Pseudomonas (left) and Staphylococcus (right) 10 20.2 Related Gram-Negative Aerobic Rods • Genera Burkholderia, Acinetobacter, Stenotrophomonas • Similar to pseudomonads • Wide variety of habitats in soil, water, and related environments • Obligate aerobes; do not ferment sugars • Motile, oxidase positive • Opportunistic 11 Burkholderia • Burkholderia cepacia – active in biodegradation of a variety of substances; opportunistic agent in respiratory tract, urinary tract, and occasionally skin infections; drug resistant • B. pseudomallei – generally acquired through penetrating injury or inhalation from environmental reservoir; wound infections, bronchitis and pneumonia, septicemia 12 Acinetobacter and Stenotrophomonas • Acinetobacter baumanii – nosocomial and community acquired infections; wounds, lungs, urinary tract, burns, blood; extremely resistant – treatment with combination antimicrobials • Stenotrophomonas maltophilia – forms biofilms; contaminant of disinfectants dialysis equipment, respiratory equipment, water dispensers, and catheters; clinical isolate in respiratory soft tissue, blood, CSF; high resistance to multidrugs 13 Brucella and Brucellosis • Tiny gram-negative coccobacilli • 2 species: – Brucella abortus (cattle) – Brucella suis (pigs) • Brucellosis, malta fever, undulant fever, and Bang disease – a zoonosis transmitted to humans from infected animals • Fluctuating pattern of fever – weeks to a year • Combination of tetracycline and rifampin or streptomycin • Animal vaccine available • Potential bioweapon 14 Figure 20.5 Agglutination titer test for brucellosis 15 Francisella Tularensis and Tularemia • Causes tularemia, a zoonotic disease of mammals endemic to the northern hemisphere, particularly rabbits • Transmitted by contact with infected animals, water and dust or bites by vectors • Headache, backache, fever, chills, malaise, and weakness • 10% death rate in systemic and pulmonic forms • Intracellular persistence can lead to relapse • Gentamicin or tetracycline • Attenuated vaccine • Potential bioterrorism agent 16 Bordetella Pertussis • Minute, encapsulated coccobacillus • Causes pertussis or whooping cough, a communicable childhood affliction • Acute respiratory syndrome • Often severe, life-threatening complications in babies • Reservoir – apparently healthy carriers • Transmission by direct contact or inhalation of aerosols 17 Bordetella Pertussis • Virulence factors – Receptors that recognize and bind to ciliated respiratory epithelial cells – Toxins that destroy and dislodge ciliated cells • Loss of ciliary mechanism leads to buildup of mucus and blockage of the airways • Vaccine – DTaP – acellular vaccine contains toxoid and other Ags 18 Figure 20.7 Prevalence of pertussis in the United States 19 Alcaligenes • Live primarily in soil and water • May become normal flora • A. faecalis – most common clinical species – Isolated from feces, sputum, and urine – Occasionally associated with opportunistic infections – pneumonia, septicemia, and meningitis 20 Legionella Pneumophila and Legionellosis • Widely distributed in water • Live in close association with amoebas • 1976 epidemic of pneumonia afflicted 200 American Legion members attending a convention in Philadelphia and killed 29 • Legionnaires disease and Pontiac fever • Prevalent in males over 50 • Nosocomial disease in elderly patients • Fever, cough, diarrhea, abdominal pain, pneumonia fatality rate of 3-30% • Azithromycin 21 Figure 20.8 Appearance of Legionella pneumophila 22 20.3 Enterobacteriaceae Family • Enterics • Large family of small, non-spore-forming gram-negative rods • Many members inhabit soil, water, decaying matter, and are common occupants of large bowel of animals including humans • Most frequent cause of diarrhea through enterotoxins • Enterics, along with Pseudomonas sp., account for almost 50% of nosocomial infections 23 Figure 20.9 Bacteria that account for the majority of hospital infections 24 • Facultative anaerobes, grow best in air • All ferment glucose, reduce nitrates to nitrites, oxidase negative, and catalase positive • Divided into coliforms (lactose fermenters) and non-coliforms (non-lactose fermenters) • Enrichment, selective and differential media utilized for screening samples for pathogens 25 Figure 20.10 Biochemical traits for separating enteric genera 26 Figure 20.11 Isolation media for enterics 27 Figure 20.12 BBL Enterotube II, rapid biochemical testing of enterics 28 Antigenic Structures and Virulence Factors Complex surface antigens contribute to pathogenicity and trigger immune response: • H – flagellar Ag • K – capsule and/or fimbrial Ag • O – somatic or cell wall Ag – all have • Endotoxin • Exotoxins 29 Figure 20.13 Antigenic structures in gram-negative enteric rods 30 20.4 Coliform Organisms and Diseases 31 Escherichia Coli: The Most Prevalent Enteric Bacillus • Most common aerobic and non-fastidious bacterium in gut • 150 strains • Some have developed virulence through plasmid transfer, others are opportunists 32 Pathogenic Strains of E. Coli • Enterotoxigenic E. coli causes severe diarrhea due to heat-labile toxin and heat-stable toxin – stimulate secretion and fluid loss; also has fimbriae • Enteroinvasive E. coli causes inflammatory disease of the large intestine • Enteropathogenic E. coli linked to wasting form infantile diarrhea • Enterohemorrhagic E. coli, O157:H7 strain, causes hemorrhagic syndrome and kidney damage 33 Escherichia coli • Pathogenic strains frequent agents of infantile diarrhea – greatest cause of mortality among babies • Causes ~70% of traveler’s diarrhea • Causes 50-80% UTI • Coliform count – indicator of fecal contamination in water 34 Figure 20.14 Rapid identification of E. coli O157:H7 35 Other Coliforms Clinically important mainly as opportunists • Klebsiella pneumoniae – normal inhabitant of respiratory tract, has large capsule, cause of nosocomial pneumonia, meningitis, bacteremia, wound infections, and UTIs • Enterobacter sp. – UTIs, surgical wounds • Citrobacter sp. – opportunistic UTIs and bacteremia • Serratia marcescens – produces a red pigment; causes pneumonia, burn and wound infections, septicemia and meningitis 36 Figure 20.15 A capsule stain of Klebsiella pneumoniae 37 Figure 20.16 Serratia marcescens 38 20.5 Noncoliform Lactose-Negative Enterics • Proteus, Morganella, Providencia • Salmonella and Shigella 39 Opportunists: Proteus and Its Relatives Proteus, Morganella, Providencia – ordinarily harmless saprobes in soil, manure, sewage, polluted water, commensals of humans and animals – Proteus sp. – swarm on surface of moist agar in a concentric pattern – Involved in UTI, wound infections, pneumonia, septicemia, and infant diarrhea – Morganella morganii and Providencia sp. involved in similar infections • All demonstrate resistance to several antimicrobials 40 Figure 20.17 Wavelike, swarming pattern of Proteus vulgaris 41 Salmonella and Shigella • Well-developed virulence factors, primary pathogens, not normal human flora • Salmonelloses and Shigelloses – Some gastrointestinal involvement and diarrhea but often affect other systems 42 Typhoid Fever and Other Salmonelloses • Salmonella typhi – most serious pathogen of the genus; cause of typhoid fever; human host • S. cholerae-suis – zoonosis of swine • S. enteritidis – includes 1,700 different serotypes based on variation on O, H, and Vi • Flagellated; survive outside the host • Resistant to chemicals – bile and dyes 43 Typhoid Fever • Bacillus enters with ingestion of fecally contaminated food or water; occasionally spread by close personal contact; ID 1,000-10,000 cells • Asymptomatic carriers; some chronic carriers shed bacilli from gallbladder • Bacilli adhere to small intestine, cause invasive diarrhea that leads to septicemia • Treat chronic infections with chloramphenicol or sulfatrimethoprim • 2 vaccines for temporary protection 44 Figure 20.18 Prevalence of salmonelloses 45 Figure 20.19 The phases of typhoid fever 46 Animal Salmonelloses • Salmonelloses other than typhoid fever are called enteric fevers, Salmonella food poisoning, and gastroenteritis • Usually less severe than typhoid fever but more prevalent • Caused by one of many serotypes of Salmonella enteritidis; all zoonotic in origin but humans can become carriers – Cattle, poultry, rodents, reptiles, animal, and dairy products – Fomites contaminated with animal intestinal flora 47 Shigella and Bacillary Dysentery • • • • Shigellosis – incapacitating dysentery S. dysenteriae, S. sonnei, S. flexneri, and S. boydii Human parasites Invades villus of large intestine, does not perforate intestine or invade blood • Enters Peyer’s patches instigate inflammatory response; endotoxin and exotoxins • Treatment – fluid replacement and ciprofloxacin and sulfatrimethoprim 48 Figure 20.20 The appearance of the large intestinal mucosa in Shigella 49 The Enteric Yersinia Pathogens • Yersinia enterocolitica – domestic and wild animals, fish, fruits, vegetables, and water – Bacteria enter small intestinal mucosa, some enter lymphatic and survive in phagocytes; inflammation of ileum can mimic appendicitis • Y. pseudotuberculosis – infection similar to Y. enterocolitica, more lymph node inflammation 50 Nonenteric Yersinia Pestis and Plague • Nonenteric • Tiny, gram-negative rod, unusual bipolar staining and capsules • Virulence factors – capsular and envelope proteins protect against phagocytosis and foster intracellular growth – Coagulase, endotoxin, murine toxin 51 Figure 20.21 Gram-stain of Yersinia pestis 52 Yersinia Pestis • Humans develop plague through contact with wild animals (sylvatic plague) or domestic or semidomestic animals (urban plague) or infected humans • Found in 200 species of mammals – rodents, without causing disease • Flea vectors – bacteria replicates in gut, coagulase causes blood clotting that blocks the esophagus; flea becomes ravenous 53 Figure 20.22 Infection cycle of Yersinia pestis 54 Pathology of Plague • ID 3-50 bacilli • Bubonic – bacillus multiplies in flea bite, enters lymph, causes necrosis and swelling called a bubo in groin or axilla • Septicemic – progression to massive bacterial growth; virulence factors cause intravascular coagulation subcutaneous hemorrhage and purpura – black plague • Pneumonic – infection localized to lungs, highly contagious; fatal without treatment 55 Figure 20.23 The bubo, classic sign of bubonic plague 56 • Diagnosis depends on history, symptoms, and lab findings from aspiration of buboes • Treatment: streptomycin, tetracycline, or chloramphenicol • Killed or attenuated vaccine available • Prevention by quarantine and control of rodent population in human habitats 57 Oxidase-Positive Nonenteric Pathogens • • • • • • Pasteurella multocida Haemophilus influenzae H. aegyptius H. ducreyi H. parainfluenzae H. aphrophilus 58 Pasteurella Multocida • Zoonotic genus; normal flora in animals • Opportunistic infections • Animal bites or scratches cause local abscess that can spread to joints, bones, and lymph nodes • Immunocompromised are at risk for septicemia and complications • Treatment: penicillin and tetracycline 59 Haemophilus • Tiny gram-negative pleomorphic rods • Fastidious, sensitive to drying, temperature extremes, and disinfectants • None can grow on blood agar without special techniques – chocolate agar • Require hemin, NAD, or NADP • Some species are normal colonists of upper respiratory tract or vagina (H. parainfluenzae, H. ducreyi) • Others are virulent species responsible for childhood meningitis, and chancroid 60 Haemophilus • H. influenzae – acute bacterial meningitis, epiglottitis, otitis media, sinusitis, pneumonia, and bronchitis – Subunit vaccine Hib • H. aegyptius – conjunctivitis, pink eye • H. ducreyi – chancroid STD • H. parainfluenzae and H. aphrophilus – normal oral and nasopharyngeal flora; infective endocarditis 61 Figure 20.25 Meningitis in the United States 62 Figure 20.26 Acute conjunctivitis 63