* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Neural Control Hierarchy Of The Heart Has Not Evolved To Deal
Survey
Document related concepts
Transcript
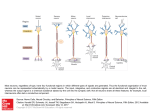
Articles in PresS. Physiol Genomics (May 21, 2013). doi:10.1152/physiolgenomics.00027.2013 1 Neural Control Hierarchy Of The Heart Has Not 2 Evolved To Deal With Myocardial Ischemia 3 G. Kember1 , J. A. Armour2 , M. Zamir3,4,† 1 Department of Engineering Mathematics, Dalhousie University, P. O. Box 1000, Halifax, Nova Scotia 2 Department of Pharmacology, Quillen College of Medicine, East Tennessee State University, Johnson City, Tennessee, 37614-8866. 3 Department of Applied Mathematics 4 Department of Medical Biophysics The University of Western Ontario London, Canada, N6A 5B7 † 4 corresponding author: [email protected] May 20, 2013 1 Copyright © 2013 by the American Physiological Society. Abstract 1 2 The consequences of myocardial ischemia are examined from the standpoint 3 of the neural control system of the heart- a hierarchy of three neuronal centers 4 residing in central command, intrathoracic ganglia, and intrinsic cardiac gan- 5 glia. The basis of the investigation is the premise that while this hierarchical 6 control system has evolved to deal with “normal” physiological circumstances, 7 its response in the event of myocardial ischemia is unpredictable because the 8 singular circumstances of this event are as yet not part of its evolutionary reper- 9 toire. The results indicate that the harmonious relationship between the three 10 levels of control breaks down- because of a conflict between the priorities which 11 they have evolved to deal with. Essentially, while the main priority in central 12 command is blood demand, the priority at the intrathoracic and cardiac levels 13 is heart rate. As a result of this breakdown, heart rate becomes less predictable 14 and therefore less reliable as a diagnostic guide as to the traumatic state of the 15 heart, which it is commonly used as such following an ischemic event. On 16 the basis of these results it is proposed that under the singular conditions of 17 myocardial ischemia a determination of neural control indices in addition to 18 cardiovascular indices has the potential of enhancing clinical outcome. 19 Keywords: Intrinsic cardiac nervous system. Central command. Neuroplasticity. 20 Neurocardiology. Heart rate. 2 1 1 Introduction 2 Myocardial ischemia is generally considered from the standpoint of its deleterious 3 effect on myocardial tissue and in conjunction with coronary artery disease. The 4 way in which the ischemic event affects the neural control of the heart, however, has 5 received little attention so far. The latter is clearly important because a derangement 6 of the neural control hierarchy of the heart may be ultimately as critical a determinant 7 of the clinical outcome of myocardial ischemia as is the damage of myocardial tissue. 8 In particular, the lack of or reduced blood supply to the ischemic region of the 9 myocardium will also have a direct effect on the viability of neural tissue within that 10 region. In addition, the altered chemical and/or mechanical milieu of the affected 11 cardiac tissue will lead to a greatly altered neural transduction from that region. 12 Both of these effects will impinge on the stable dynamics of the neural control system 13 of the heart in general and heart rate in particular. 14 In addition to direct damage to neural tissue, however, the ischemic event presents 15 the complex hierarchical neural control system of the heart with a set of singular 16 circumstances which the system has not evolved to deal with. The way in which 17 the system responds to these “new” circumstances, new on the evolutionary scale, is 18 currently unknown. The lack of this knowledge renders the interpretation of cardiac 19 indices at the time of myocardial ischemia, particularly heart rate, without a clear 20 physiological basis. The present study is an attempt to explore the physiological 21 pathways which the hierarchical neural control system of the heart may follow in the 22 event of myocardial ischemia, using a simulation of that event. 23 Some important experimental work have been done in the past to explore the neu- 24 rological aspects of myocardial ischemia. In a review by Eckberg (9) it was pointed out 25 that “Vagal and sympathetic cardiovascular control is deranged profoundly in patients 26 with congestive heart failure.” A study by del Rio et al (8) examined the electrical 27 changes induced by myocardial ischemia in dogs, concluding that “Parasympathetic 28 activity during acute coronary occlusion can protect against ischemia-induced ma- 29 lignant arrhythmias; nonetheless, the mechanism mediating this protection remains 3 1 unclear.” These studies illustrate the fact that experimental or clinical observations 2 in the event of myocardial ischemia, particulary of heart rate, provide the manifes- 3 tations of a derangement of the neural control system of the heart but they do not 4 provide the underlying mechanisms. The present study is therefore aimed at comple- 5 menting these observations by exploring the possible mechanisms of a derangement 6 of the neural control system of the heart caused by circumstances which the system 7 has not evolved to deal with. 8 Heart rate anomalies have been independently linked to pathologies including 9 coronary artery disease, myocardial infarction and heart failure (16,24). In particular, 10 elevated heart rate and reduced heart rate variability have been found to correlate 11 with increased risk of both atrial (22) and ventricular (27) arrhythmias. An elevated 12 heart rate in patients experiencing acute myocardial ischemia (AMI) has been linked 13 to an increase in the risk of mortality within one year of the event (2). Reduced heart 14 rate variability has been shown to be a risk factor for a poor outcome on the time 15 scale of several weeks after an AMI (5). Autonomic disturbances have been associated 16 with idiopathic ventricular arrhythmias (10), and disturbances within 30 minutes of 17 an AMI have been associated with increased risk of sudden cardiac death (31). 18 Studies of congenital heart disease have yielded similar results. An increased risk of 19 lethal ventricular arrhythmias after surgical repair of tetralogy of Fallot (6) and higher 20 incidence of mortality involving atrial tachyarrhythmias after Fontan surgery (7) were 21 observed in patients having reduced heart rate variability and baroreceptor sensitivity. 22 Reduced heart rate variability was also linked to sudden cardiac death in patients 23 with other forms of congenital heart disease (17) whether or not they had undergone 24 surgery. In these studies, and in a seminal review by (23), autonomic disturbance are 25 noted as being associated with an increased risk of atrial and ventricular arrhythmias. 26 There is thus mounting support for the view that derangement of the neural 27 control system of the heart may be ultimately as critical a determinant of the clinical 28 outcome of myocardial ischemia as is the pathological insult on myocardial tissue. In 29 addition, the lack of or reduced blood supply to the ischemic region of the myocardium 30 will have a direct effect on the viability of neural tissue within that region (1) and 4 1 may result in complex effects such as ischemic pre-conditioning (25), and the altered 2 chemical and/or mechanical milieu of the affected cardiac tissue will lead to a greatly 3 altered neural transduction from that region (26). Each of these effects will have a 4 highly variable impact on the dynamics of the neural control system of heart function 5 (13). 6 While the existence of these effects is not in any way questionable, as the above 7 studies indicate, they have not generally been considered so far because of the difficul- 8 ties involved in integrating such effects within the present view of the neural control 9 of heart function, specifically the view that this control resides largely in central com- 10 mand (4,16,19,20). This view is based on a central control system represented by pre- 11 to post-ganglionic efferent neurons, the preganglionic neurons residing in the central 12 nervous system. These central neurons are made up of medullary parasympathetic 13 and spinal cord sympathetic efferent preganglionic neurons. They receive sensory 14 inputs from cardiovascular afferent neurons for feed back of heart status. Hence, all 15 control decisions are assumed to emanate from the central nervous system. In this pa- 16 per we shall refer to this as the “central command” level of control, to be distinguished 17 from two other levels as described below. As such, the peripheral neural components 18 are seen as serving a passive role to either deliver centrally determined inputs to the 19 heart or to return feed back of heart status to the central nervous system. 20 Contrary to this view, it is our underlying hypothesis that peripheral neural com- 21 ponents must be considered in order to understand the full dynamics of neural control 22 of heart function and, for the purpose of the present paper, in order to determine the 23 full consequences of neural derangement during a cardiac ischemic event. Under- 24 standing the relationship between autonomic dysfunction and the onset of cardiac 25 arrhythmias cannot be explained solely within the scope of central neural command 26 theories (23). This is evident from anatomical and functional studies that have un- 27 covered intrathoracic extracardiac and intrinsic cardiac elements of the wider control 28 system of heart function (1, 11, 12). 29 To that end, we use a model of neural control of the heart based on a hierarchy of 30 three populations of neurons, the “top” level residing in central command, the “mid5 1 dle” residing within intrathoracic extracardiac ganglia, and the “bottom” residing 2 within intrinsic cardiac ganglia. At each level, neurons act both individually and in 3 concert with others. The ability of this model to explain heart rate anomalies, specif- 4 ically the presence and absence of heart rate oscillations (Mayer waves), has been 5 demonstrated previously (14). It was also shown that “networking” among neurons 6 endows this neural control system of the heart with a measure of plasticity that leads 7 to heterogeneity in neural behavior consistent with common observations (15). In 8 the present paper we explore the way in which this network plasticity and the inter- 9 play between and within the three levels of control respond to the singular conditions 10 created by myocardial ischemia. 11 2 12 2.1 13 The neural network on which our model is based has 3N neurons equally divided 14 among three levels of control to be referred to as levels 1,2,3 or “bottom”, “middle”, 15 “top”, or “cardiac”, “intrathoracic”, “central”, respectively. Two indices, j, k are 16 used to identify the k th neuron at the j th level. The state of activity (≡ level of 17 discharge) of neuron j, k is denoted by Sj,k which is scaled such that its value ranges 18 between 1.0 when the neuron is most active and 0.0 when it is inactive. 19 2.2 20 Broadly speaking, the neural network receives continuous updates of current demand 21 for blood flow and current heart rate, and processes these to produce an appropriate 22 change in heart rate. The main result of this algorithm, and the chief feature of the 23 model, is that demand for blood flow does not proceed directly to the heart or to 24 central command but to the neural network as a whole. Essential details of how this 25 occurs are given in what follows, more details can be found in (14, 15). 26 METHODS Neural Network Structure Heart Rate Control Algorithm Heart rate is constrained to lie between prescribed maximum and minimum values. 6 1 A scaled heart rate H is used in what follows, such that H = 1.0 when heart rate is 2 maximum and H = 0.0 when heart rate is minimum. 3 The dynamics of the neural network unfold piecewise at consecutive time intervals 4 t(n) , n = 1, 2, . . ., where demand for blood flow and current heart rate are used as 5 inputs and an incremental “move” ∆M (n) (t) is produced as output. The latter is 6 based on the mean activity of neurons at the cardiac level ∑N1 F 7 (n) = (n) k=1 S1,k (1) N1 such that ∆M (n) = β(F (n) − α) (2) (n) 8 where α is a reference activity level, β is a constant and S1,k , k = 1, 2, . . . , N1 , is the 9 level of activity of neurons at level 1 (cardiac) of the network at time interval t(n) . 10 Within each time interval, heart rate is a continuous function of time governed by a 11 first order linear system τH 12 dH (n) (t) + H (n) (t) = M (n) (t) dt (3) where τH is a time constant and M (n) (t) = i=n−1 ∑ ∆M (i) (t) (4) i=0 13 For simplicity, in what follows the time variable t shall not be shown explicitly but 14 will be implicit within each time interval t(n) . 15 2.3 16 The discharge from a neuron j, k within the network in time interval t(n) is represented 17 by the state of activity Sj,k of that neuron. This state is affected by (i) current blood 18 demand, (ii) current heart rate and, (iii) the level of activity of neighboring neurons. 19 A change in the state of activity the neuron due to these effects shall be denoted 20 respectively by δ1 Sj,k , δ2 Sj,k , δ3 Sj,k , and total change by ∆Sj,k . Neural Discharge (n) (n) (n) (n) (n) 7 1 We distinguish between two types of neurons (29,30): “heart rate neurons” which 2 are affected by only current heart rate and the activity of neighboring neurons, and 3 “blood demand neurons” which are affected by only demand for blood flow and the 4 activity of neighboring neurons. Thus the change in the state of activity of a neuron 5 j, k is given by (n) (n) (n) ∆Sj,k = δ1 Sj,k + δ3 Sj,k (n) (n) (n) ∆Sj,k = δ2 Sj,k + δ3 Sj,k heart rate neurons (5) blood demand neurons (6) 6 The extent to which heart rate H and blood demand D affect the state of activ- 7 ity of a neuron (j, k) are represented respectively by heart rate and blood demand 8 “sensitivities” hj,k and dj,k , such that (n) (n) (n) (n) δ1 Sj,k =− hj,k × H (n−L) (n) h (7) (n) 9 where H (n−L) is heart rate delayed by a time constant τL = L∆t and h is the mean (n) 10 of hj,k over the entire network and, similarly, (n) (n) δ2 Sj,k 11 = dj,k (n) d × D(n) Dmax (8) where the demand is scaled with respect to a maximum demand Dmax . 12 It is important to note, as indicated by the (n) superscripts, that the sensitivities 13 hj,k and dj,k can change from one time interval to the next, a feature which plays a 14 critical role following the onset of myocardial ischemia. This feature can be thought 15 of as a measure of “plasticity” in the sensitivities of neurons to heart rate and to 16 blood demand and we shall refer to it as “neural plasticity” to be distinguished 17 from “network plasticity” which represents plasticity in the neighbor weightings PJ,K 18 within the network. To demonstrate the role of neural plasticity following the onset 19 of myocardial ischemia, we shall compare a scenario in which this feature is enabled 20 (“neural plasticity: ON”) and one in which it is disabled (“neural plasticity: OFF”). (n) (n) (n) 8 1 2.4 Neural Networking 2 Another component of change in the activity of a neuron is due to the extent to which 3 it is affected by the activity of other neurons, which we refer to briefly as “networking” 4 and which is a key feature of our model. Networking occurs between a neuron and 5 its neighbors at the same level of the neural network and at the next adjacent level. 6 Thus, a neuron at the cardiac level has neighbors at the cardiac and intrathoracic 7 level, a neuron at central command has neighbors at the central and intrathoracic 8 levels, while a neuron at the intrathoracic level has neighbors at all three levels. 9 The degree of connectivity or “synaptic strength” between a neuron j, k and each 10 of its neighbors is represented by a weighting PJ(i),K(i) , where i = 1 . . . Nb(j,k) identify 11 the neighbors and J, K (upper case) are the positions of these neighbors within the 12 network. Again we note, from the superscript (n) that synaptic strength can change 13 from one time interval to the next, thus providing, in effect, a measure of plasticity 14 within the network as a whole (15). (n) 15 The way in which the state of activity of a neuron j, k is influenced by the state of 16 activity of its neighboring neurons J, K is what we have referred to as “networking” 17 among neurons and is represented by δ3 in Eqs.5,6. It is a key feature of the model 18 whereby every neuron within the network influences and is influenced by other neu- 19 rons. The extent of networking between a particular neuron j, k and its neighboring 20 neurons J(i), K(i) is determined by the sum of the difference prevailing in time in- 21 terval t(n) between the state of activity of that neuron and the states of activity of 22 the neighboring neurons, specifically ∑ ( Nb(j,k) (n) δ3 Sj,k = (n) (n) SJ(i),K(i) − Sj,k ) (n) × PJ(i),K(i) (9) i=1 23 2.5 Network Plasticity 24 The concept of plasticity, which has its origin in brain function, is now well accepted 25 as a property of neural networks in general (29, 30). As pointed out in the previous 26 section and demonstrated in (15), plasticity is enabled by allowing the connectivity 27 among neurons PJ(i),K(i) to change in time. The rules by which the change occurs are (n) 9 1 referred to as “plasticity rules” and there are currently two principal rules which are 2 believed to operate concurrently and which we implement in this paper. 3 (i) Homeostatic plasticity rule: Neurons that are making only minimal contribu- 4 tion to the overall network activity have their contribution increased while, 5 conversely, neurons that are making large contribution have their contribution 6 decreased. 7 (ii) Hebbian plasticity rule: Neurons that are making only minimal contribution to 8 the overall network activity have their contribution reduced even further while, 9 conversely, neurons that are making large contribution have their contribution increased even further. 10 11 The rules are implemented at time intervals ∆t = 0.01s. In all cases the change 12 in the activity of a neuron is influenced by a change in the values of its neighbor 13 weightings PJ(i),K(i) . (n) 14 It has been shown that both rules are required for the stability of a neural network 15 (18, 29, 30). However, the consequences of these rules following the singular event of 16 myocardial ischemia have yet to be tested and they form the main focus of the present 17 paper. For this purpose we examine the dynamics of the network with and without 18 the application of these rules and we refer to these conditions as “Network plasticity: 19 ON” and “Network plasticity: OFF” respectively. 20 2.6 21 The onset of myocardial ischemia is implemented by imposing a 50% step increase 22 in blood demand D(n) at the cardiac level of the network at time t = 500s. This 23 is followed, at times t ≥ 500s, by an incremental increase in the sensitivities dj,k of 24 blood demand neurons and a concurrent decrease in the sensitivities hj,k of heart rate 25 neurons throughout the network. The incremental changes ∆d, ∆h are very small, 26 distributed randomly in the range [0, 10−5 ], but they are implemented continually at The Onset of Myocadial Ischemia and Neural Plasticity (n) (n) (n) 27 every time step (∆t = 0.01s) up to a preset upper thresholds of dj,k = 0.99 and a 28 preset lower threshold of hj,k which is randomly distributed in the range [0, 0.1]. (n) 10 1 3 2 The aim of the results which we sought was to determine the way in which the three 3 neuronal centers respond to the ischemic event individually and collectively as they are 4 influenced by each other via network and neural plasticities. To that end we examined 5 heart rate and related properties of the neural control system under three conditions: 6 (i) network and neural plasticities OFF, (ii) network plasticity ON, neural plasticity 7 OFF, (iii) network and neural plasticities ON. Under the first condition networking 8 between neurons within and between the three control centers with the connectivity 9 among neurons being based on fixed parameters. Under the second condition these 10 parameters are variable, thereby giving rise to network plasticity. Under the third 11 condition, the sensitivities of neurons to blood demand and to heart rate, which are 12 based on fixed parameters in (i) and (ii), become variable and thereby give rise to 13 neural plasticity. In all cases a 2, 000s run of the system is executed. 14 15 Results The course of heart rate through the onset of myocardial ischemia and under the three states of the neural network is shown in Figure 1. 16 Networking among neurons gives rise to two streams of priorities within the net- 17 work which have previously been referred as “demand drive” and “heart drive” (14). 18 The heart drive of a neuron j, k is defined as the sum of the neuron neighbor weight- 19 ings PJ(i),K(i) multiplied by the sensitivity of hJ(i),K(i) of each of the neighbor neurons 20 to current heart rate, i.e. (n) (n) ∑ Nb(j,k) (n) Hdr (j, k) = (n) (n) (10) (n) (11) hJ(i),K(i) × PJ(i),K(i) i=1 21 while the demand drive is defined similarly as ∑ Nb(j,k) (n) Ddr (j, k) = (n) dJ(i),K(i) × PJ(i),K(i) i=1 22 The evolutions of these two drives under the three states of the neural network and 23 through the onset of the ischemic event are shown in Figures 2 and 3 respectively. 24 A measure of the extent to which network plasticity is at play in the dynamic 25 control of heart rate is the accumulated number of implementations of the Hebbian 11 1 and Homeostatic plasticity rules, as described in Section 2.5. The total number of 2 these implementations at the three levels of the network and under the three different 3 states of the network are shown in Figure 4. 4 The key feature of a neural “network” is that neurons within the network do not 5 respond en masse as a single unit but act individually while, at the same time, they 6 are influencing and are being influenced by each other. A mapping of the simultaneous 7 activities of neurons within the network is therefore useful for interpreting the ultimate 8 outcome, namely the pattern of heart rate, in terms of neural activity. Individual 9 neural cell activity or discharge Sj,k , scaled between 0 (inactive) and 1.0 (most active), 10 as described in Section 2.3, are shown for a representative selection of neuron from 11 each of the three levels of the network in Figures 5-7. 12 4 13 Key elements of discussion of the overall neural control of the cardiovascular system 14 include the role of baroreflexes in the control of blood pressure and the role of sym- 15 pathetic and parasympathetic drives in the control of heart rate. A discussion of 16 one or the other of these elements in isolation is an oversimplification because these 17 elements act interdependently rather than independently from each other. Because 18 of the complexity of the integrated system, however, many animal and human studies 19 have focused simply on the apparent effects of different stressors on heart rate (3, 8) 20 and heart rate variability (3, 9, 21, 28). In each case the intervening mechanism is 21 not known and is likely multifaceted, involving an interplay between baroreceptor 22 feedback and sympathetic/parasympathetic drive, followed by final implementation 23 by the hierarchical neural control system of the heart. To place our study and its 24 limitations in proper perspective, therefore, the focus of the study is on this final 25 stage of the process, namely on how the hierarchical neural control system of the 26 heart ultimately implements the changes in heart rate. (n) Discussion and Conclusions 27 The main purpose of this study was to investigate the response of the hierarchical 28 neural control network of the heart following the onset of myocardial ischemia. The 12 1 control network, consisting of three populations of neurons residing at the cardiac, 2 intrathoracic, and central command levels, has been shown previously (14) to produce 3 results that are more consistent with physiological observation of heart rate oscilla- 4 tions and variability. The basis of our investigation was the premise that while this 5 hierarchical control system has evolved to deal with “normal” physiological circum- 6 stances, its response in the event of myocardial ischemia is unpredictable because the 7 singular circumstances of this event are as yet not part of its evolutionary repertoire. 8 The use of a model to probe the question of what this response might be is therefore 9 not only apt but necessary. 10 In the event of myocardial ischemia, heart rate is used in the clinical setting both 11 as a diagnostic marker of the traumatic state of the heart as well as a guide to 12 appropriate action. The main focus is usually on stabilizing heart rate and restoring 13 blood flow to myocardial tissue. Our results suggest that, at the same time, attention 14 should also be directed towards the stability of the hierarchical neural control system 15 of the heart. 16 More specifically, the results indicate that the harmonious relationship within and 17 between the three levels of neural control of the heart breaks down because of a clash 18 of the priorities which the three levels of control have evolved to deal with. The 19 clash occurs, essentially, because these priorities are inappropriate in the singular 20 circumstances of myocardial ischemia. 21 In particular, while the main priority at central command is to respond to demands 22 for blood flow, the main priority at the cardiac and intrathoracic levels, as has been 23 demonstrated previously (14), is to process these demands before they actually reach 24 the heart and thereby provide a protective measure against excessive drive of the 25 heart. In other words, and in short, while the main priority in central command 26 is blood demand, the priority at the intrathoracic and cardiac levels is heart rate. 27 While these disparate priorities coexist in harmony under “normal” physiological 28 circumstances, presumably because they have evolved to do so, our results indicate 29 that this harmony breaks down under the singular conditions of myocardial ischemia. 30 An important outcome of this breakdown is that heart rate becomes less pre13 1 dictable and therefore less reliable as a diagnostic marker of the functional state of 2 the heart. Our results indicate that following the onset of myocardial ischemia, heart 3 rate actually becomes an emergent property dependent heavily on the state of the hi- 4 erarchical neural control system of the heart. On that basis we propose, in conclusion, 5 that under the singular conditions of myocardial ischemia, a determination of neural 6 control indices in addition to cardiovascular indices has the potential of enhancing 7 clinical outcome. 8 Summary: Under the singular conditions of myocardial ischemia, the neural con- 9 trol hierarchy of the heart breaks down and, consequently, heart rate becomes an 10 unpredictable property of that breakdown rather than an index of the traumatic 11 state of the heart caused by the ischemic insult on myocardial tissue. Under these 12 conditions, therefore, the monitoring of heart rate alone in the clinical setting may 13 not be a reliable guide to appropriate action. 14 5 15 This work was supported by the Natural Science and Engineering Research Council 16 of Canada. 17 References 18 19 Acknowledgment 1. Armour J. Cardiac neuronal hierarchy in health and disease. Am J Physiol 287:262-271, 2004. 20 2. Berton G, Cordiano R, Palmieri R, Gheno G, Mormino P, Palatini P. Heart rate 21 during myocardial infarction: relationship with one-year global mortality in men 22 and women. Can J Cardiol 18(5):495-502, 2002. 23 24 3. Billman GE. Heart rate variability a historical perspective. Front Physiol, Doi:10.3389/fphys.2011.00086, 2011. 14 1 4. Cacioppo J, Berntson G, Binkley P, Quigley K, Uchino B, Fieldstone A. Auto- 2 nomic cardiac control. ii. noninvasive indices and basal response as revealed by 3 autonomic blockades. Psychophysiology 31:586-598, 1994. 4 5. Casolo G, Stroder P, Signorini C, Calzolari F, Zucchini M, Balli E, Sulla A, 5 Lazzerini S. Heart rate variability during the acute phase of myocardial infarction. 6 Circulation 85(5):2073-9, 1992. 7 6. Davos CH, Davlouros PA, Wensel R, Francis D, Davies LC, Kilner PJ, Coats 8 AJ, Piepoli M, Gatzoulis MA. Global impairment of cardiac autonomic nervous 9 activity late after repair of tetralogy of fallot. Circulation 106(suppl)I69-75, 2002. 10 7. Davos CH, Francis DP, Leenarts MF, Yap SC, Li W, Davlouros PA, Wensel 11 R, Coats AJ, Piepoli M, Sreeram N, Gatzoulis MA. Global impairment of car- 12 diac autonomic nervous activity late after the fontan operation. Circulation 13 108(suppl)II180-5, 2003. 14 8. del Rio CL, Dawson TA, Clymer BD, Paterson DJ, Billman GE. Effects of acute 15 vagal nerve stimulation on the early passive electrical changes induced by myocar- 16 dial ischaemia in dogs: heart rate-mediated attenuation. Exp. Physiol. 93:931-944, 17 2008. 18 19 9. Eckberg DL. Baroreflexes and the failing human heart. Circulation 96:4133-4137, 1997. 20 10. Fei L, Statters D, Hnatkova K, Poloniecki J, Malik M, Camm J. Change of au- 21 tonomic influence on the heart immediately before the onset of spontaneous id- 22 iopathic ventricular tachycardia. J Am Coll Cardiol 24(6):1515-1522, 1994. 23 11. Horackova M, Armour J, Byczko Z. Distribution of intrinsic cardiac neurons in 24 whole-mount guinea pig atria identified by multiple neurochemical coding. A 25 confocal microscope study. Cell and Tissue Res 297:409-421, 1999. 26 12. Horackova M, Croll R, Hopkins D, Losier A, Armour J. Morphological and im- 27 munohistochemical properties of primary longterm cultures of adult guinea-14 15 1 pig ventricular cardiomyocytes with peripheral cardiac neurons. Tissue and Cell 2 28:411-425, 1996. 3 13. Huang M, Ardell J, Hanna B, Wolf S, Armour J. Effects of transient coronary 4 artery occlusion on canine intrinsic cardiac neuronal activity. Integ Physiol Behav 5 Sci 28:5-21, 1993. 6 7 8 9 10 11 14. Kember G, Armour J, Zamir M. Neural control of heart rate: The role of neuronal networking. J Theoret Biol 277:41-47, 2011. 15. Kember G, Armour J, Zamir M. Dynamic neural networking as a basis for plasticity in the control of heart rate. J Theoret Biol 317:39-46, 2012. 16. La Rovere M. Heart rate and arrhythmic risk: old markers never die. Europace 12:155-157, 2010. 12 17. Lammers A, Kaemmerer H, Hollweck R, Schneider R, Barthel P, Braun S, Wacker 13 A, Brodherr-Heberlein S, Hauser M, Eicken A, Schmidt G, Hess J. Impaired 14 cardiac autonomic nervous activity predicts sudden cardiac death in patients 15 with operated and unoperated congenital cardiac disease. J Thorac Cardiovasc 16 Surg 132:647-655, 2006. 17 18 19 20 18. Maffei A, Bucher D, Fontanini A. Homeostatic plasticity in the nervous system: Editorial. Neural Plasticity, doi:10.1155/2012/913472, 2012. 19. Malliani A, Schwartz P, Zanchetti A. Neural mechanisms in life-threatening arrhythmias. Am Heart J 100(5):705-15, 1980. 21 20. Matsukawa K. Central command: control of cardiac sympathetic and vagal effer- 22 ent nerve activity and the arterial baroreflex during spontaneous motor behaviour 23 in animals. Exp Physiol 97:20-28, 2011. 24 25 21. Monahan KD. A new answer to an old question: does ageing modify baroreflex control of vascular sympathetic outflow in humans? J Physiol 587:1857, 2009. 16 1 22. Okin P, Wachtell K, Kjedsen S, Julius S, Lindholm L, Dahlof B, Hille DA, Niem- 2 inen MS, Edelman JM, Devereux RB. Incidence of atrial fibrillation in relation 3 to changing heart rate over time in hypertensive patients: the life study. Circ 4 Arrhythmia Electrophysiol 1, 337-43, 2008. 5 23. Paton J, Boscan P, Pickering A, Nalivaiko E. The yin and yang of cardiac au- 6 tonomic control: Vago-sympathetic interactions revisited. Brain Res Rev 49:555- 7 565, 2005. 8 24. Pokorny J, Stanek V, Vrana M. Sudden cardiac death thirty years ago and at 9 present. the role of autonomic disturbances in acute myocardial infarction revis- 10 11 12 ited. Physiol Res 60:715-728, 2011. 25. Sanada S, Kitakaze M. Ischemic preconditioning: emerging evidence, controversy, and translational trials. Intl J Cardiol 97:263-276, 2004. 13 26. Seyedi N, Maruyama R, Levi R. Bradykinin activates a cross-signaling pathway 14 between sensory and adrenergic nerve endings in the heart: A novel mechanism 15 of ischemic norepinephrine release? J Pharmacol Exp Ther 290:656-663, 1999. 16 27. Soliman E, Elsalam M, Li Y. The relationship between high resting heart rate 17 and ventricular arrhythmogenesis in patients referred to ambulatory 24 h electro- 18 cardiographic recording. Europace 12:261-265, 2010. 19 20 21 22 23 24 25 26 28. Studinger P, Goldstein R, Taylor JA. Age- and fitness-related alterations in vascular sympathetic control. J Physiol 587:2049-2057, 2009. 29. Turrigiano G, Nelson S. Hebb and homeostasis in neuronal plasticity. Current Opinion in Neur 10:358-364, 2000. 30. Turrigiano G, Nelson S. Homeostatic plasticity in the developing nervous system. Nature Reviews Neuroscience 5(2):97-107, 2004. 31. Webb S, Adgey A, Pantridge J. Autonomic disturbance at onset of acute myocardial infarction. Br Med J 3:89-92, 1972. 17 1 Figure Captions 2 Figure 1: Heart rate as impacted by the onset of myocardial ischemia and increased 3 blood demand at t = 500s under three different states of the neural network as 4 indicated in each panel. In the absence of network plasticity and neural plasticity, 5 heart rate simply moves from one state of oscillation to another, with a small change in 6 the mean. With network plasticity ON, these oscillations are promptly extinguished 7 as has been shown previously (14). With the addition of neural plasticity, a dramatic 8 effect emerges as seen in the large panel. There is a clash between network plasticity 9 and neural plasticity, which in this paper is being referred to as “derangement” of the 10 control hierarchy of the neural network as discussed further in the text. 11 Figure 2: Heart drives, as defined in Eq.10, under the three states of the neural net- 12 work as indicated in the individual panels. With both network plasticity and neural 13 plasticity OFF, heart drives are constant at all three levels of the neural network: 14 cardiac (red), intrathoracic (green), central command (blue), because both compo- 15 nents of the drive are constant. With network plasticity ON, PJ,K become variable 16 which results in the initial rearrangement of heart drive at the three levels of the 17 network, followed by constant levels which are little affected by the onset of myocar- 18 dial ischemia at t = 500s. With the addition of neural plasticity, however, as hJ,K 19 become variable, heart drive drops sharply at the onset of myocardial ischemia, as the 20 demand for blood flow becomes a higher priority than heart rate particularly within 21 central command (blue). 22 Figure 3: Demand drives, as defined in Eq.11, under the three states of the neural 23 network as indicated in the individual panels. Results in the top two panels are similar 24 to those for heart drive described in Figure 2, but with both network plasticity and 25 neural plasticity ON (large panel), the large increases in demand drive following the 26 onset of myocardial ischemia at t = 500s are seen to be a clear counterpart to the 27 results for heart drive in Figure 2. 28 Figure 4: An accumulated count of implementations of the Hebbian (solid lines) and 18 1 Homeostatic (dashed) plasticity rules, the number of such implementations being a 2 measure of the extent to which network plasticity is at play in the dynamic control 3 of heart rate. As seen in the top two panels, these effects are absent when network 4 plasticity is OFF and are fairly constant when network plasticity is ON, very little 5 affected by the onset of myocardial ischemia. However, this picture changes drastically 6 with the addition of neural plasticity (lower panel). The number of implementations 7 rise at all three levels of the network (red: cardiac, green: intrathoracic, blue: central), 8 in piecewise fashion where the turning points coincide with those in the time course 9 of the heart rate seen in Figure 1. 10 Figure 5: Neural cell activity of a sample of 30 neurons at each of the three levels 11 of the network: cardiac (red), intrathoracic (green), blue (central command), with 12 network and neural plasticities OFF. Constant activity of a single neuron would 13 appear as a horizontal line at an activity level between 0 (inactive) and 1.0 (most 14 active). Oscillatory activity appears as lines moving up and down which on the large 15 time scale of the figure merge as a solid block. the figure thus shows oscillatory 16 cell activity before and after the onset of myocardial ischemia at t = 500s, which is 17 consistent with the oscillatory heart rate seen in the top left panel of Figure 1. The 18 present figure shows further that cell activity before the ischemic event is dominated 19 by the central command level, while after that event there are significant contributions 20 from the cardiac and intrrathoracic levels. 21 Figure 6: Neural cell activity as in Figure 5 but with network plasticity ON. Oscil- 22 latory behavior is promptly extinguished by the network plasticity, consistent with 23 the corresponding behavior of heart rate seen in the top right panel of Figure 1. The 24 onset of myocardial ischemia at t = 500s causes only a small “blip”, again consistent 25 with the corresonding behavior of heart rate. 26 Figure 7: Neural cell activity as in Figure 5 but with both network and neural 27 plasticities ON. Behavior before the onset of the ischemic event at t = 500s is seen to 28 be similar to that seen in Figure 6, but following that event a dramatic clash is seen 29 to unfold between the network plasticity and neural plasticity at the three levels of 19 1 control. The result is an alternating emergence and extinction of oscillatory behavior 2 which ultimately abates, again, consistent with the corresponding behavior seen with 3 heart rate in the lower panel of Figure 1. This is what in the present paper is being 4 referred to as “derangement” of the control hierarchy of heart rate. 20 0.4 0.4 Network plasticity OFF Neural plasticity OFF 0.3 heart rate heart rate 0.3 0.2 Network plasticity ON Neural plasticity OFF 0.2 0.1 0.1 0 0 0 0 1000 500 time (s) 1000 500 time (s) 0.4 0.35 Network plasticity ON Neural plasticity ON heart rate 0.3 0.25 0.2 0.15 0.1 0.05 0 0 500 1000 time (s) 1500 2000 Figure 1: Heart rate as impacted by the onset of myocardial ischemia and increased blood demand at t = 500s under three different states of the neural network as indicated in each panel. In the absence of network plasticity and neural plasticity, heart rate simply moves from one state of oscillation to another, with a small change in the mean. With network plasticity ON, these oscillations are promptly extinguished as has been shown previously (14). With the addition of neural plasticity, a dramatic effect emerges as seen in the large panel. There is a clash between network plasticity and neural plasticity, which in this paper is being referred to as “derangement” of the control hierarchy of the neural network as discussed further in the text. 21 1 1 Network plasticity ON 0.8 Neural plasticity OFF heart drive heart drive Network plasticity OFF 0.8 Neural plasticity OFF 0.6 0.4 0.2 0.6 0.4 0.2 0 0 500 time (s) 0 0 1000 500 time (s) 1000 1 heart drive 0.8 Network plasticity ON Neural plasticity ON 0.6 0.4 0.2 0 0 500 1000 time (s) 1500 2000 Figure 2: Heart drives, as defined in Eq.10, under the three states of the neural network as indicated in the individual panels. With both network plasticity and neural plasticity OFF, heart drives are constant at all three levels of the neural network: cardiac (red), intrathoracic (green), central command (blue), because both components of the drive are constant. With network plasticity ON, PJ,K become variable which results in the initial rearrangement of heart drive at the three levels of the network, followed by constant levels which are little affected by the onset of myocardial ischemia at t = 500s. With the addition of neural plasticity, however, as hJ,K become variable, heart drive drops sharply at the onset of myocardial ischemia, as the demand for blood flow becomes a higher priority than heart rate particularly within central command (blue). 22 1.5 2 Network plasticity OFF Neural plasticity OFF demand drive demand drive 2 1 0.5 0 0 500 time (s) 1.5 1 0.5 0 0 1000 Network plasticity ON Neural plasticity OFF 500 time (s) 1000 2 Network plasticity ON Neural plasticity ON demand drive 1.5 1 0.5 0 0 500 1000 time (s) 1500 2000 Figure 3: Demand drives, as defined in Eq.11, under the three states of the neural network as indicated in the individual panels. Results in the top two panels are similar to those for heart drive described in Figure 2, but with both network plasticity and neural plasticity ON (large panel), the large increases in demand drive following the onset of myocardial ischemia at t = 500s are seen to be a clear counterpart to the results for heart drive in Figure 2. 23 0.5 5 Network plasticity OFF Neural plasticity OFF Hebb/Homeo count Hebb/Homeo count 1 0 −0.5 −1 0 500 time (s) x 10 Network plasticity ON 4 Neural plasticity OFF 3 2 1 0 0 1000 7 500 time (s) 1000 7 5 x 10 Hebb/Homeo count 4 Network plasticity ON Neural plasticity ON 3 2 1 0 0 500 1000 time (s) 1500 2000 Figure 4: An accumulated count of implementations of the Hebbian (solid lines) and Homeostatic (dashed) plasticity rules, the number of such implementations being a measure of the extent to which network plasticity is at play in the dynamic control of heart rate. As seen in the top two panels, these effects are absent when network plasticity is OFF and are fairly constant when network plasticity is ON, very little affected by the onset of myocardial ischemia. However, this picture changes drastically with the addition of neural plasticity (lower panel). The number of implementations rise at all three levels of the network (red: cardiac, green: intrathoracic, blue: central), in piecewise fashion where the turning points coincide with those in the time course of the heart rate seen in Figure 1. 24 1 cell activity 0.8 0.6 0.4 0.2 0 0 200 400 600 time (s) 800 1000 Figure 5: Neural cell activity of a sample of 30 neurons at each of the three levels of the network: cardiac (red), intrathoracic (green), blue (central command), with network and neural plasticities OFF. Constant activity of a single neuron would appear as a horizontal line at an activity level between 0 (inactive) and 1.0 (most active). Oscillatory activity appears as lines moving up and down which on the large time scale of the figure merge as a solid block. the figure thus shows oscillatory cell activity before and after the onset of myocardial ischemia at t = 500s, which is consistent with the oscillatory heart rate seen in the top left panel of Figure 1. The present figure shows further that cell activity before the ischemic event is dominated by the central command level, while after that event there are significant contributions from the cardiac and intrrathoracic levels. 25 1 cell activity 0.8 0.6 0.4 0.2 0 0 200 400 600 time (s) 800 1000 Figure 6: Neural cell activity as in Figure 5 but with network plasticity ON. Oscillatory behavior is promptly extinguished by the network plasticity, consistent with the corresponding behavior of heart rate seen in the top right panel of Figure 1. The onset of myocardial ischemia at t = 500s causes only a small “blip”, again consistent with the corresonding behavior of heart rate. 26 1 cell activity 0.8 0.6 0.4 0.2 0 0 500 1000 time (s) 1500 2000 Figure 7: Neural cell activity as in Figure 5 but with both network and neural plasticities ON. Behavior before the onset of the ischemic event at t = 500s is seen to be similar to that seen in Figure 6, but following that event a dramatic clash is seen to unfold between the network plasticity and neural plasticity at the three levels of control. The result is an alternating emergence and extinction of oscillatory behavior which ultimately abates, again, consistent with the corresponding behavior seen with heart rate in the lower panel of Figure 1. This is what in the present paper is being referred to as “derangement” of the control hierarchy of heart rate. 27