* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Medical Evaluation of the HIV Dental Patient
Infection control wikipedia , lookup
Dental emergency wikipedia , lookup
Dental degree wikipedia , lookup
Medical ethics wikipedia , lookup
Epidemiology of HIV/AIDS wikipedia , lookup
Focal infection theory wikipedia , lookup
HIV and pregnancy wikipedia , lookup
Diseases of poverty wikipedia , lookup
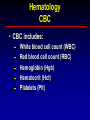
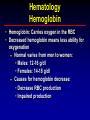
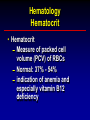
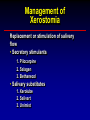
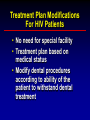
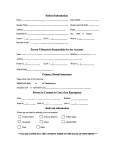
Module 1 Medical Evaluation of the HIV Dental Patient Medical Evaluation of the HIV Dental Patient Louis G. DePaola, DDS, MS Professor, Department of Diagnostic Sciences and Pathology Dental School University of Maryland Baltimore Director, Dental Training Pennsylvania-MidAtlantic AIDS ETC Michael Glick, DMD Professor and Chairman, Department of Diagnostic Sciences University of Medicine and Dentistry of New Jersey Director, Dental Training New Jersey, AIDS ETC Dr. Valli I. Meeks, DDS, MS RDH Department of Diagnostic Sciences and Pathology Dental School University of Maryland Baltimore Medical Evaluation of the HIV Dental Patient • Dental management of HIV infected patients does not differ from that of non-HIV infected patients. Most treatment can be performed by general practitioners. No special facility or equipment is required. “Standard Precautions” are followed. • HIV infected patients who require specialist care should be appropriately referred according to the same referral protocol as for the non-HIV infected patient. e.g. oral medicine, oral pathology, oral surgery, endodontics, periodontal therapy, orthodontics, pedodontics, prosthodontics Medical Evaluation of the HIV Dental Patient • A comprehensive medical and oral health assessment is an essential component for safe and appropriate oral health care. HIV infected persons often present with medical problems resulting from HIV-related immune suppression and co-morbid conditions. Early recognition and intervention for opportunistic infections (OIs) can significantly reduce morbidity and improve the quality of life for patients infected with HIV disease. Medical Evaluation of the HIV Dental Patient • HIV-infected patients are living longer and develop chronic diseases, many secondary to the toxicity of their medications, including Lipodystrophy Hyperglycemia Liver disease Medical Concerns • Patient’s susceptibility to infections • Impaired hemostasis • Drug actions and interactions • Ability to withstand the stress and trauma due to dental care Medical Problem List • Patient’s susceptibility to infections Hemodialysis Bacterial endocarditis Poorly controlled diabetes mellitus Medical Problem List • Impaired hemostasis Hemophilia Liver disease due to: • Hepatitis B infection and/or • Hepatitis C infections and/or • Alcohol, substance use/abuse Idiopathic thrombocytopenia purpura Medical Problem List • Drug actions and interactions Avoid acetaminophen in patients with severe liver disease Avoid NSAIDs, including aspirin, in patients with impaired hemostasis Recognize side-effects and drug-interactions with antiretroviral medications • See Module 3, part 3 Medical Problem List • Ability to withstand the stress and trauma due to dental care Cardiovascular disease Stroke Poorly controlled diabetes mellitus Medical History • A medical history (MHx) should be recorded for each patient. • A thorough MHx should be recorded every 6 months. • An abbreviated updated MHx should be recorded at every visit. Medical History • Medical history should include: Chief complaints and history of present illness Review of past medical history Hospitalizations and surgeries Current/recent illnesses Medications Allergies Substance Review abuse history of systems Systems Review Cardiovascular system Respiratory system Central nervous system Gastrointestinal system Genitourinary system Musculoskeletal system Endocrine system Skin Head and neck Dental Examination • Document base line pulse and blood pressure • Record pulse and blood pressure every visit for patients with hypertension or who are taking anti-hypertensive medications • Intra and extra-oral examination HIV Disease History • Date of HIV infection if known • Current HIV disease progression CD4 count - trend (up, down, stable) Viral load - trend (up, down, stable) • History of opportunistic infection(s) • Medication(s) Medications • Current Medications including: Prescription medications, OTC, herbal, naturopathic and homeopathic remedies and treatments, and nutritional supplements • HIV patients are frequently on numerous antiretroviral medications with complex dosing regimens. • Numerous drug-to-drug interactions have been well documented. • A complete listing of all medications is essential to minimize potential adverse drug interaction to medications that may be prescribed by the dental provider. Opportunistic Infections • History of opportunistic infections • Previous viral, fungal or bacterial infections • Current or previous antibiotic prophylaxis for opportunistic infections • Malignancies (including site) Kaposi’s sarcoma (KS) Non-Hodkins Lymphoma (NHL) Other Medical Consultation and Laboratory Testing • Patients with HIV infection often have chronic/systemic disease(s) that is unrelated to HIV. When providing treatment for HIV infected patients, as with any non-infected patient, a medical consultation may be indicated. • The following additional information is indicated and can usually be obtained from the patients physician: Hematological Blood Values Indication of patient’s risk for infection and bleeding tendencies • Complete Blood Count (CBC) Platelet count Differential blood cell count • Liver enzymes • Coagulation tests Hematology CBC • CBC includes: White blood cell count (WBC) Red blood cell count (RBC) Hemoglobin (Hgb) Hematocrit (Hct) Platelets (Plt) Hematology CBC • Total white and red blood cell count, hematocrit, and platelet counts are important in managing HIV patients: Many HIV+ patients are neutropenic, thrombocytopenic, and anemic Values indicate susceptibility to infection and bleeding Should be repeated at 3-6 month intervals • Patients with advanced HIV disease may require more frequent evaluation Hematology Differential White Blood Cell Count Total WBC: 4,000 – 11,000 cells/mm3 Neutrophils: 3,000-6,000 cells/mm3 – 30% – 70% of total WBC • Lymphocytes: 1,500 – 4,000 cells/mm3 – 20% - 50% of total WBC • Monocytes: 200 - 900 cells/mm3 – 1% - 12% of total WBC • Eosinophils: 100 - 700 cells/mm3 – 0% - 3% of total WBC • Basophils: 20 - 50 cells/mm3 – 0% - 1% of total WBC Hematology WBC • Neutropenia Normal neutrophil count: • 4,500-10,000 cells/mm3 Mild neutropenia: • 2,500- 4,500 cells/mm3 Severe neutropenia: • Below 1,000 cells/mm3 Antibiotic prophylaxis is indicated with neutroplils < 500 cells/mm3 • Many clinicians use American Heart Association Regimen. However, others feel that antibiotic therapy should continue for as long as open wounds are present in the oral cavity. Hematology Red Blood Cells • Red Blood Cells Anemia is common in HIV disease Decrease in RBCs or Hgb often caused by antiretroviral therapy and other medications Normal RBC: 4.5 - 5.5 x 106 cells/mm3 Hematology Hemoglobin • Hemoglobin: Carries oxygen in the RBC • Decreased hemoglobin means less ability for oxygenation Normal varies from men to women: • Males: 12-16 g/dl • Females: 14-18 g/dl Causes for hemoglobin decrease: • Decrease RBC production • Impaired production Hematology Platelet Count Normal platelet count: 150,000 - 400,000 cells/mm3 Thrombocytopenia: Decreased platelet count 100,000 - 140,000 cells/mm3 > 50-60,000 cells/mm3, adequate for routine dental care including simple extractions < 20,000 may see spontaneous bleeding Thromboytopenia is associate with bruising, and petechiae of skin and mucosa Hematology Hematocrit • Hematocrit Measure of packed cell volume (PCV) of RBCs Normal: 37% - 54% indication of anemia and especially vitamin B12 deficiency Hematology Liver Enzymes • ALT, AST values Non-specific transaminases • Often elevated with acute liver disease • Marked elevation may indicate decreased liver function • Patients may be prone to hemorrhage • Drug metabolism may be impaired Hematology Coagulation Tests Indicates patient’s clotting ability Increase indicates: Coagulation abnormality due to liver disease Other systemic diseases Anticoagulant therapy Medications Significantly elevated coagulation test results may require modification of dental treatment Hematology Coagulation Tests Coagulation tests: Prothrombin time (PT) • Normal: 9-11 seconds Activated partial thromboplastin time (aPTT) • Normal: 28-38 seconds INR (international normalized ratio) • Normal: 1.0 • >2.0 indicative of possible use of anticoagulation medications such as Coumadin® Immunological Blood Values CD4 Count • CD4 Count Indicates HIV progression and degree of immune suppression Normal CD4 count 800-1000 cells/mm3 • Major opportunistic infections frequently seen with CD4 cell count <200 cells/mm3 • CD4 cell count < 200 cells/mm3 is an AIDS diagnosis CD4 Counts (T-4 Helper Lymphocyte) Absolute CD4 helper count Total number of CD4 cells/mm3 CD4 % Percent of CD4 cells of the total lymphocytes • “Healthy” and usually asymptomatic patients – CD4 cell count >500 cells/mm3 (>29%) • Symptomatic patient – CD4 cell count of 200-499 cells/mm3 (14-28%) AIDS: – CD4 cell count <200 cells/mm3 (<14%) Immunological Plasma Viral Load • Plasma Viral Load: Indication of degree of viral replication and suggestion of immune suppression • Destruction of CD4 lymphocytes Measure of therapeutic (HAART) success or failure Prognostic: • The higher the viral load, the faster the progression of HIV disease and the poorer the long term prognosis Viral Load Listed (usually) on lab results as: HIV-1 RNA by PCR < 10,000 copies/ml suggests a mean survival rate of >10 years > 30,000 copies/ml suggest a mean survival rate of <5 years Confidentiality • At all times, confidentiality must be maintained for all patients, regardless of HIV serostatus. • Proper consent should be obtained before any confidential medical or dental information is released to other medical or dental providers. Dental Treatment Plan Priorities • • • • • Alleviate pain Prevent further oral disease Restore function Restore esthetics Improve quality of life Restorative/Prosthodontic Considerations • • • • • Ability to perform oral hygiene Caries index Reduced salivary flow Presence of oral lesions “End of life” concerns/issues Management of Xerostomia Replacement or stimulation of salivary flow • Secretory stimulants 1. Pilocarpine 2. Salagen 3. Bethanecol • Salivary substitutes 1. Xerolube 2. Salivart 3. Unimist Treatment Plan Modifications For HIV Patients • No need for special facility • Treatment plan based on medical status • Modify dental procedures according to ability of the patient to withstand dental treatment Treatment Plan Modifications For HIV Patients • Treatment plan based on: Medical status Finances Patient acceptance • Modify dental procedures according to ability of the patient to tolerate dental procedures Antibiotic Prophylaxis Indicated when: Neutrophils: <500 cells/mm3 According to AHA guidelines if patient has heart/valvular problems Need for antibiotic prophylaxis is not based on CD4 count Antibiotic Prophylaxis Patients with indwelling catheters such as a Hickman catheter may require antibiotic prophylaxis prior to dental care. Medical consultation may be warranted. Renal dialysis patients with shunts for hemodialysis require antibiotic prophylaxis prior to invasive dental care. Selected Bibliography 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. The American Academy of Oral Medicine. Clinicians Guide to HIV-Infected Patients, 2001, 3rd Edition, Editors: Patton L & Glick M, Baltimore, MD 21209. Molinari JA, Glick M. Infectious Diseases. In Burket’s Oral Medicine. Greenberg MS, Glick M. Eds. BC Decker Inc. Hamilton, Ontario, Canada. 2002 pp. 525-562 Bartlett J and Gallant J. Medical Management of HIV Infection, 2001-2002 Edition, Publisher: Johns Hopkins University School of Medicine, Department of Infectious Diseases, Baltimore, MD. Department of Health and Human Services (DHHS) and the Henry J. Kaiser Family Foundation. Guidelines for the Use of Antiretroviral Agents in HIV-Infected Adults and Adolescents; May 2001. Available for download at: http://www.hivatis.org. Department of Health and Human Services (DHHS). USPHS/IDSA Guidelines for the Prevention of Opportunistic Infections in Persons Infected with Human Immunodeficiency Virus. July 2001. Available for download at: http://www.hivatis.org. Infection Control Recommendations for the Dental Office and the Dental Laboratory ADA Council on Scientific Affairs and ADA Council on Dental Practice available for download at https://w3.ada.org/prof/prac/issues/topics/icontrol/ic-recs/index.html. HIVDENT. Dental Treatment Considerations, August 2001; available for download at http://www.hivdent.org/dtc.htm. The Dental Alliance for AIDS/HIV Care. Principles for the Oral Health Management of the HIV/AIDS Patient, 2001; available for download at http://www.critpath.org/daac/standards.html Infection Control Guidelines: September,1997; Organization for Safety & Asepsis Procedures (OSAP); available for download at http://www.osap.org/resources/IC/icguide97.htm. Centers for Disease Control and Prevention (CDC). Recommended Infection Control Practices for Dentistry, 1993. MMWR Morb Mortal Wkly Rep. 1993; 42(RR-8) 1-20.