* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
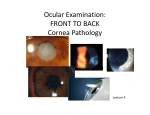
Download Miscellaneous corneal conditions (Imp for UGs)
Survey
Document related concepts
Transcript
Corneal dystrophies & other miscellaneous corneal conditions MBBS KGMU Common corneal disorders • Keratitis/ corneal ulcer. • Corneal trauma. • Keratomalacia. • Ectatic conditions. • Corneal dystrophies. • Corneal degenerations. Differences between dystrophy & degeneration Corneal dystrophy • Bilaterally symmetrical. • Often hereditary. • Limited to a particular corneal layer. • Non-inflammatory. Corneal degeneration • Non-hereditary. • Usually unilateral sometimes bilateral. • Not strictly limited to a particular corneal layer. • Non inflammatory Corneal dystrophies Corneal Dystrophies • Epithelial & sub-epithelial. • Bowman’s membrane. • Stromal. • Endothelial. Epithelial, sub-epith & Bowman’s corneal dystrophies • Epithelial & sub-epithelial – manifest in adults. • Epithelial basement membrane dystrophy. • Meesman dystrophy. • Bowman’s layer dystrophies – manifest in childhood. • Thiel Behnke corneal dystrophy. • Reis-Bucklers corneal dystrophy. Comparison between epithelial, subepithelial, Bowman’s dystrophies • Similarities: • Symptoms: • Asymptomatic / associated with recurrent corneal erosions. • Foreign body sensation & watering. • Treatment by PTK –photo-therapeutic keratectomy by EXCIMER LASER. • Difference: Slit lamp examination shows patterns typical for each one. Meesman’s dystrophy (intra-epithelial microcystic appearance) Stromal Dystrophies • Granular form • Lattice form • Macular form Bilateral. Manifest at puberty. Diminution of vision is the presenting complaint. Central cornea. Granular stromal dystrophy AD. Crumb-like accumulation of hyaline material Lattice dystrophy (AD. Criss-cross lines). Macular Dystophy AR Opacities dispersed throughout stroma. Endothelial dystrophies • Fuchs endothelial dystrophy – AD. Elderly. • CHED – Congenital hereditary endothelial dystrophy. AD/AR. • PPMD –Posterior polymorphous dystrophy. AD. Features common to all endothelial dystrophies • Limbus-to-limbus corneal clouding • Bilateral. • Endothelium is attenuated or even absent • Oedematous cornea may be 2-3 times normal thickness. • Generalised haze or diffuse ground glass appearance. • Photophobia and lacrimation in late stages due to bullous keratopathy. Specular microscopy in endothelial dystrophy Normal endothelim Decreased cell count, pleomorphism, polymegathism Congenital hereditary endothelial dystrophy (CHED) • Autosomal dominant (later in infancy). • Autosomal recessive • Earlier presentation (at birth; nystagmus). CHED Posterior polymorphous dystrophy • Autosomal dominant. • Bilateral. • 2nd or 3rd decade….rarely -in early infancy. • Vesicle like lesions in non-banded part of Descemet’s membrane. • Periph ant synechiae & raised IOP may be present. Management of endothelial dystrophies • Specular microscopy – for endothelial cell count. • Pachymetry –corneal thickness. Treatment required if symptomatic. Symptomatic treatment: • Hypertonic saline eye drops. • Bandage contact lens. Definitive treatment: Endothelial keratoplasty (DSAEK). Penetrating keratoplasty. Corneal degenerations Corneal degenerations • Arcus senilis / juvenilis. • Band shaped keratopathy. • Terriens marginal degeneration. • Salzmann nodular degeneration. • Spheroidal degeneration. Arcus senilis Terrien marginal degeneration • Bilateral. • Progressive thinning of superior peripheral cornea. • No inflammation. • Presents with myopia or astigmatism. Band shaped keratopathy • Horizontal opacification in palpebral aperture. • Chronic uveitis, silicon oil. • Blind shrunken eyes. • Hyperparathyroidism, sarcoidosis. • Treatment – chelation with EDTA. • PTK ?? Ectatic conditions Ectatic conditions (non inflammatory) • Keratoconus. • Pellucid marginal degeneration. • Keratoglobus. Keratoconus • Congenital weakess of corneal collagen. • Conical shape of cornea because of central thinning and bulging (Munson sign). • Manifests after puberty. • High myopia & astigmatism. • Treatment options: • Rigid contact lens. • Corneal cross linking (C3R). • Keratoplasty. Keratoconus Pellucid marginal degeneration • Painless bilateral thinning of inferior peripheral cornea. • Myopia & astigmatism. • It is probably a variant of keratoconus. Keratomalacia Keratomalacia • Bilateral. • Rapidly increasing clouding of cornea. • No congestion. • Melting of cornea. • Night blindness +/• Other features of malnutrition / diarrhoea. • Timely injecs of Vit A & control of malnutrition. Corneal injuries • Best possible repair also ends up in subnormal visual gain. • Timely keratoplasty is required in visually significant opacity to prevent amblyopia. • Donor tissue selection should be very carefully done - good endothelial count. Need of the hour • Proper education of medical personnel, school teachers and health workers regarding causes and prevention of childhood blindness. • Training of medical personnel at primary and secondary health care centres regarding early diagnosis of treatable conditions and suitable management. • To know ‘when to refer’ to higher centre. • Over-the-counter sale of corticosteroid eye drops to be stopped. Our students are the future of this beautiful institution Do your best always text