* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download - Catalyst
Coronary artery disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Atrial septal defect wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
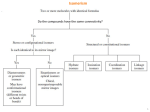
Heterotaxy Syndrome: considering malrotation Isaac Chuang Stein Seattle Children’s Hospital General Pediatric Surgery Thursday August 13, 2015 Outline • Intro to Heterotaxy • Epidemiology • Ways to stratify Heterotaxy patients • Clinical Presentation • Implications for intestinal malrotation What is Heterotaxy? • Internal thoraco-abdominal organs demonstrate abnormal arrangement across the left-right axis of the body; broad spectrum • Results in an unusual degree of symmetry between the right and left sides of the body • Can involve the heart, liver, lungs, intestine, and spleen • Associated with mutations of genes that encode proteins that are components of the TGF-B pathway1 • NODAL, NKX2-5, CRELD1, LEFTY2, ZIC3, CRIPTC Epidemiology • HS occurs in 1 in 10,000-40,000 births2 • Equal distribution between male and female • Equal risk across varying ethnic groups • *Within the Heterotaxy population, 32-89% are estimated to have intestinal rotation anomalies8 Ways to stratify patients • Atrial appendage isomerism • Right atrial isomerism vs. Left atrial isomerism • Used to describe whether heart has two “right” atria or two “left” atria • Polysplenia syndrome vs. Asplenia syndrome • Situs inversus • Right/left asymmetry remains • Mirror image of normal anatomy • Will only have one spleen Right Atrial Isomerism (RAI) • “Two right sides” • Heart with bilateral right atria and atrial appendages • Absence of left-sided structures (such as coronary sinus) • Consistent heart defects • • • • Absent atrial septum3,4 Anomalous pulmonary venous drainage3,4 Pulmonary outflow tract obstruction3,4 Single ventricle physiology3,4 • Absent spleen Left Atrial Isomerism (LAI) • “Two left sides” • Heart with bilateral left atria and atrial appendages • Cardiac abnormalities • *Interrupted IVC – characteristic (80%)5 • Highly variable atrial septal anatomy • Commonly show polysplenia Polysplenia vs. Asplenia Polysplenia Asplenia • Spleen seen on left and right sides of abdomen • Spleen absent from abdomen • Indicative of left atrial isomerism and its associated abnormalities • Indicative of right atrial isomerism and its associated abnormalities How will they present? • Antenatal • Fetal complete heart block – consider LAI6 • AV canal defect with ventricular asymmetry – consider RAI • Postnatal • Cyanosis – due to right-to-left shunting secondary to pulmonary artery outflow obstruction • Respiratory distress – pulmonary congestion due to obstructed pulmonary veins • *Presentation of patients with RAI is much more severe How will they present? • Noncardiac presentations • Sepsis – secondary to asplenia in RAI • Jaundice – secondary to biliary atresia (10% of LAI)7 • Bilious vomiting – secondary to malrotation Risk of malrotation • Intestinal rotational anomalies have been reported in 32-89% of patients with Heterotaxy8 • Malrotation has been described in both RAI and LAI • May be asymptomatic; must always consider malrotation in a patient with HS • Evaluation and management of the asymptomatic patient is controversial Malrotation in RAI vs. LAI • Hill et al. 2014, 38 patients with HS identified. • 18/38 underwent diagnostic laparoscopy or laparotomy based on upper GI findings or clinical symptoms worrisome for malrotation (bilious emesis, abdominal distension, bloody BM) • Malrotation identified in 8/18 patients (44%) who underwent surgery • Presence of abdominal symptoms predictive of identifying malrotation (80%) LAI vs. RAI • Likelihood of malrotation in LAI is significantly lower than in RAI (15% vs 72%)10 • Especially in an asymptomatic patient with LAI Hill et al. 2014 Management of the asymptomatic patient • Risks vs. benefits of surgery must be weighed heavily in his patient population • Avoid overtreating, especially in these patients with cardiac anomalies • Papillon et al. in 2013 • 30 asymptomatic HS patients with upper GI findings indicative of malrotation • 0% had true malrotation or a narrow mesentery at time of exploration Treatment algorithm Hill et al. (2014) Alternative approach • Yu et al. 2009 retrospective review over 1997-2007 (Boston Children’s) • 31 HS patients compared to 51 non-HS patients undergoing Ladd’s • No significant difference found in… • Rates of SBO • Hospital stay • Hospital mortality • Routine screening and elective Ladd’s procedure to any patient with HS with positive upper GI given possible catastrophic outcome of volvulus Multicenter Analysis • Salavitabar et al. 2015 (NYPB, Columbia) • Inclusion criteria: HS, IRA shown on upper GI, asymptomatic • 325 patients at 41 tertiary care children’s hospitals (Pediatric Health Information System database) • 2004-2011 • Primary outcome: major morbidity or mortality on admissions subsequent to the initial hospitalization • Obstruction including volvulus, gut ischemia, intestinal resection, any subsequent admission. Multicenter Analysis • 188/325 (58%) underwent Ladd’s • Remainder managed with observation • Ladd’s procedure on initial hospitalization was associated with a 2.2x increase in odds of major morbidity or mortality (p=0.007) • Suggest that in an asymptomatic patient with HS, even with IRA seen on upper GI, cautious observation is safest. The asymptomatic patient • Multidisciplinary approach with cardiology, cardiac surgery, GI, etc… • Consider patient’s overall health/ability to undergo surgery • Ability to follow-up/social support • Consider isomerism if present • Comfort level of surgeon with Ladd’s procedure References 1. Kosaki K, Bassi MT, Kosaki R, et al. Characterization and mutation analysis of human LEFTYA and LEFTYB, homologues of murine genese implicated in left-right axis development. Am J Hum Genet 1999; 64: 712. 2. Lim JS, McCrindle BW, Smallhorn JF, et al. Clinial features, management, and outcome of children with fetal and postnatal diagnoses of isomerism syndromes. Circulation 2005; 112: 2454. 3. Sapire DW, Ho SY, Anderson RH, Rigby ML. Diagnosis and significance of atrial isomerism. Am J Cardiol 1986; 58: 342. 4. Stranger P, Rudolph AM, Edwards JE. Cardiac malpositions. An overview based on study of sixty-five necropsy specimens. Circulation 1977; 56: 159 5. Sharma S, Devine W, Anderson RH, Zuberbuhler JR. Identification and analysis of left atrial isomerism. Am J Cardiol 1987; 60: 1157. 6. Ho SY, Fagg N, Anderson RH, et al. Disposition of the atrioventricular conduction tissues in the heart with isomerism of the atrial appendages: its relation to congenital complete heart block. J Am Coll Cardiol 1992; 20: 904. 7. Tanano H, Hasegawa T, Kawahara H, et al. Biliary atresia associated with congenital structural anomalies. J Pediatr Surg 1999; 34: 1687. 8. Strouse PJ. Disorders of intestinal rotation and fixation (“malrotation”). Pedatr Radiol 2004; 34(11): 837-51. 9. Ferdman B, States L, Gaynor JL, et al. Abnormalities of intestinal rotation in patients with congeniral heart disease and the heterotaxy syndrome. Congenit Heart Dis 2007; 2(1): 12-8. 10. Hill SJ, Heiss KF, Mittal R, et al. Heterotoxy syndrome and malrotation: Does isomerism influence risk and decision to treat. J Pedatr Surg 2014; 49: 934937. 11. Papillon S, Goodhue CJ, Zmora O, et al. Congenital heart disease and heterotaxy; upper gastrointestinal fluoroscopy can be misleading and surgery in an asymptomatic patient is not beneficial. J Pedatr Surg 2013; 48: 164-9. 12. Yu DC, Thiagarajan RR, Laussen PC, et al. Outcomes after the Ladd procedure in patients with heterotaxy syndrome, congenital heart disease, and intestinal malrotation. J Pediatr Surg 2009; 44: 1089-95. 13. Salavitabar A, Anderson B, Aspelund G, et al. Heterotaxy syndrome and intestinal rotational anomalies: Impact of the Ladd procedure. J Pediatr Surg 2015; In press.