* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download CARDIOPULMONARY RESUSCITATION
Survey
Document related concepts
Transcript
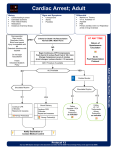
CARDIOPULMONARY RESUSCITATION CARDIAC ARREST Abrupt loss of consciousness caused by lack of adequate cerebral blood flow due to failure of cardiac pump function. Survival depends on • The setting in which arrest occurs • Electrical mechanisms • Underlying clinical status Electrical mechanisms • • • • Ventricular fibrillation Pulseless VT Asystole Pulseless electrical activity PHASES OF VF ELECTRICAL (0-4 min) o adequate myocardial ATP store o defibrillation alone restore perfusing o rhythm(without chest compressions) o duration of this phase can be prolonged by bystander CPR. Circulatory phase(4-10 min) depletion of ATP store, lactic acidosis defibrillation without chest compression rarely successful, may result in PEA ECG fine fibrillatory wave. Metabolic phase(>10 min) terminal phase irreversible damage less chance of successful defibrillation mild therapeutic hypothermia delay the onset. Pulseless electrical activity H “S • Hypoxia • Hypovolemia • Hydrogen ion(acidosis) • Hypo/hyperkalemia • Hypothermia. T”S • Toxins • Tamponade • Tension pneumothorax • Thrombosis(pulmonary) • Thrombosis(coronary) Asystole • No cardiac electrical and mechanical activity of heart. • Terminal rhythm in non intervened PEA or VF • Same causes of PEA can also sometimes present initially as asystole AHA 2010 GUIDELINE • Recognition of SCA based on unresponsiveness and absence of normal breathing( ie the victim is not breathing or gasping) • Look ,listen, and feel removed • ABC Sequence CAB • Encourage hands only CPR • Continue effective chest compressions/CPR until return of spontaneous circulation (ROSC) or termination of resuscitative efforts • Continued de-emphasis on pulse check Ensure high-quality CPR • compressions of adequate rate and depth • Allowing full chest recoil between compressions • Minimizing interruptions in chest compressions • Avoiding excessive ventilation Chain Chainof ofSurvival Survival Immediate recognition and activation, early CPR, rapid defibrillation, effective advanced life support and integrated post-cardiac arrest care. ADULT BLS SEQUENCE Recognition of SCA unresponsive no breathing or only gasping Pulse checknot recommended for lay rescuer Healthcare provider –not more than 10 sec Early CPR Early CPR Chest Compressions Chest compressions consist of forceful rhythmic applications of pressure over the lower half of the sternum. These compressions create blood flow by increasing intrathoracic pressure and directly compressing the heart. This generates blood flow and oxygen delivery to the myocardium and brain. Effective chest compressions “push hard and push fast” rate of at least 100 compressions per minute compression depth of at least 2 inches/5 cm. Allow complete recoil of the chest after each compression, to allow the heart to fill completely before the next compression Minimizing interruptions in compressions A compression-ventilation ratio of 30:2 is recommended HANDS ONLY CPR • Initially during SCA with VF rescue breath are not important • Oxygen level remains adequate. • Gasping and passive chest recoil allow gas exchange. • Improves survival in OHCA Airway Control and Ventilation • During low blood flow states such as CPR, oxygen delivery to the heart and brain is limited by blood flow rather than by arterial oxygen content. • Advanced airway placement in cardiac arrest should not delay initial CPR and defibrillation • Empirical use of 100% inspired oxygen during CPR optimizes arterial oxyhemoglobin content and in turn oxygen delivery. Airway and Ventilations • Opening the airway (with a head tilt–chin lift or jaw thrust) followed by rescue breaths • Untrained rescuer will provide Hands-Only (compression-only) CPR and the lone rescuer who is able, should open the airway and give rescue breaths with chest compressions. • Ventilations should be provided if the victim has a high likelihood of an asphyxial cause of the arrest. Rescue Breaths • by mouth-to-mouth or bag-mask • Deliver each rescue breath over 1 second • Give a sufficient tidal volume to produce visible chest rise. • Use a compression to ventilation ratio of 30:2 Mouth-to-Mouth Rescue Breathing • Open the victim’s airway, pinch the victim’s nose • Create an airtight mouth-to-mouth seal. • Give 1 breath over 1 second, take a “regular” (not a deep) breath • A second rescue breath over next 1 second Ventilation With Bag and Mask • With room air or oxygen. • Positive-pressure ventilation without an advanced airway • Produce gastric inflation and its complications • To deliver approximately 600mL tidal volume. • Squeezing a 1-L adult bag about two thirds of its volume or a 2-L adult bag about one third. • Cycles of 30compressions and 2 breaths. • Delivers ventilations during pauses in compressions and each breath over 1 second. • Can use supplementary oxygen (O2concentration 40%, at a minimum flow rate of 10 to 12 L/min) when available. • When an advanced airway (ie, endotracheal tube, combitube,or laryngeal mask airway [LMA]) is in place during 2-person CPR, • give 1 breath every 6 to 8 seconds without attempting to synchronize breaths between compressions • This will result in delivery of 8 to 10 breaths/minute • There should be no pause in chest compressions for delivery of ventilations Cricoid Pressure • Applying pressure to the victim’s cricoid cartilage to push the trachea posteriorly and compress the esophagus against the cervical vertebrae • Used in a few special circumstances (eg, to aid in viewing the vocal cords during tracheal intubation, • The routine use of cricoid pressure in adult cardiac arrest is not recommended • During CPR cardiac output is 25% to 33% of normal • Oxygen uptake from the lungs and CO2 delivery to the lungs are also reduced • low minute ventilation (lower than normal tidal volume and respiratory rate) can maintain effective oxygenation and ventilation • Excessive ventilation is unnecessary and can cause gastric inflation and its resultant, regurgitation and aspiration • Excessive ventilation can be harmful because it increases Intrathoracic pressure decreases venous return to the heart diminishes cardiac output • Rescuers should avoid excessive ventilation (too many breaths or too large a volume) during CPR Universal Adult Basic Life Support (BLS) Algorithm Adult Advanced Cardiovascular Life Support • Advanced cardiovascular life support (ACLS) includes interventions to treat cardiac arrest, and improve outcomes of patients who achieve return of spontaneous circulation (ROSC). • Includes: -airway management, -ventilation support, and -Rhythm based management of cardiac arrest Advanced airways Advantages • Improved ventillation and oxygenation • Eliminate pauses in chest compressions • 1 breath every 6-8 sec(8-10 breath/min) • Reduce risk of aspiration Supraglotic airways • Laryngeal mask airways regurgitation less when ET is difficult neck injury positioning of patient is difficult for ET Provides equivalent ventillation comp. ET. • Esophageal tracheal tube • Laryngeal tube DEFIBRILLATION Initial shock • 360j for monophasic , same dose for subsequent shocks • 120-200j for biphasic defibrillator, subsequent dose same or higher. • If VF recurs use previously successful energy level Medication for arrest rhythms Vasopressors • Epinephrine 1 mg IV/IO every 3-5 min • Alpha-adrenergic receptor stimulation produces vasoconstriction. • Increases coronary perfusion pressure, • Cerebral perfusion pressure. Vasopressin • Non adrenergic • Coronary vasoconstrictor • Dose:40 units IV/IO ANTI ARRYTHMICS AMIODARONE • For VF/Pulseless VT unresponsive to CPR, defibrillation ,vasopressor • Initial 300mg IV/IO can be followed by 150mg Lidocaine • if amiodarone not available • initial dose 1 to 1.5 mg/kg IV • addl. Dose 0.5 to 0.75 mg/kg if not responding Magnesium sulphate • Used in torsades de pointes • Dose 1-2gm diluted in 5% D Post - cardiac arrest care Objective • Optimise cardio pulmonary function • Try to identify precipitating causes • Control body temperature to optimise • Neurological recovery • Identify and treat ACS Induced hypothermia • In comatose (lack of meaningful response to verbal commands) adult patients • With ROSC after out of hospital VF arrest (class 1) • In hospital arrest with any rhythm (class2 b) • Cooled to 32-340C for 12 -24 hrs • Inhibitory effect on adverse enzymatic and chemical reactions initiated by ischemia • Inhibits the release of glutamic and dopamine • Induces brain derived neurotropic factors • • • • Cooling blanket Ice packs Direct immersion in ice water IV ice-cold fluids (500 ml to 30 ml/kg NS or Ringer’s lactate) • Monitor with esophageal thermometer or bladder catheters in nonanuric patients THANK U THANK U 1.current recommendation for compression ventilation ratio a) 15:2 b) 30:2 c) 15:1 d) 1:5 2.initial dose of amiodarone in ACLS a)300 mg bolus b)150 mg bolus c)450 mg d)200 mg 3) Therapeutic hypothermia a)32-34 b)30-32 c)27-30 d)35 4)1st shock for VF with monophasic defibrillator is a)300 j b)360 j c)250 j d)200 j 5)Breath/min with advanced airway in CPR is a)8-10 b)5 c)7 d)2 6)Max .rate of defibrillation success is in which phase of VT a)Circulatory phase b)Electrical phase c)Metabolic phase d)Equal in all phase 7) rate of chest compression /min at least A)60 b)80 c)100 d)120 8)drug not used routinely in adult ACLS a)Epinephrine b)Amiodarone c)Vasopressin d)atropine 9)depth of chest compression A)3 cm b)5 cm c)4 cm d)6 cm 10)not a part of BLS A)Chest compression b)Bag and mask ventillation c)Manual defibrillation d)AED