* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Endovascular treatment of aortic coarctation
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Turner syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Drug-eluting stent wikipedia , lookup
Aortic stenosis wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
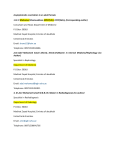
M I L E V I VA N M D S P E C I A L H O S P I TA L F O R S U R G I C A L D I S E A S E S “ F I L I P V T O R I ”, S K O PJ E Definition and anatomy Introduction • CoAo: – Simple definition: stenosis mostly in the thoracic descending aorta – Complex congenital heart disease • Significant anatomical variability • Diverse associated lesions • Histological abnormalities of the aorta Clinical presentation Class I 1. Every HTA pt have the brachial and femoral pulses palpated simultaneously . Bilateral brachial artery blood pressures and one popliteal artery blood pressures should be measured (Level of Evidence: C) 2. Initial imaging and hemodynamic evaluation by TTE, including suprasternal notch acoustic windows, is useful in suspected aortic coarctation. (Level of Evidence:B) 3. Every patient with coarctation (repaired or not) should have at least 1 cardiovascular MRI or CT scan for complete evaluation of the thoracic aorta and intracranial vessels. (Level of Evidence: B) *ACC/AHA 2008 Guidelines for Adults With CHD Diagnostics procedures Guidelines for Interventional and Surgical Treatment of Coarctation of the Aorta in adults Class I 1. Intervention for coarctation is recommended in the following circumstances: a. Peak-to-peak coarctation gradient greater than or equal to 20 mm Hg. (Level of Evidence: C) b. Peak-to-peak coarctation gradient less than 20 mm Hg in the presence of anatomic imaging evidence of significant coarctation with radiological evidence of significant collateral flow. (Level of Evidence: C) 2. Choice of percutaneous catheter intervention versus surgical repair of native discrete coarctation should be determined by consultation with a team of ACHD cardiologists, interventionalists, and surgeons at an ACHD center.(Level ofEvidence:C) 3. Percutaneous catheter intervention is indicated for recurrent, discrete coarctation and a peak-to-peak gradient of at least 20 mm Hg. (Level of Evidence: B) 4. Surgeons with training and expertise in CHD should perform operations for previously repaired coarctation and the following indications:) a. Long recoarctation segment. (Level of Evidence: B) b. Concomitant hypoplasia of the aortic arch. (Level of Evidence: B) Class IIb Stent placement for long-segment coarctation may be considered, but the usefulness is not well established, and the long-term efficacy and safety are unknown. ACC/AHA 2008 Guidelines for Adults With CHD Management of native CoAo Percutaneous treatment of congenital heart diseases in Filip Vtori Hospital (2003-2014) Treatment of congenital heart defects 180 160 156 140 120 100 80 69 54 60 40 28 2009-2014 25 24 20 6 2 Aortic stenosis Coronary AV fistula 0 ASD Pulmonary stenosis PDA VSD PFO Coarctation of the aorta Balloon angioplasty - infant and children (<8yrs/25kg), feasible anatomy, n=14 Indications for stenting of CoAo • Patients > 8 yrs (> 25-30 kg) • No intracardiac lesion • Native CoAo or Recurrent CoA (post surgical or balloon) • Discrete or segmentar CoAo • Normal or hypoplasic isthmus • Mild CoA (SG < 20 mmHg) with left ventricular hypertrophy and/or systemic arterial hypertension Stent implantation (>8yrs/ 25 kg, feasible anatomy), n=10 Miscellaneous CoAo Miscellaneous CoAo Miscellaneous CoAo Results (2009-2014) Patients # 24 Male Female 17 (71%) 7 (29%) Age 2mo – 49y Treatment: Baloon Stent 14 (58%) 10 (42%) Mean PG (before interv.) Mean PG (after interv.) 56mmHg (35-85) 19mmHg (10-29) Isolated Combined (VSD, PDA) 19 (79%) 5 (21%) Complications 1 (4%) Our complications Case #1 Patient T.J., male, age 14y Presentation: headaches, ↑BP(190/120mmHg), ↓femoral pulse Echocardiography: Coarctation PG 50mmHg, LVH (IVS 16mm) Balloon predilatation (Tyshak 10/30mm); Bip Balloon 22/45mm 22P 8atm 16mm; stent CP8Z39 Case #2 Patient A.N., male, age 19y Presentation: asymptomatic ↑BP(160/100mmHg) Echocardiography: Coarctation PG 40mmHg, LVH (IVS 14mm) CP stent 8Zig 39mm; pre dilatation balloon Tyshak II 22/40mm Case #3 Patient N.N., female, age 49y Two years prior ACBPx1, ASD Closure + TKR; AFF; HTA; HLM Coarctatation PG 40mmHg Covered CP stent 8 Zig 28mm, 18mm N.N. 49yrs. Summary and Follow-Up Class I 1. Lifelong cardiology follow-up is recommended for all patients with aortic coarctation, repaired or not. (Level of Evidence: C) 2. Patients with surgical repair or percutaneous intervention for coarctation should have at least yearly followup. (Level of Evidence: C) 3. Late postoperative thoracic aortic imaging should be performed to assess for aortic dilatation or aneurysm formation for all pts. (Level of Evidence: B) 4. Patients should be observed closely for systemic arterial hypertension, which should be treated aggressively after recoarctation is excluded. (Level of Evidence:B) 5. Evaluation of the coarctation repair site by MRI/CT should be performed at intervals of 5 years or less (Level of Evidence: C) Class IIb 1. Routine exercise testing may be performed at intervals determined by consultation with the regional ACHD center. (Level of Evidence: C) ACC/AHA 2008 Guidelines for Adults With CHD Best option for patient, MD and hospitals Age >8yrs/25 kg Good anatomy No concomitant lesions Stenting of aorta Thanks for your attention