* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Slide Set - Professional Heart Daily
Saturated fat and cardiovascular disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Coronary artery disease wikipedia , lookup
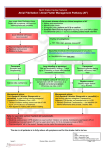
AHA/ASA Guideline Guidelines for the Prevention of Stroke in Patients With Stroke or Transient Ischemic Attack: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. The American Association of Neurological Surgeons and Congress of Neurological Surgeons have reviewed this document and affirm its educational content. ©2010 American Heart Association, Inc. All rights reserved. Writing Committee Karen L. Furie, MD, MPH, FAHA, Chair Scott E. Kasner, MD, MSCE, FAHA, Vice Chair • • • • • • • • Robert J. Adams, MD, MS, FAHA Gregory W. Albers, MD Ruth L. Bush, MD, MPH Susan C. Fagan, PharmD, FAHA Jonathan L. Halperin, MD, FAHA S. Claiborne Johnston, MD, PhD Irene Katzan, MD, MS, FAHA Walter N. Kernan, MD • • • • • • • • Pamela H. Mitchell, PhD, CNRN, RN, FAAN, FAHA Bruce Ovbiagele, MD, MS, FAHA Yuko Y. Palesch, PhD Ralph L. Sacco, MD, MS, FAHA, FAAN Lee H. Schwamm, MD, FAHA Sylvia Wassertheil-Smoller, MD, PhD, FAHA Tanya N. Turan, MD, FAHA Deidre Wentworth, MSN, RN On behalf of the American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Clinical Cardiology; and Interdisciplinary Council on Quality of Care and Outcomes Research ©2010 American Heart Association, Inc. All rights reserved. Slide Set developed by: Karen Furie, MD Dawn Kleindorfer, MD Anne Leonard, MPH, RN, CCRC, FAHA ©2010 American Heart Association, Inc. All rights reserved. Definition of Classes and Levels of Evidence Used in AHA Recommendations Class I Conditions for which there is evidence for and/or general agreement that the procedure or treatment is useful and effective. Class II Conditions for which there is conflicting evidence and/or a divergence of opinion about the usefulness/efficacy of a procedure or treatment. Class IIa The weight of evidence or opinion is in favor of the procedure or treatment. Class Iib Usefulness/efficacy is less well established by evidence or opinion. Class III Conditions for which there is evidence and/or general agreement that the procedure or treatment is not useful/effective and in some cases may be harmful. Therapeutic Recommendations Level of Evidence A Data derived from multiple randomized clinical trials or meta-analyses Level of Evidence B Data derived from a single randomized trial or nonrandomized studies Level of Evidence C Consensus opinion of experts, case studies, or standard of care Diagnostic Recommendations Level of Evidence A Data derived from multiple prospective cohort studies using a reference standard applied by a masked evaluator Level of Evidence B Data derived from a single grade A study, or one or more case-control studies, or studies using a reference standard applied by an unmasked evaluator Level of Evidence C Consensus opinion of experts ©2010 American Heart Association, Inc. All rights reserved. Hypertension as a Risk Factor for Recurrent Stroke • About 72 million Americans have hypertension, defined as >140/90 mm/Hg. • Meta-analysis of randomized controlled trials have demonstrated a 30%-40% reduction of stroke with blood pressure management. • Risk reduction is greater with larger reductions in BP. • From available data, the use of diuretics and ACEI are an important treatment option. • Individualization of treatment is important depending on the overall clinical picture. • Control of HTN the most modifiable risk factor to prevent stroke. ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Treatable Vascular Risk Factors Risk Factors Recommendation - Hypertension Class/Level of Evidence BP reduction is recommended for both prevention of recurrent stroke and prevention of other vascular events in persons who have had an ischemic stroke or TIA and are beyond the first 24 hours Class I; LOE A Because this benefit extends to persons with and without a documented history of hypertension, this recommendation is reasonable for all patients with ischemic stroke or TIA who are considered appropriate for BP reduction Class IIa; LOE B An absolute target BP level and reduction are uncertain and should be individualized, but benefit has been associated with an average reduction of approximately 10/5 mm Hg, and normal BP levels have been defined as <120/80 mm Hg by JNC 7 Class IIa; LOE B ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Treatable Vascular Risk Factors Risk Factors Recommendation - Hypertension Class/Level of Evidence Several lifestyle modifications have been associated with BP reduction and are a reasonable part of a comprehensive antihypertensive therapy. Class IIa; LOE C These modifications include salt restriction; weight loss; consumption of a diet rich in fruits, vegetables, and low-fat dairy products; regular aerobic physical activity; and limited alcohol consumption. The optimal drug regimen to achieve the recommended level of reduction is uncertain because direct comparisons between regimens are limited. The available data indicate that diuretics or the combination of diuretics and an ACEI are useful Class I; LOE A The choice of specific drugs and targets should be individualized on the basis of pharmacologic properties, mechanism of action, and consideration of specific patient characteristics for which specific agents are probably indicated (eg, extracranial cerebrovascular occlusive disease, renal impairment, cardiac disease, and diabetes) Class IIa; LOE B New Recommendation ©2010 American Heart Association, Inc. All rights reserved. Diabetes and Stroke Prevention • An estimated 8% of the US adult population is affected by diabetes. • The prevalence of diabetes in persons with stroke is about 15%-33%. • Diabetes is a risk factor for stroke, but its relationship to recurrent stroke is unclear. • Diabetes is a clear RF in persons with lacunar strokes. ©2010 American Heart Association, Inc. All rights reserved. Diabetes • Definitions: – Normal fasting blood glucose: <100mg/dL – Impaired fasting blood glucose: 100mg/dL-125mg/dL – Hyperglycemia – fasting plasma glucose level of >126mg/dL, or a casual plasma glucose of >200mg/dL along with other symptoms attributable to diabetes. – A hemoglobin A1c (HbA1c) level >7% -inadequate control of hyperglycemia – Diet, exercise, oral hypoglycemic drugs, and insulin are recommended for glycemic control. ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Treatable Vascular Risk Factors Risk Factors Recommendation - Diabetes Class/Level of Evidence Use of existing guidelines for glycemic control and BP targets in patients with diabetes is recommended for patients who have had a stroke or TIA Class I; LOE B New Recommendation ©2010 American Heart Association, Inc. All rights reserved. Blood lipids and Stroke Prevention • Epidemiological studies have shown a modest relationship between elevated total cholesterol or low-density lipoprotein cholesterol with an increased risk of ischemic stroke. • Recent studies have linked higher serum triglycerides to ischemic stroke and large artery atherosclerosis. • There has been a link between low-density lipoprotein and the occurrence of ICH. • Meta-analysis of trials including over 90,000 patients in statin trials showed that the larger reduction in LDL-C the larger the reduction in stroke. ©2010 American Heart Association, Inc. All rights reserved. SPARCL – Stroke Prevention by Aggressive Reduction in Cholesterol Levels • Important trial to establish the relationship between aggressive lowering of LDL-C and secondary prevention • 4371 persons with LDL-C = 100mg/dL-190mg/dL • Prior stroke or TIA, no hx of CHD • Randomized to 80 mg atorvastatin vs. placebo – Mean FUP 4.9 years – Endpoint: fatal and nonfatal stroke = 11.2% who received atorvastatin vs. 13.1% who received placebo, results: u u 5 yr absolute RR, 2.2%, HR 0.84; 85% CI (0.71 to 0.99; P=0.03) 5 yr absolute RR in cardiovascular events was 3.5% (HR, 0.80; 95% CI, 0.690.92; P=0.002). ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Treatable Vascular Risk Factors Risk Factors Recommendation - Lipids Class/Level of Evidence Statin therapy with intensive lipid-lowering effects is recommended to reduce risk of stroke and cardiovascular events among patients with ischemic stroke or TIA who have evidence of atherosclerosis, an LDL-C level ≥100 mg/dl, and who are without known CHD. Class I; LOE B For patients with atherosclerotic ischemic stroke or TIA and without known CHD, it is reasonable to target a reduction of at least 50% in LDL-C or a target LDL-C level of <70 mg/dL to obtain maximum benefit. Class IIa; LOE B New recommendation ACEI indicates angiotensin-converting enzyme inhibitor; BP, blood pressure; CHD, coronary heart disease; HDL, high-density lipoprotein cholesterol; JNC 7, The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; LDL-C, lowdensity lipoprotein cholesterol; NCEP III, The Third Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Cholesterol in Adults; SPARCL, Stroke Prevention by Aggressive Reduction in Cholesterol Levels; and TIA, transient ischemic attack. *See Tables 1 and 2 for explanation of class and level of evidence. ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Treatable Vascular Risk Factors Risk Factors Recommendations - Lipids Class/Level of Evidence Patients with ischemic stroke or TIA with elevated cholesterol or comorbid coronary artery disease should be otherwise managed according to NCEP III guidelines, which include lifestyle modification, dietary guidelines, and medication recommendations. Class I; LOE A Patients with ischemic stroke or TIA with low HDL-C may be considered for treatment with niacin or gemfibrozil. Class IIb; LOE B ACEI indicates angiotensin-converting enzyme inhibitor; BP, blood pressure; CHD, coronary heart disease; HDL, high-density lipoprotein cholesterol; JNC 7, The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; LDL-C, lowdensity lipoprotein cholesterol; NCEP III, The Third Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Cholesterol in Adults; SPARCL, Stroke Prevention by Aggressive Reduction in Cholesterol Levels; and TIA, transient ischemic attack. *See Tables 1 and 2 for explanation of class and level of evidence. ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Modifiable Behavioral Risk Factors Risk Factor Recommendation Class/Level of Evidence Cigarette smoking Healthcare providers should strongly advise every patient with stroke or TIA who has smoked in the past year to quit. Class I; LOE C It is reasonable to avoid environmental (passive) tobacco smoke . Class IIa; LOE C Counseling, nicotine products, and oral smoking cessation medications are effective for helping smokers to quit. Class I; LOE A Healthcare providers should strongly advise every patient with stroke or TIA who has smoked in the past year to quit. Class I; LOE C Counseling, nicotine products, and oral smoking cessation medications are effective for helping smokers to quit . Class I; LOE A ©2010 American Heart Association, Inc. All rights reserved. Alcohol Consumption • There is strong evidence that chronic alcoholism and heavy drinking are risk factors for stroke subtypes. • Most studies have suggested a J-shaped association between alcohol and ischemic stroke, with a protective effect from light to moderate consumption and an elevated risk of stroke with heavy consumption. • Majority of data on the risk of alcohol pertain to primary prevention (See AHA Primary Prevention of Stroke Guideline). • The mechanism for reduced risk of ischemic stroke with light to moderate consumption may be related to an increase in HDL, a decrease in platelet aggregation, and a lower concentration of plasma fibrinogen. • In heavy alcohol users, the mechanism may be related to increased blood pressure, hypercoagulable state, reduced cerebral blood flow, and AF or cardioembolism due to cardiomyopathy. ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Modifiable Behavioral Risk Factors Risk Factor Recommendation Class/Level of Evidence Alcohol consumption Patients with ischemic stroke or TIA who are heavy drinkers should eliminate or reduce their consumption of alcohol. Class I; LOE C Light to moderate levels of alcohol consumption (no more than 2 drinks per day for men and 1 drink per day for nonpregnant women) may be reasonable; nondrinkers should not be counseled to start drinking. Class IIb; LOE B ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Modifiable Behavioral Risk Factors Risk Factor Recommendation Class/Level of Evidence Physical Activity Class IIb; LOE C For patients with ischemic stroke or TIA who are capable of engaging in physical activity, at least 30 minutes of moderateintensity physical exercise, typically defined as vigorous activity sufficient to break a sweat or noticeably raise heart rate, 1 to 3 times a week (e.g., walking briskly, using an exercise bicycle) may be considered to reduce risk factors and comorbid conditions that increase the likelihood of recurrent stroke. For those individuals with a disability following ischemic stroke, supervision by a healthcare professional, such as a physical therapist or cardiac rehabilitation professional, at least on initiation of an exercise regimen, may be considered. ©2010 American Heart Association, Inc. All rights reserved. Class IIb; LOE C Metabolic Syndrome and Stroke • Refers to a constellation of several physiological abnormalities that increase the risk for vascular disease. – Hypertriglyceridemia, low HDL-C, high blood pressure, and hyperglycemia. – Expanded risks include subclinical inflammation and disorders of thrombosis, fibrinolysis and endothelial function (all may be genetic). – Commonly diagnosed using NCEP Adult Treatment Panel criteria (WHO and AHA have adopted these criteria). ©2010 American Heart Association, Inc. All rights reserved. Metabolic Syndrome AHA Definition • 3 out of 5 features present – Increased waist circumference (>102cm in men; >88cm in women) – Elevated triglycerides (>150mg/dL) – Reduced HDL-C (<50mg/dL in men; <40mg/dL in women) – Elevated BP >130/85mm/Hg – Elevated fasting glucose of >100mg/dL • Diet, exercise, and use of drugs that enhance insulin sensitivity have been shown improvements in persons with metabolic syndrome. ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Modifiable Behavioral Risk Factors Risk Factor Recommendation Class/Level of Evidence Metabolic Syndrome At this time, the utility of screening patients for the metabolic syndrome after stroke has not been established. Class IIb; LOE C New Recommendation For patients who are screened and classified as having the metabolic syndrome, management should include counseling for lifestyle modification (diet, exercise, and weight loss) for vascular risk reduction. Class I; LOE C New Recommendation Preventive care for patients with the metabolic syndrome should include appropriate treatment for individual components of the syndrome that are also stroke risk factors, particularly dyslipidemia and hypertension. Class I; LOE A New Recommendation TIA denotes Transient Ischemic Attack See Tables I and II for explanation of Class and Level of Evidence ©2010 American Heart Association, Inc. All rights reserved. Symptomatic Extracranial Carotid Disease • Several randomized and nonrandomized trials have compared surgical intervention (carotid endarterectomy- CEA) with best medical therapy alone. • Best medical therapy did not include use of HMG-CoA reductase inhibitors (statins), alternative antiplatelets (such as clopidogrel or sustained-release dipyridamole-aspirin), optimization of BP control, and smoking cessation therapy. • Surgical techniques have evolved. • Carotid angioplasty and stenting (CAS) have emerged as alternative treatments for stroke prevention in persons deemed at high risk for conventional endarterectomy. ©2010 American Heart Association, Inc. All rights reserved. Carotid Endarterectomy: Conventional Gold Standard Surgical Treatment Left image: High grade internal carotid artery stenosis, digital subtraction image, suggestive of ulceration. Right image: pathologic specimen of carotid artery plaque with thrombus. Prospective Trials Comparing Carotid Endarterectomy and Medical Therapy Trial ECST NASCET VACS Mean Follow-up Surgical Arm* Medical Arm* 3y 2.8% 16.8% 2.7 y 9% 26% 11.9 mo 7.9% 25.6% ECST indicates European Carotid Surgery Trial; NASCET, North American Symptomatic Carotid Endarterectomy Trial; and VACS, Veterans Affairs Cooperative Study Program. *Risk of fatal or nonfatal ipsilateral stroke. ©2010 American Heart Association, Inc. All rights reserved. Carotid Revascularization Endarterectomy vs. Stenting Trial (CREST) % Trial Design: Prospective, multicenter, randomized, controlled trial with blinded endpoint adjudication. Comparing carotid endarterectomy (CEA) and carotid artery stenting (CAS) in participants with symptomatic and asymptomatic stenosis. N = 2502. 108 US sites and 9 Canadian sites. Multidisciplinary research team: surgeon, research coordinator, interventionalist, and neurologist. Primary Endpoint: Any clinical stroke, myocardial infarction or death within the peri-procedural period plus occurrence of ipsilateral stroke going forward. Primary Endpoint HR = 1.11; 95% CI: 0.81-1.51 P=0.51 CAS CEA Other Results •. No difference in treatment effect according to symptomatic status (P=0.84) or sex (P=0.34). •The 4 yr rate of stroke or death was 6.4% with CAS and 4.7% with CEA (HR, 1.50; P= 0.03). •Rates in the symptomatic group, 8.0% for CAS and 6.4% for CEA (HR 1.37; P=0.14. •Rates in the asymptomatic group, 4.5% for CAS and 2.7% for CEA (HR= 1.86; P=0.07). •Components of the periprocedural rates were different: •Death – CAS = 0.7% vs. CEA 0.3%, P=0.18 •Stroke – CAS = 4.1% vs. CEA 2.3% , P= 0.01 •Myocardial infarction – CAS = 1.1% vs. CEA= 2.3%, P=0.03 Brott TG, Hobson RW et al. Stenting vs. Endarterectomy for Treatment of Carotid-Artery Stenosis.. N Engl J Med 363;1, July 2010 ©2010 American Heart Association, Inc. All rights reserved. CREST Hazard Ratio for CAS Versus CEA in 1321 Symptomatic Patients by Treatment Group Periprocedural HR (95% CI) 4-Year Study Period HR (95% CI) MI 0.45 (0.18-1.11) --- Any periprocedural stroke or postprocedural ipsilateral stroke 1.74 (1.02-2.98) 1.29 (0.84-1.98) Any periprocedural stroke, death, or postprocedural ipsilateral stroke 1.89 (1.11-3.21) 1.37 (0.90-2.09) Any periprocedural stroke, MI, death, or postprocedural ipsilateral stroke 1.26 (0.81-1.96) 1.08 (0.74-1.59) CAS indicates carotid angioplasty and stenting; CEA, carotid endarectomy; CI, confidence interval; HR, hazard ratio; and MI, myocardial infarction. ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Interventional Approaches to Patients With Stroke Caused by Large-Artery Atherosclerotic Disease Risk Factor – Symptomatic Extracranial Carotid Disease Recommendations Class/Level of Evidence For patients with recent TIA or ischemic stroke within the past 6 months and ipsilateral severe (70% to 99%) carotid artery stenosis, CEA is recommended if the perioperative morbidity and mortality risk is estimated to be <6%. Class I; LOE A For patients with recent TIA or ischemic stroke and ipsilateral moderate (50% to 69%) carotid stenosis, CEA is recommended depending on patient-specific factors such as age, sex, and comorbidities if the perioperative morbidity and mortality risk is estimated to be <6%. Class I; LOE B When the degree of stenosis is <50%, there is no indication for carotid revascularization by either CEA or CAS. Class III; LOE A ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Interventional Approaches to Patients With Stroke Caused by Large-Artery Atherosclerotic Disease Risk Factor – Symptomatic Extracranial Carotid Disease Recommendations Class/Level of Evidence When CEA is indicated for patients with TIA or stroke, surgery within 2 weeks is reasonable rather than delaying surgery if there are no contraindications to early revascularization. Class IIa; LOE B CAS is indicated as an alternative to CEA for symptomatic patients at average or low risk of complications associated with endovascular intervention when the diameter of the lumen of the internal carotid artery is reduced by >70% by noninvasive imaging or >50% by catheter angiography. Class I; LOE B ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Interventional Approaches to Patients With Stroke Caused by Large- Artery Atherosclerotic Disease Risk Factor – Symptomatic Extracranial Carotid Disease Recommendations Class/Level of Evidence Among patients with symptomatic severe stenosis (>70%) in whom the stenosis is difficult to access surgically, medical conditions are present that greatly increase the risk for surgery, or when other specific circumstances exist, such as radiationinduced stenosis or re-stenosis after CEA, CAS may be considered. Class IIb; LOE B CAS in the above setting is reasonable when performed by operators with established periprocedural morbidity and mortality rates of 4% to 6%, similar to those observed in trials of CEA and CAS. Class IIa; LOE B For patients with symptomatic extracranial carotid occlusion, EC/IC bypass surgery is not routinely recommended. Class III; LOE A Optimal medical therapy, which should include antiplatelet therapy, statin therapy, and risk factor modification, is recommended for all patients with carotid artery stenosis and a TIA or stroke as outlined elsewhere in this guideline. Class I; LOE B New Recommendation ©2010 American Heart Association, Inc. All rights reserved. Extracranial Vertebrobasilar Disease • Persons with occlusive disease of the proximal and cervical portions of the vertebral artery (VA) are at relatively high risk for posterior or vertebrobasilar circulation ischemia. • Symptomatic VA stenosis carries a high recurrent risk in the first 7 days after symptoms onset than patients with recently symptomatic carotid stenosis. • Best medical therapy for these patients is unclear, and the role of invasive treatment remains uncertain. • There are few randomized trials providing evidence how to treat this disease. ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Interventional Approaches to Patients With Stroke Caused by Large-Artery Atherosclerotic Disease Risk Factor – Extracranial Vertebral Disease Recommendations Class/Level of Evidence Optimal medical thereapy, which should include antiplatelet therapy, statin therapy, and risk factor modification, is recommended for all patients with vertebral artery stenosis and a TIA or stroke as outlined elsewhere in the guideline. Class I; LOE B Endovascular and surgical treatment of patients with extracranial vertebral stenosis may be considered when patients are having symptoms despite optimal medical treatment (including antithrombotics, statins, and relevant risk factor control). Class IIb; LOE C ©2010 American Heart Association, Inc. All rights reserved. Intracranial Atherosclerosis • Patients with symptomatic intracranial atherosclerosis are at high risk of subsequent stroke. • The WASID study enrolled 569 patients with stroke or TIA resulting from intracranial stenoses of the MCA, intracranial internal carotid artery, intracranial vertebral artery, or basilar artery. – Randomized to aspirin 1300mg or warfarin (target INR of 2.0-3.0). – This study was stopped early due to safety issues in the warfarin arm. – Results: no significant difference between groups in terms of the primary endpoint (ischemic stroke, brain hemorrhage and vascular death: HR, warfarin vs. aspirin, 0.96; 95% CI, 0.68 to 1.37). ©2010 American Heart Association, Inc. All rights reserved. WASID Continued – There was more bleeding in the warfarin arm. – In the first year after the initial event the overall risk of recurrent stroke was 15% and the risk of stroke in the territory of the stenosis was 12%. – For patients with stenosis of > 70% the 1-yr risk of stroke in the territory of the stenotic artery was 19%. • Multivariate analysis = risk of stroke in the symptomatic vascular territory was highest for a stenosis >70%, and in patients enrolled early <17 days after the initial event. • Women were at increased risk. ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Interventional Approaches to Patients With Stroke Caused by Large-Artery Atherosclerotic Disease Risk Factor – Intracranial Atherosclerosis Recommendations Class/Level of Evidence For patients with a stroke or TIA due to 50% to 99% stenosis of a major intracranial artery, aspirin is recommended in preference to warfarin. Patients in the WASID trial were treated with aspirin 1,300 mg/d, but the optimal dose of aspirin in this population has not been determined. On the basis of the data on general safety and efficacy, aspirin doses of 50 mg/d to 325 mg/d are recommended. Class I, LOE B For patients with stroke or TIA due to 50% to 99% stenosis of a major intracranial artery, long-term maintenance of BP <140/90 mm Hg and total cholesterol level <200 mg/dL may be reasonable. Class IIb; LOE B New recommendation For patients with stroke or TIA due to 50% to 99% stenosis of a major intracranial artery, the usefulness of angioplasty and/or stent placement is unknown and is considered investigational. Class IIb; LOE C New recommendation For patients with stroke or TIA due to 50% to 99% stenosis of a major intracranial artery, EC/IC bypass surgery is not recommended. Class III; LOE B New recommendation New Recommendations CAS indicates carotid angioplasty and stenting; CEA, carotid endarterectomy; EC/IC, extracranial-intracranial; and TIA, transient ischemic attack. *See Tables 1 and 2 for explanation of class and level of evidence. ©2010 American Heart Association, Inc. All rights reserved. Atrial Fibrillation and Stroke • Both persistent and paroxysmal Afib are potent risk factors for first and recurrent stroke. • >75,000 stroke cases are attributed to Afib each year. • It is estimated that over 2 million persons have Afib in the US. • The leading arrhythmia in the elderly. • Multiple clinical trials have demonstrated the superiority of warfarin vs. placebo in preventing stroke. ©2010 American Heart Association, Inc. All rights reserved. • Irregularly irregular rhythm. • Sometimes with a rapid ventricular response. Recommendations for Patients With Cardioembolic Stroke Types Risk Factor – Atrial Fibrillation Class/Level of Evidence For patients with ischemic stroke or TIA with paroxysmal (intermittent) or permanent AF, anticoagulation with a vitamin K antagonist (target INR 2.5; range, 2.0 to 3.0) is recommended. Class I; LOE A For patients unable to take oral anticoagulants, aspirin alone is recommended. Class I; LOE A The combination of clopidogrel plus aspirin carries a risk of bleeding similar to that of warfarin and therefore is not recommended for patients with a hemorrhagic contraindication to warfarin. Class III; LOE B New Recommendation For patients with AF at high risk for stroke (stroke or TIA within 3 months, CHADS2 score of 5 or 6, mechanical valve or rheumatic valve disease) who require temporary interruption of oral anticoagulation, bridging therapy with an LMWH administered subcutaneously is reasonable. Class IIa; LOE C New Recommendation ©2010 American Heart Association, Inc. All rights reserved. Acute MI and LV Thrombus • In the absence of acute reperfusion therapy, intracardiac thrombi occurs in about 1/3 of patients in the first 2 weeks after anterior MI and in higher rates in those with large infarcts involving the LV apex. • Cerebral infarcts occur in about 10% of patients with LV thrombus in the absence of anticoagulation therapy. • Ventricular mural thrombi occur in patients with chronic ventricular dysfunction resulting from CAD, hypertension, or other dilated cardiomyopathy. • These are at persistent risk of stroke and systemic embolism whether or not AF is documented. ©2010 American Heart Association, Inc. All rights reserved. Acute MI and LV Thrombus • On the basis of available clinical trial results, Class I recommendations have advised oral anticoagulation of patients with echocardiographically detected LV thrombi after AMI. • No consensus regarding duration of anticoagulant treatment. • Stroke risk persists several months after MI. • The risk of thromboembolism seems to decrease after the first 3 months. • In patients with chronic ventricular aneurysm, the risk of embolism is fairly low, even through intracardiac thrombi occur frequently in this condition. ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Patients With Cardioembolic Stroke Types Risk Factor – Acute MI and LV Thrombus Class/Level of Evidence Patients with ischemic stroke or TIA in the setting of acute MI complicated by LV mural thrombus formation identified by echocardiography or another cardiac imaging technique should be treated with oral anticoagulation (target INR 2.5; range 2.0 to 3.0) for at least 3 months. Class I; LOE B ©2010 American Heart Association, Inc. All rights reserved. Cardiomyopathy • About 10% of patients with ischemic stroke have an LVEF of <30%. • Optimal stroke prevention in certain conditions is not known. • The Warfarin and Antiplatelet Therapy in Chronic Heart Failure trial (WATCH), a randomized trial, was terminated without adequate power to define the effect of warfarin compared with aspirin or clopidogrel on stroke. • The ongoing Warfarin vs. Aspirin in Reduced Cardiac Ejection Fraction (WARCEF) is designed to compare the efficacy of warfarin (INR 2.5-3.0) and aspirin (325mg daily). – Composite endpoint of death or stroke (ischemic or hemorrhagic) in patients with LVEF <35% without documented AF, mechanical heart valves, or other indication for anticoagulant therapy. ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Patients With Cardioembolic Stroke Types Risk Factor – Cardiomyopathy Class/Level of Evidence In patients with prior stroke or transient cerebral ischemic attack in sinus rhythm who have cardiomyopathy characterized by systolic dysfunction (LVEF 35%), the benefit of warfarin has not been established. Class IIb; LOE B New recommendation Warfarin (INR 2.0 to 3.0), aspirin (81 mg daily), clopidogrel (75 mg daily), or the combination of aspirin (25 mg twice daily) plus extended-release dipyridamole (200 mg twice daily) may be considered to prevent recurrent ischemic events in patients with previous ischemic stroke or TIA and cardiomyopathy. Class IIb; LOE B ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Patients With Cardioembolic Stroke Types Risk Factor – Native Valvular Heart Disease Class/Level of Evidence For patients with ischemic stroke or TIA who have rheumatic mitral valve disease, whether or not AF is present, long-term warfarin therapy is reasonable with an INR target range of 2.5 (range, 2.0 to 3.0). Class IIa; LOE C To avoid additional bleeding risk, antiplatelet agents should not be routinely added to warfarin. Class III; LOE C For patients with ischemic stroke or TIA and native aortic or nonrheumatic mitral valve disease who do not have AF, antiplatelet therapy may be reasonable. Class IIb; LOE C For patients with ischemic stroke or TIA and mitral annular calcification, antiplatelet therapy may be considered. Class IIb; LOE C For patients with MVP who have ischemic stroke or TIA, long-term antiplatelet therapy may be considered. Class IIb; LOE C ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Patients With Cardioembolic Stroke Types Risk Factor – Prosthetic Heart Valves Class/Level of Evidence For patients with ischemic stroke or TIA who have mechanical prosthetic heart valves, warfarin is recommended with an INR target of 3.0 (range, 2.5 to 3.5). Class I; LOE B For patients with mechanical prosthetic heart valves who have an ischemic stroke or systemic embolism despite adequate therapy with oral anticoagulants, aspirin 75 mg/d to 100 mg/d in addition to oral anticoagulants and maintenance of the INR at a target of 3.0 (range, 2.5 to 3.5) is reasonable if the patient is not at high bleeding risk (e.g., history of hemorrhage, varices, or other known vascular anomalies conveying increased risk of hemorrhage, coagulopathy). Class IIa; LOE B For patients with ischemic stroke or TIA who have bioprosthetic heart valves with no other source of thromboembolism, anticoagulation with warfarin (INR 2.0 to 3.0) may be considered. Class IIb; LOE C AF indicates atrial fibrillation; INR, international normalized ratio; LMWH, low-molecular-weight heparin; LV, left ventricular; LVEF, left ventricular ejection fraction; MVP, mitral valve prolapse; and TIA, transient ischemic attack. *See Tables 1 and 2 for explanation of class and level of evidence ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Antithrombotic Therapy for Noncardioembolic Stroke or TIA (Oral Anticoagulant and Antiplatelet Therapies) Class/Level of Evidence For patients with noncardioembolic ischemic stroke or TIA, the use of antiplatelet agents rather than oral anticoagulation is recommended to reduce risk of recurrent stroke and other cardiovascular events. Class I; LOE A Aspirin (50 mg/d to 325 mg/d) monotherapy, the combination of aspirin 25 mg and extended-release dipyridamole 200 mg twice daily, and clopidogrel 75 mg monotherapy are all acceptable options for initial therapy. The selection of an antiplatelet agent should be individualized on the basis of patient risk factor profiles, cost, tolerance, and other clinical characteristics. Class I; LOE A Class I; LOE B The addition of aspirin to clopidogrel increases risk of hemorrhage and is not recommended for routine secondary prevention after ischemic stroke or TIA. Class III; LOE A For patients allergic to aspirin, clopidogrel is reasonable. Class IIa; LOE C For patients who have an ischemic stroke while taking aspirin, there is no evidence that increasing the dose of aspirin provides additional benefit. Although alternative antiplatelet agents are often considered, no single agent or combination has been studied in patients who have had an event while receiving aspirin. Class IIb; LOE C ©2010 American Heart Association, Inc. All rights reserved. Class IIa; LOE B Recommendations for Stroke Patients With Other Specific Conditions Risk Factor - Arterial Dissections Class/Level of Evidence For patients with ischemic stroke or TIA and extracranial carotid or vertebral arterial dissection, antithrombotic treatment for at least 3 to 6 months is reasonable. Class IIa; LOE B The relative efficacy of antiplatelet therapy compared with anticoagulation is unknown for patients with ischemic stroke or TIA and extracranial carotid or vertebral arterial dissection. Class IIb; LOE B New Recommendation For patients with stroke or TIA and extracranial carotid or vertebral arterial dissection who have definite recurrent cerebral ischemic events despite optimal medical therapy, endovascular therapy (stenting) may be considered. Class IIb; LOE C Patients with stroke or TIA and extracranial carotid or vertebral arterial dissection who fail or are not candidates for endovascular therapy may be considered for surgical treatment. Class IIb; LOE C ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Stroke Patients With Other Specific Conditions Risk Factor - Patent Foreman Ovale Class/Level of Evidence For patients with an ischemic stroke or TIA and a PFO, antiplatelet therapy is reasonable. Class IIa; LOE B There are insufficient data to establish whether anticoagulation is equivalent or superior to aspirin for secondary stroke prevention in patients with PFO. Class IIb; LOE B New Recommendation There are insufficient data to make a recommendation regarding PFO closure in patients with stroke and PFO. Class IIb; LOE C ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Stroke Patients With Other Specific Conditions Risk Factor - Hyperhomocysteinemia Class/Level of Evidence Although folate supplementation reduces levels of homocysteine and may be considered for patients with ischemic stroke and hyperhomocysteinemia, there is no evidence that reducing homocysteine levels prevents stroke recurrence. Class IIb; LOE B ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Stroke Patients With Other Specific Conditions Risk Factor - Inherited Thrombophilias Class/Level of Evidence Patients with arterial ischemic stroke or TIA with an established inherited thrombophilia should be evaluated for DVT, which is an indication for short- or longterm anticoagulant therapy depending on the clinical and hematological circumstances. Class I; LOE A Patients should be fully evaluated for alternative mechanisms of stroke. In the absence of venous thrombosis in patients with arterial stroke or TIA and a proven thrombophilia, either anticoagulant or antiplatelet therapy is reasonable. Class IIa; LOE C For patients with spontaneous cerebral venous thrombosis and/or a history of recurrent thrombotic events and an inherited thrombophilia, long-term anticoagulation is probably indicated. Class IIa; LOE C ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Stroke Patients With Other Specific Conditions Risk Factor – APL Antibodies Class/Level of Evidence For patients with cryptogenic ischemic stroke or TIA in whom an APL antibody is detected, antiplatelet therapy is reasonable. Class IIa; LOE B For patients with ischemic stroke or TIA who meet the criteria for the APL antibody syndrome, oral anticoagulation with a target INR of 2.0 to 3.0 is reasonable. Class IIa; LOE B ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Stroke Patients With Other Specific Conditions Risk Factor – Sickle Cell Disease Class/Level of Evidence For adults with SCD and ischemic stroke or TIA, the general treatment recommendations cited above are reasonable with regard to control of risk factors and the use of antiplatelet agents. Class IIa; LOE B Additional therapies that may be considered to prevent recurrent cerebral ischemic events in patients with SCD include regular blood transfusions to reduce hemoglobin S to <30% to 50% of total hemoglobin, hydroxyurea, or bypass surgery in cases of advanced occlusive disease. Class IIb; LOE C ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Stroke Patients With Other Specific Conditions Risk Factor – Cerebral Venous Sinus Thrombosis Class/Level of Evidence Anticoagulation is probably effective for patients with acute CVT. Class IIa; LOE B In the absence of trial data to define the optimal duration of anticoagulation for acute CVT, it is reasonable to administer anticoagulation for at least 3 months followed by antiplatelet therapy. Class IIa; LOE C ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Stroke Patients With Other Specific Conditions Risk Factor – Fabry Disease Class/Level of Evidence For patients with ischemic stroke or TIA and Fabry disease, alpha-galactosidase enzyme replacement therapy is recommended. Class I; LOE B New Recommendation Other secondary prevention measures as outlined elsewhere in this guideline are recommended for patients with ischemic stroke or TIA and Fabry disease. Class I; LOE C New Recommendation ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Stroke Patients With Other Specific Conditions Risk Factor – Pregnancy Class/Level of Evidence For pregnant women with ischemic stroke or TIA and high-risk thromboembolic conditions such as hypercoagulable state or mechanical heart valves, the following options may be considered: adjusted-dose UFH throughout pregnancy, for example, a subcutaneous dose every 12 hours with monitoring of activated partial thromboplastin time; adjusted-dose LMWH with monitoring of anti-factor Xa throughout pregnancy; or UFH or LMWH until week 13, followed by warfarin until the middle of the third trimester and reinstatement of UFH or LMWH until delivery. Class IIb; LOE C In the absence of a high-risk thromboembolic condition, pregnant women with stroke or TIA may be considered for treatment with UFH or LMWH throughout the first trimester, followed by low-dose aspirin for the remainder of the pregnancy. Class IIb; LOE C ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Stroke Patients With Other Specific Conditions Risk Factor – Postmenopausal Hormone Replacement Therapy Class/Level of Evidence For women who have had ischemic stroke or TIA, postmenopausal hormone therapy (with estrogen with or without a progestin) is not recommended. Class III; LOE A ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Stroke Patients With Other Specific Conditions Risk Factor - Use of Anticoagulation after Intracranial Hemorrhage Class/Level of Evidence For patients who develop ICH, SAH, or SDH, it is reasonable to discontinue all anticoagulants and antiplatelets during the acute period for at least 1 to 2 weeks and reverse any warfarin effect with fresh frozen plasma or prothrombin complex concentrate and vitamin K immediately. Class IIa; LOE B Protamine sulfate should be used to reverse heparin-associated ICH, with the dose depending on the time from cessation of heparin. Class I; LOE B New Recommendation ©2010 American Heart Association, Inc. All rights reserved. Recommendations for Stroke Patients With Other Specific Conditions Risk Factor - Use of Anticoagulation after Intracranial Hemorrhage Class/Level of Evidence The decision to restart antithrombotic therapy after ICH related to antithrombotic therapy depends on the risk of subsequent arterial or venous thromboembolism, risk of recurrent ICH, and overall status of the patient. For patients with a comparatively lower risk of cerebral infarction (e.g., AF without prior ischemic stroke) and a higher risk of amyloid angiopathy (eg, elderly patients with lobar ICH) or with very poor overall neurological function, an antiplatelet agent may be considered for prevention of ischemic stroke. Class IIb; LOE B New Recommendation In patients with a very high risk of thromboembolism in whom restarting warfarin is considered, it may be reasonable to restart warfarin at 7 to 10 days after onset of the original ICH. For patients with hemorrhagic cerebral infarction, it may be reasonable to continue anticoagulation, depending on the specific clinical scenario and underlying indication for anticoagulant therapy . ©2010 American Heart Association, Inc. All rights reserved. Class IIb; LOE C Recommendations for Stroke Patients With Other Specific Conditions Special Approaches to Implementing Guidelines and their Use in High-Risk Populations Class/Level of Evidence It can be beneficial to embed strategies for implementation within the process of guideline development and distribution to improve utilization of the recommendations. Class IIa; LOE B New Recommendation Intervention strategies can be useful to address economic and geographic barriers to achieving compliance with guidelines and to emphasize the need for improved access to care for the aged, underserved, and high-risk ethnic populations. Class IIa; LOE B New Recommendation APL indicates antiphospholipid; CVT, cerebral venous thrombosis; DVT, deep vein thrombosis; ICH, intracerebral hemorrhage; LMWH, low-molecular-weight heparin; PFO, patent foramen ovale; SAH, subarachnoid hemorrhage; SCD, sickle cell disease; SDH, subdural hematoma; TIA, transient ischemic attack; and UFH, unfractionated heparin. *See Tables 1 and 2 for explanation of class and level of evidence. ©2010 American Heart Association, Inc. All rights reserved. Conclusions • Update to the 2008 Guidelines • Several new recommendations (Glycemic control, metabolic syndrome, endovascular intervention for carotid artery stenosis, atrial fibrillation) • Secondary prevention important to reduce the number of recurrent strokes • Secondary Prevention Guidelines are critical to hospitals who are primary stroke center certified – These guidelines offer evidence-based and best practice recommendations. ©2010 American Heart Association, Inc. All rights reserved.