* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Prognostic Value of a Novel Classification Scheme for Heart Failure
Saturated fat and cardiovascular disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Rheumatic fever wikipedia , lookup
Heart failure wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
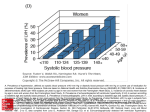
American Journal of Epidemiology Copyright ª 2006 by the Johns Hopkins Bloomberg School of Public Health All rights reserved; printed in U.S.A. Vol. 164, No. 2 DOI: 10.1093/aje/kwj168 Advance Access publication May 17, 2006 Practice of Epidemiology Prognostic Value of a Novel Classification Scheme for Heart Failure: The Minnesota Heart Failure Criteria Joseph Kim1,2, David R. Jacobs, Jr.2,3, Russell V. Luepker2, Eyal Shahar2, Karen L. Margolis4, and Mark P. Becker5 1 Medical Statistics Unit, London School of Hygiene and Tropical Medicine, University of London, London, United Kingdom. Division of Epidemiology and Community Health, School of Public Health, University of Minnesota, Minneapolis, MN. 3 Department of Nutrition, Faculty of Medicine, University of Oslo, Oslo, Norway. 4 Berman Center for Outcomes and Clinical Research, Minneapolis, MN. 5 Office of the Provost, University of South Carolina, Columbia, SC. 2 Received for publication August 11, 2004; accepted for publication January 25, 2006. The authors present the Minnesota Heart Failure Criteria (MHFC), derived using latent class analysis from widely available items in the Framingham Criteria. The authors used 1995 and 2000 data on hospitalized Minnesota Heart Survey subjects discharged after myocardial infarction or heart failure (N ¼ 7,379). Selected Framingham Criteria variables (dyspnea, pulmonary rales, cardiomegaly, interstitial or pulmonary edema on chest radiograph, S3 heart sound, tachycardia) plus left ventricular ejection fraction were used. The discriminatory power of the MHFC was evaluated using age- and sex-adjusted 2-year mortality. A five-class latent class analysis model was collapsed into cases and noncases. Mortality estimates discriminated noncases (18%) from cases (43%) (p < 0.001). The MHFC performed better than previous truncated criteria (Framingham Criteria: 26% noncases, 43% cases; Duke Criteria: 29%, 40%; Killip Score: 31%, 44%; Boston Score: 28%, 45%). In a subset of patients admitted for heart failure (n ¼ 5,128), the MHFC identified all but 2% (116/4,746) of cases found with a nearly full version of the Framingham Criteria. In terms of prognostic value, the MHFC are as precise as or more precise than several previous sets of truncated criteria. They closely approximate a nearly full version of the Framingham Criteria but require many fewer variables and can facilitate epidemiologic case-finding for heart failure. cardiovascular diseases; classification; diagnosis; heart diseases; heart failure, congestive; validation studies [publication type] Abbreviations: ICD-9, International Classification of Diseases, Ninth Revision; LCA, latent class analysis; LVEF, left ventricular ejection fraction; MHSAMI, Minnesota Heart Survey Acute Myocardial Infarction; MHSCHF, Minnesota Heart Survey Community Surveillance of Heart Failure. Heart failure is a major public health problem affecting over five million persons in the United States and over 23 million worldwide (1). The epidemiologic study of heart failure, however, has been partly impeded by the absence of a universally agreed-upon case definition (2–12). Though numerous case definitions have been introduced into the literature—primarily in the form of epidemiologic classifi- cation schemes (13–19)—most, if not all, of these criteria are based solely on a composite of signs and symptoms and ignore left ventricular ejection fraction (LVEF), a key index of underlying cardiac physiology for which there was limited data availability when the criteria were being developed (3, 5, 8, 20). In addition, existing criteria were evaluated using standard measures of validity (e.g., sensitivity and Correspondence to Dr. Joseph Kim, Medical Statistics Unit, Department of Epidemiology and Population Health, London School of Hygiene and Tropical Medicine, Keppel Street, London WC1E 7HT, United Kingdom (e-mail: [email protected]). 184 Am J Epidemiol 2006;164:184–193 Prognostic Value of the Minnesota Heart Failure Criteria specificity), all of which assume a perfect reference standard; given the absence of a diagnostic gold standard for heart failure, there is considerable uncertainty in the estimates of validity obtained for these criteria. In their original conception, the Framingham Criteria— arguably the most widely used epidemiologic criteria for heart failure—were defined by combining 17 ‘‘major’’ or ‘‘minor’’ heart-failure-related variables to form a diagnosis of heart failure in dichotomous categories (heart failure/no heart failure) (21). However, in practice, the Framingham Criteria are often implemented using only a subset of these variables, since data on many of the characteristics (e.g., circulation time) are no longer collected in routine clinical practice. It would therefore be of interest to evaluate the validity of a more abridged form of the criteria and compare this result with that of the original Framingham Criteria. Moreover, the incorporation of data on LVEF could enhance the classification process. We present a novel epidemiologic classification scheme for heart failure—the Minnesota Heart Failure Criteria— derived from widely available items used in the Framingham Criteria, employing latent class analysis (LCA), a probabilistic approach to disease classification which allows for and can potentially identify more precise categories of disease conditions. Validation of the Minnesota Heart Failure Criteria was performed under the assumption that persons with true cases of heart failure will have a higher risk of mortality than noncases in the 2 years following hospitalization. MATERIALS AND METHODS Study population The study included a population-based sample of patients whose records were abstracted as part of the Minnesota Heart Survey for the hospitalization discharge years 1995 and 2000. Patients were selected from two independent components of the Minnesota Heart Survey: the Acute Myocardial Infarction Study (22) and the Community Surveillance of Congestive Heart Failure Study (23). Acute myocardial infarction study. Patients selected for the Minnesota Heart Survey Acute Myocardial Infarction (MHSAMI) Study for the 1995 hospital discharge year were considered (22). Participants were residents of the Minneapolis-St. Paul, Minnesota, metropolitan area during 1995 and were between the ages of 30 and 74 years. Patients were hospitalized with an eligible International Classification of Diseases, Ninth Revision (ICD-9), discharge code for acute myocardial infarction (i.e., ICD-9 codes 410 and 411) in any of the participating regional acute-care hospitals. Trained nurses abstracted data on a 40 percent sample of men and an 80 percent sample of women. Relevant data on signs and symptoms, medical history, cardiac enzyme levels, clinical complications, therapy, and autopsy results were gathered. Congestive heart failure study. All patients in the Minnesota Heart Survey Congestive Heart Failure (MHSCHF) Study had an eligible ICD-9 discharge code for heart failure (i.e., ICD-9 code 428 or another heart-failure-related disAm J Epidemiol 2006;164:184–193 185 charge code) during 1995 or 2000 (23). Consistent with the MHSAMI, patients were residents of the MinneapolisSt. Paul metropolitan area at the time of the index hospitalization, but in MHSCHF they were between the ages of 35 and 84 years. Trained nurses abstracted data from 50 percent of all hospital discharges and gathered data on patient demographic factors, medical history, physical examination, electrocardiographic findings, chest radiography, and blood laboratory results and, where available, basic information on cardiac imaging (including current and historical LVEF) and cardiac catheterization. Combined data set. A combined data set was formed on the basis of MHSCHF data for 1995 and 2000 and MHSAMI data for 1995. The data were merged to broaden the spectrum of disease (with regard to both disease severity and type of heart failure) and to enhance the generalizability of the criteria. We hypothesized that the majority of noncases would arise from MHSAMI while the majority of cases would arise from MHSCHF. Statistical methods Development of the Minnesota Heart Failure Criteria. There are numerous methods by which a classification scheme for heart failure can be derived (13, 24). For this study, we chose LCA, an established method of categorical data analysis which has been used previously to validate diagnostic tests in the absence of a perfect reference standard (25–29). LCA is ideally suited for this purpose, because it makes no assumption about the independence of errors between the diagnostic test and the reference standard, which helps in avoiding the known problem of inflated validity estimates with the use of an imperfect reference standard (29, 30). LCA uses a nonlinear statistical model to classify groups of subjects who have shared characteristics into latent classes (e.g., diagnostic subgroups) (30, 31). It achieves this by maximizing a mathematical likelihood function based on the patients’ distributional pattern of signs, symptoms, and physiologic markers present at the time of evaluation. Given that the distribution of criterion variables is biologically relevant to the disease classification and there are sufficiently large numbers of cases and noncases to support these categorizations, LCA can identify the disease subcategories reliably. LCA is discussed further in other publications (28, 30–32) and in Web appendix 1, which is posted on the Journal’s website (http://www.aje.oxfordjournals.org). Variable selection. The variables defining the categories of heart failure were chosen on the basis of clinical relevance using the short Framingham Criteria, plus LVEF (table 1). They included dyspnea at rest or upon exertion, pulmonary rales, cardiomegaly, interstitial or pulmonary edema, the S3 heart sound, tachycardia (resting heart rate >120 beats/minute), and LVEF (<40 percent, 40 percent, or missing data). LCA model selection. A challenge of LCA is to choose the most appropriate number of latent classes using a parsimonious set of criterion variables. We set out to identify a plausible classification structure for heart failure with the fewest possible number of criterion variables. However, given the limited availability of variables in MHSAMI, we 186 Kim et al. TABLE 1. Sets of heart failure signs and symptoms compared with those of the Minnesota Heart Survey, 1995 and 2000 Existing criteria Heart failure sign or symptom Framingham Criteria (46) Duke Criteria (34) Killip Score (47) Dyspnea Pulmonary rales X Cardiomegaly X Acute pulmonary edema X S3 heart sound X Tachycardia (120 beats/minute) X Minnesota Heart Survey data sets Boston Score (19) MHSCHF* Study (n ¼ 5,128) Combined MHSAMI* data sety Study (n ¼ 2,251) (N ¼ 7,379) X Xz Xz Xz X§ X X X X{ X X X X X# X X** X** X X X X X X Xyy X X X X X X Paroxysmal nocturnal dyspnea X X X Orthopnea X X X X X Left ventricular ejection fraction percentage Neck vein distension X X Hepatojugular reflux X X Weight loss X X Ankle edema X X Hepatomegaly X Pleural effusion X Hypotension (systolic blood pressure <90 mmHg) X X X Night cough X Vital capacity (1/3 of maximum) X Increased venous pressure (>16 cm of water) X Circulation time 25 seconds X Venous hypertension X Peripheral vasoconstriction X X X Elevated jugular venous pressure X Wheezing X Upper zone flow X * MHSCHF, Minnesota Heart Survey Community Surveillance of Heart Failure; MHSAMI, Minnesota Heart Survey Acute Myocardial Infarction. y Pooled data from the MHSCHF and MHSAMI studies. z Dyspnea at rest or upon exertion. § Basilar or more than basilar rales. { Cardiomegaly on chest radiograph or cardiothoracic ratio 0.5. # Alveolar or interstitial pulmonary edema. ** Interstitial or pulmonary edema. yy Heart rate >110 beats/minute. opted to include all seven variables in the initial LCA model. We then compared the goodness of fit of this model with varying numbers of diagnostic classes. Nested models were evaluated through goodness-of-fit statistics: the Pearson chisquared (v2) test, the likelihood ratio chi-squared (L2) test, Akaike’s information criterion, and the Bayesian information criterion. All LCA models were fitted using Latent GOLD (version 2.0; Statistical Innovations, Belmont, Massachusetts) (33). Mortality comparison: LCA model versus previous truncated criteria. In the absence of a perfect gold standard, a diag- nostic test can be validated by comparing its results against a known consequence of the disease (34–37). Since a major predictable outcome of heart failure is short-term mortality (38–45), we hypothesized a priori that true heart failure cases would have a greater risk of mortality than noncases and that a positive deviation in mortality from noncases would reflect the discriminatory power of the criterion. Am J Epidemiol 2006;164:184–193 Prognostic Value of the Minnesota Heart Failure Criteria To this end, we fitted age- and sex-adjusted linear models to obtain absolute risk estimates of 2-year mortality for each LCA category. All-cause mortality, rather than heart-failure-specific mortality, was used to avoid possible misclassification resulting from death due to multisystem disease. We compared these estimates against those obtained similarly with sets of commonly used heart failure criteria (i.e., the Framingham Criteria (46), the Killip Score (47), the Duke Criteria (34), and the Boston Score (19)) which were adapted for use with data available in the Minnesota Heart Survey. The purpose here was to show the amount of additional information about the lethality of heart failure that is contained in a set of existing criteria, as a base for a similar examination of the LCA criteria. However, these results do not reflect the full potential of each criterion, since only those variables for which data are routinely collected in hospitals and are readily available in the Minnesota Heart Survey were used (referred to herein as ‘‘previous truncated criteria’’). In MHSCHF, it was possible to compute results for both a ‘‘short’’ set of Framingham Criteria (a six-item score based on widely available items) and a ‘‘long’’ set of Framingham Criteria (a 13-item score based on variables commonly assessed when evaluating possible heart failure) (table 1). It was only possible to compute results for the ‘‘short’’ Framingham Criteria in MHSAMI, since the collection of data on heart-failure-related variables was not part of the central aims of that study. Of the original 17 Framingham Criteria items (table 1), the long Framingham Criteria excluded factors that are not currently commonly assessed in patients being evaluated for possible heart failure: circulation time (25 seconds), increased venous pressure (>16 cm of water), vital capacity (1/3 of maximum), and night cough. To allow comparability with previous truncated criteria, LCA classes were collapsed into dichotomous disease categories (i.e., noncases and cases). We assessed possible interaction of the relation between diagnostic criteria and mortality with LVEF. All statistical analysis (excluding LCA) was performed using SAS for Windows (version 8.2; SAS Institute, Inc., Cary, North Carolina). RESULTS Development of the Minnesota Heart Failure Criteria We began by examining the prevalence of each criterion variable in all subjects, as well as in cases identified by the short Framingham Criteria separately for MHSAMI and MHSCHF (table 2). As expected, more subjects in MHSCHF than in MHSAMI presented with each of the seven heart failure criterion variables. Among cases identified by the short Framingham Criteria, pulmonary rales were less common in MHSAMI as compared with MHSCHF (40 percent vs. 95 percent), as were the S3 heart sound (9 percent vs. 22percent) and dyspnea(78 percentvs.93percent). MHSAMI subjects who fulfilled the short Framingham Criteria for heart failure more often had a high heart rate (30 percent vs. 16 percent) and pulmonary edema (77 percent vs. 55 percent). Am J Epidemiol 2006;164:184–193 187 The prevalences of cardiomegaly and low ejection fraction were similar between MHSCHF and MHSAMI. Bearing these differences in mind, we found that a fiveclass LCA model had a good fit to the observed data (Web appendix 1). The distributions of signs and symptoms by diagnostic class are shown in table 3. The LCA model shows that class 1 subjects had the lowest probability of presenting with the seven criterion variables: Few, if any, of these subjects had the S3 heart sound, interstitial or pulmonary edema, or tachycardia, though a relatively large proportion (40 percent) of subjects had dyspnea. Therefore, on the basis of the distributional pattern of conditional probabilities for the seven criterion variables, we labeled class 1 subjects ‘‘noncases.’’ In contrast, subjects in class 5 had the largest probability of presenting with a criterion variable: Nearly all of them had dyspnea, pulmonary rales, and cardiomegaly, while they also had the highest probability of presenting with depressed LVEF. Few subjects had the S3 heart sound in any other heart failure class, whereas over half of all class 5 subjects had the S3 heart sound. Therefore, we labeled these subjects as having ‘‘advanced heart failure.’’ Among the remaining classes, the distinctions were less clear: A defining feature of class 3 was that nearly all subjects had interstitial or pulmonary edema, in contrast to class 2, where only 1 percent of subjects had the sign. Among class 3 subjects, the presence of interstitial or pulmonary edema was consistent with a high prevalence of dyspnea and pulmonary rales. We hypothesized that subjects in classes 2, 3, and 4 had one form or another of ‘‘heart failure.’’ The prevalence of each diagnostic class (i.e., unconditional probability) is also shown in table 3. The ‘‘noncases’’ formed a large group comprising 28 percent (2,057/7,379) of the study population; the remaining 72 percent were classified as having some form of heart failure. The distribution of conditional probabilities and the consequent formation of the diagnostic classes were consistent with the population of origin: The ‘‘noncases’’ had the largest proportion derived from MHSAMI (84 percent), whereas nearly all subjects with ‘‘advanced heart failure’’ originated from MHSCHF. The majority of subjects with an LVEF under 40 percent originated from the MHSCHF data set: Only 32 percent of subjects in class 4 and 1 percent of subjects in class 5 were from MHSAMI. The posterior probabilities of diagnostic class membership for subjects with all signs and symptoms and a known LVEF (27, or 128 patterns), as well as those with missing data on LVEF (26, or 64 possible patterns), are shown in Web appendix 2 (http://www.aje.oxfordjournals.org). One hundred and fifty of the 192 possible response patterns were observed in our study population; we observed at least 10 patients in 82 categories. The response patterns listed in Web appendix 2, together with LCA class assignment based on their respective posterior probabilities, form the Minnesota Heart Failure Criteria. Application of the Minnesota Heart Failure Criteria in an epidemiologic setting is illustrated through an example: Suppose retrospectively abstracted medical records indicate that a subject had pulmonary rales, the S3 heart sound, interstitial or pulmonary edema, cardiomegaly, and dyspnea 188 Kim et al. TABLE 2. Distribution of heart failure signs and symptoms at the time of the index hospitalization, by data set, Minnesota Heart Survey, 1995 and 2000 All patients Heart failure sign/ symptom present? MHSAMIy Study (n ¼ 2,251) Heart failure cases only* MHSCHFy Study (n ¼ 5,128) No. % MHSAMI Study (n ¼ 253) MHSCHF Study (n ¼ 3,983) No. No. No. % % % No 1,209 54 461 9 55 22 264 7 Yes 1,042 46 4,667 91 198 78 3,719 93 2,115 94 762 15 151 60 190 5 136 6 4,366 85 102 40 3,793 95 1,577 70 1,423 28 42 17 540 14 674 30 3,705 72 211 83 3,443 86 1,993 89 2,911 57 57 23 1,806 45 258 11 2,217 43 196 77 2,177 55 2,219 99 4,242 83 231 91 3,116 78 32 1 886 17 22 9 867 22 2,122 94 4,473 87 177 70 3,356 84 129 6 655 13 76 30 627 16 No 906 40 1,297 25 64 25 1,023 26 Yes 323 14 1,735 34 104 41 1,435 36 1,022 45 2,096 41 85 34 1,525 38 Dyspnea Pulmonary rales No Yes Cardiomegaly on chest radiograph No Yes Interstitial or pulmonary edema No Yes S3 heart sound No Yes Heart rate >120 beats/minute No Yes Left ventricular ejection fraction <40% Missing data * Based on the short Framingham Criteria (six variables for which data were available in both studies). y MHSAMI, Minnesota Heart Survey Acute Myocardial Infarction; MHSCHF, Minnesota Heart Survey Community Surveillance of Heart Failure. but had missing data for LVEF. Web appendix 2 (observation number 187) would classify this person as belonging to class 5 with 74 percent certainty. With regard to risk stratification, we can further state that the person has advanced heart failure with a 53 percent risk of 2-year mortality. A simple SAS program that provides an algorithm for classifying people into the corresponding LCA categories based on the seven manifest variables for heart failure is downloadable from a University of Minnesota website (http:// www.epi.umn.edu/mhf). Mortality comparison: previous truncated criteria versus Minnesota Heart Failure Criteria The results shown in tables 4 and 5, when interpreted together, establish the discriminatory power of the Minnesota Heart Failure Criteria. Table 4 presents the 2-year mortality difference between labeled cases and noncases according to the previous truncated criteria (short Framingham Criteria: 26 percent noncases vs. 43 percent cases; Duke Criteria: 29 percent noncases vs. 40 percent cases; Killip Score: 31 percent noncases vs. 44 percent cases; Boston Score: 28 percent noncases vs. 45 percent cases). As compared with the previous truncated criteria, noncases identified by the Minnesota Heart Failure Criteria had the lowest mortality (18 percent), while cases had mortality equal to that of the short Framingham Criteria (43 percent) (p for difference < 0.001; table 5). Moreover, cases with advanced heart failure had a significantly greater risk of mortality than usual heart failure cases (47 percent vs. 42 percent; p ¼ 0.003). The difference in mortality between heart failure and advanced heart failure was greater in MHSAMI (33 percent heart failure vs. 53 percent advanced heart failure; p ¼ 0.067) than in MHSCHF (45 percent heart failure vs. 50 percent advanced heart failure; p ¼ 0.014), though the Am J Epidemiol 2006;164:184–193 Prognostic Value of the Minnesota Heart Failure Criteria previous truncated criteria (table 4), persons with a normal LVEF always had lower mortality than persons with a low LVEF, while those with a low LVEF and missing data had higher mortality. The lowest mortality was seen in noncases with normal LVEF (table 4); it equaled that of Minnesota Heart Failure Criteria noncases in the combined data set (table 5). In both tables, persons with missing data on LVEF always had an intermediate risk, and those noncases with a low LVEF performed as poorly as the cases. In addition, we found that the majority of persons in MHSAMI had a favorable mortality estimate (9 percent), while nearly all of the cases had an estimate comparable to that of the noncases in MHSCHF (33 percent) (table 5). Thus, the choice of using MHSAMI as the dominant source of noncases was appropriate, given that most subjects appeared to be free of heart failure and the variables required for performing LCA were easily accessible. TABLE 3. Marginal percentage of persons with heart failure symptoms, signs, and functional measures in each assigned latent class analysis class, ordered by the probability of occurrence in class 5, Minnesota Heart Survey, 1995 and 2000 Heart failure sign or symptom Dyspnea upon rest or exertion Pulmonary rales Latent class analysis class 1 2 3 4 5 40 98 96 58 99 4 81 93 39 99 Cardiomegaly 18 62 77 65 91 Left ventricular ejection fraction <40% 13 44 42 73 86 S3 heart sound 0 7 6 9 54 Interstitial or pulmonary edema 2 1 95 30 52 Heart rate >120 beats/minute 2 12 19 7 14 2,057 2,088 1,773 735 726 28 28 24 10 10 189 Prevalence of latent class No. of subjects % % of subjects from the Minnesota Heart Survey Acute Myocardial Infarction Study 84 8 6 32 Cross-classification of the Framingham Criteria and the Minnesota Heart Failure Criteria We found that the classification achieved using the Minnesota Heart Failure Criteria was remarkably consistent with the long Framingham Criteria, which approximate the full Framingham Criteria (see upper half of table 6). In MHSCHF, the two criteria agreed in 95 percent (4,848/ 5,128) of participants, including 218 noncases and 4,630 cases. These two criteria disagreed only in 5 percent (280/ 5,128) of all cases who had an ICD-9 heart-failure-related discharge code. Among the 280 discordant pairs (116 identified by the long Framingham Criteria but missed by the 1 statistical significance was marginal because there were only nine cases with advanced heart failure in MHSAMI. We also found that the discriminatory power of each criterion was modified by LVEF. Among cases identified by TABLE 4. Absolute risk of 2-year mortality* according to previous truncated criteria for heart failure, Minnesota Heart Survey, 1995 and 2000 Left ventricular ejection fraction Classification No. of subjects All patients (N ¼ 7,379) 40% (n ¼ 2,203) <40% (n ¼ 2,058) Missing data (n ¼ 3,118) ARz 95% CIz AR 95% CI AR 95% CI AR 95% CI p for interactiony Short Framingham Criteria§ No heart failure 3,143 0.26 0.25, 0.28 0.17 0.14, 0.19 0.42 0.38, 0.46 0.27 0.25, 0.29 Heart failure 4,236 0.43 0.42, 0.44 0.36 0.33, 0.38 0.48 0.45, 0.50 0.44 0.42, 0.46 No heart failure 2,836 0.29 0.28, 0.31 0.20 0.18, 0.23 0.42 0.38, 0.46 0.31 0.29, 0.34 Heart failure 4,543 0.40 0.39, 0.41 0.31 0.29, 0.33 0.47 0.45, 0.50 0.39 0.37, 0.41 No heart failure 4,490 0.31 0.29, 0.32 0.21 0.19, 0.23 0.44 0.41, 0.47 0.31 0.29, 0.33 Heart failure 2,889 0.44 0.42, 0.46 0.36 0.33, 0.39 0.48 0.45, 0.51 0.46 0.43, 0.48 No heart failure 3,975 0.28 0.27, 0.30 0.18 0.16, .021 0.43 0.40, 0.47 0.29 0.26, 0.31 Heart failure 3,404 0.45 0.43, 0.46 0.38 0.35, 0.41 0.48 0.45, 0.51 0.47 0.44, 0.49 <0.0001 Duke Criteria <0.0001 Killip Score <0.0001 Boston Score <0.0001 * The combined data set (pooled data from the Minnesota Heart Survey Community Surveillance of Heart Failure (MHSCHF) Study and the Minnesota Heart Survey Acute Myocardial Infarction (MHSAMI) Study) was used in the calculation of 2-year absolute risks, adjusted for age and sex. y Missing data on left ventricular ejection fraction were excluded from statistical testing. z AR, absolute risk; CI, confidence interval. § The short Framingham Criteria were based on six variables for which data were available in both the MHSCHF Study and the MHSAMI Study. Am J Epidemiol 2006;164:184–193 190 Kim et al. TABLE 5. Absolute risk of 2-year mortality* according to the Minnesota Heart Failure Criteria, Minnesota Heart Survey, 1995 and 2000 Left ventricular ejection fraction Classification No. of subjects All patients (N ¼ 7,379) ARz 95% CIz 40% (n ¼ 2,203) AR 95% CI <40% (n ¼ 2,058) AR 95% CI Missing data (n ¼ 3,118) AR p for interactiony 95% CI Combined data set § No heart failure (LCAz class 1) 2,057 0.18 0.16, 0.20 0.14 0.11, 0.17 0.36 0.29, 0.44 0.18 0.15, 0.21 Heart failure (overall) 5,322 0.43 0.41, 0.44 0.35 0.33, 0.38 0.47 0.45, 0.49 0.43 0.42, 0.45 4,596 0.42 0.41, 0.43 0.35 0.33, 0.38 0.46 0.44, 0.49 0.43 0.41, 0.45 726 0.47 0.44, 0.50 0.37 0.30, 0.45 0.49 0.45, 0.54 0.51 0.45, 0.58 Heart failure (LCA classes 2–4) Advanced heart failure (LCA class 5) <0.0001 Minnesota Heart Survey Community Surveillance of Heart Failure Study No heart failure (LCA class 1) Heart failure (overall) Heart failure (LCA classes 2–4) Advanced heart failure (LCA class 5) 334 0.35 0.30, 0.40 0.29 0.21, 0.38 0.41 0.28, 0.53 0.38 0.30, 0.46 4,794 0.46 0.45, 0.47 0.40 0.38, 0.43 0.49 0.46, 0.51 0.47 0.44, 0.49 4,077 0.45 0.44, 0.47 0.40 0.37, 0.43 0.48 0.45, 0.51 0.46 0.44, 0.48 717 0.50 0.46, 0.54 0.41 0.32, 0.50 0.50 0.46, 0.55 0.54 0.47, 0.62 <0.0001 Minnesota Heart Survey Acute Myocardial Infarction Study No heart failure (LCA class 1) Heart failure (overall) Heart failure (LCA classes 2–4) Advanced heart failure (LCA class 5) 1,723 0.09 0.07, 0.11 0.06 0.04, 0.08 0.28 0.19, 0.37 0.10 0.07, 0.12 528 0.33 0.30, 0.36 0.24 0.19, 0.30 0.37 0.31, 0.44 0.33 0.29, 0.37 519 0.33 0.30, 0.35 0.23 0.18, 0.29 0.36 0.30, 0.43 0.33 0.29, 0.38 9 0.53 0.31, 0.75 —{ 0.66 0.28, 1.04 —{ 0.0596 * The combined data set (pooled data from the Minnesota Heart Survey Community Surveillance of Heart Failure (MHSCHF) Study and the Minnesota Heart Survey Acute Myocardial Infarction (MHSAMI) Study) was used in the calculation of 2-year absolute risks, adjusted for age and sex. y Noncases vs. cases. The distinction between heart failure and advanced heart failure was ignored. Missing data on left ventricular ejection fraction were excluded from statistical testing. z AR, absolute risk; CI, confidence interval; LCA, latent class analysis. § Pooled data from the MHSCHF Study and the MHSAMI Study. { Insufficient data for calculation of parameter estimates. short Framingham Criteria; 164 identified only by the Minnesota Heart Failure Criteria), the proportions differently classified by the two sets of criteria and their mortality rates were similar; mortality estimates for the 280 subjects were higher than in the 218 mutually classified noncases, but not significantly so. The limitations of the short Framingham Criteria were apparent. No one was classified as a noncase by the Minnesota Heart Failure Criteria but as a case by the short Framingham Criteria. In contrast, 647 cases were missed by the Short Framingham Criteria; these cases had mortality (44 percent) equivalent to that of the 3,983 persons classified as cases by both the Minnesota Heart Failure Criteria and the long Framingham Criteria. The lower half of table 6 compares the Minnesota Heart Failure Criteria and the short Framingham Criteria in MHSAMI, where results for the long Framingham Criteria were not available. The two criteria agreed in 88 percent of participants (1,976/2,251), including 1,723 noncases and 253 cases. The cases had a 2-year risk of mortality that was equivalent to that of the MHSCHF cases identified by both the Minnesota Heart Failure Criteria and the long Framingham Criteria, while the noncases had substantially lower mortal- ity than the noncases in MHSCHF. A total of 275 cases misclassified as noncases by the short Framingham Criteria had significantly greater mortality (32 percent) than noncases, similar to the mortality risk in MHSCHF of noncases and cases for whom the Minnesota Heart Failure Criteria and the long Framingham Criteria disagreed. DISCUSSION In this study, we set out to derive a new classification scheme for heart failure that was suitable for epidemiology— specifically, one that could be useful for heart failure surveillance and mortality follow-up. We were cognizant in this endeavor that heart failure surveillance and case-finding, beyond potential cases already identified through physician diagnosis, would be unlikely to include the depth of relevant and decisive elements that the full Framingham Criteria call for. Thus, a more pragmatic classification scheme for heart failure is needed for epidemiologic research (especially if retrospective), and the LCA approach was intended to fill this gap. Am J Epidemiol 2006;164:184–193 Prognostic Value of the Minnesota Heart Failure Criteria TABLE 6. Absolute risk of 2-year mortalityy by heart failure classification in two different Minnesota Heart Survey data sets, 1995 and 2000 Heart failure present? Latent class analysisz Long Framingham Criteria§ Short Framingham Criteria{ (as a subset of the long Framingham Criteria) No. of subjects Mortality risk Minnesota Heart Survey Community Surveillance of Heart Failure Study (n ¼ 5,128 ) No No No 218 0.30 No Yes No 116 0.35 No Yes Yes Yes No No 164 Yes Yes No 647 0.44* Yes Yes Yes 3,983 0.44* 0 0.35 Minnesota Heart Survey Acute Myocardial Infarction Study (n ¼ 2,251)# No No No Yes 1,723 0.15 Yes No 275 0.32* Yes Yes 253 0.45* 0 * p < 0.0001 (compared with persons unanimously classified as noncases). y The 2-year mortality estimates shown were derived from ageand sex-adjusted linear models. z The five-class latent class analysis model was dichotomized for comparability (class 1 ¼ noncase; classes 2–5 ¼ heart failure case). § The long Framingham Criteria were based on 13 variables for which data were available in the Minnesota Heart Survey Community Surveillance of Heart Failure Study. { The short Framingham Criteria were based on six variables for which data were available in both the Minnesota Heart Survey Community Surveillance of Heart Failure Study and the Minnesota Heart Survey Acute Myocardial Infarction Study. # Results for the long Framingham Criteria could not be calculated because of missing data on some variables. The Minnesota Heart Failure Criteria were derived using LCA with six widely available items from the Framingham Criteria, plus LVEF, an important marker of underlying cardiac physiology that was not included in the Framingham Criteria. The best-fitting model was a five-class model, which was collapsed into three categories of risk strata (i.e., noncase, heart failure, and advanced heart failure). Using high 2-year mortality as a proxy for true cases of heart failure— which was reasonable given the high case fatality for heart failure—we showed that the LCA model provides better discrimination than the short Framingham Criteria and other previous truncated criteria considered in both patients hospitalized for congestive heart failure and patients hospitalized for acute myocardial infarction. Thus, the Minnesota Heart Failure Criteria may be a suitable substitute for the long Framingham Criteria in situations that may hide heart failure, such as cases of acute myocardial infarction and chronic obstructive pulmonary disease. The fact that the long Framingham Criteria are unAm J Epidemiol 2006;164:184–193 191 likely to be implementable in such hospital records reduces their value for general heart failure surveillance. The comparability of the Minnesota Heart Failure Criteria with the long Framingham Criteria is notable, given the contrasting mechanisms by which each set of criteria was derived: The Minnesota Heart Failure Criteria are based on a statistical model and maximum likelihood estimation, whereas the Framingham Criteria are based on clinical plausibility. We caution that we were only able to evaluate the value of a scheme using limited variables originally selected for classifying myocardial infarction, because of the restricted set of signs and symptoms available in MHSAMI. Therefore, there was no ‘‘control’’ group in the MHSCHF data set; rather, we used a comparison population in whom we thought heart failure would be relatively rare. Our data cannot confirm or firmly establish how well the previous truncated criteria would have performed had we had complete information on all of the required variables. Indeed, a study would have to be specially designed to obtain such a control set; this would probably be difficult, since very few patients without suspected heart failure are tested for the full set of 17 Framingham Criteria, and several of the original signs and symptoms are now rarely clinically assessed, even in patients suspected of having heart failure. Seen in this light, MHSAMI is a rich source for comparison with the MHSCHF data set, given that several critical heart failure signs and symptoms are included in MHSAMI and that there are some bona fide heart failure cases in the MHSAMI data set. We believe that most non-heart-failure data sets (e.g., data on chronic obstructive pulmonary disease patients) will not include many of the long Framingham Criteria variables, though they are more likely to include the six Minnesota Heart Failure Criteria variables and possibly data on LVEF. In this sense the LCA method, including LVEF, is capable of doing the desired epidemiologic job—namely surveillance of heart failure occurrence in a broad set of hospitalized patients, including many who were not specifically suspected of having heart failure. The generalizability of the Minnesota Heart Failure Criteria must be verified in other populations, both to check their validity in other settings and to extend them to an outpatient setting. Repeatability is of particular concern for response patterns with a small number of subjects. Another limitation of our criteria is that they did not identify a separate category corresponding to clinical isolated diastolic dysfunction. Although LVEF is related to diastolic dysfunction, the other signs and symptoms are apparently not sufficiently indicative of isolated diastolic dysfunction for the final LCA model to identify a subgroup with isolated diastolic dysfunction. Using LCA, we identified a plausible classification structure for heart failure with three categories of risk strata based on six Framingham Criteria variables for which data are readily available from medical records (i.e., dyspnea, pulmonary rales, cardiomegaly, S3 heart sound, interstitial or pulmonary edema, and elevated heart rate), plus LVEF. We found that the LCA classification provides better discrimination between cases and noncases against several previous sets of truncated criteria and equal discrimination against a truncated form of the Framingham Criteria that closely approximates the full version but requires many 192 Kim et al. fewer variables. The posterior probabilities from the LCA model (Web appendix 2 (http://www.aje.oxfordjournals.org)) form the basis for the Minnesota Heart Failure Criteria, which have the potential to facilitate the epidemiologic classification of heart failure. ACKNOWLEDGMENTS Funding was provided in part by grants RO1-HL-23727 and RO1-HL60959 from the National Heart, Lung, and Blood Institute. The authors thank the participating hospitals in MinneapolisSt. Paul for their long-lasting support of epidemiologic research. They are indebted to the study programmers and dedicated nurse abstractors of the Minnesota Heart Survey. Conflict of interest: none declared. REFERENCES 1. Association AH. Heart and stroke statistical update. Dallas, TX: American Heart Association, 2004. 2. Purcell IF, Poole-Wilson PA. Heart failure: why and how to define it? Eur J Heart Fail 1999;1:7–10. 3. Adams KF Jr, Zannad F. Clinical definition and epidemiology of advanced heart failure. Am Heart J 1998;135:S204–15. 4. Banerjee P, Banerjee T, Khand A, et al. Diastolic heart failure: neglected or misdiagnosed? J Am Coll Cardiol 2002; 39:138–41. 5. Cheng TO. Definition of heart failure. (Letter). Eur J Heart Fail 1999;1:433–4. 6. Denolin H, Kuhn H, Krayenbuehl HP, et al. The definition of heart failure. Eur Heart J 1983;4:445–8. 7. Harley A. The management of heart failure: a matter of definition? Cardiovasc Drugs Ther 1993;7:661–9. 8. Tavazzi L. Towards a more precise definition of heart failure aetiology. Eur Heart J 2001;22:192–5. 9. Wagner S, Cohn K. Heart failure. A proposed definition and classification. Arch Intern Med 1977;137:675–8. 10. Wilhelmsen L, Eriksson H, Svardsudd K, et al. Improving the detection and diagnosis of congestive heart failure. Eur Heart J 1989;10:13–18. 11. Yip G, Wang M, Zhang Y, et al. Left ventricular long axis function in diastolic heart failure is reduced in both diastole and systole: time for a redefinition? Heart 2002;87: 121–5. 12. Young JB, Pratt CM. Hemodynamic and hormonal alterations in patients with heart failure: toward a contemporary definition of heart failure. Semin Nephrol 1994;14:427–40. 13. Mosterd A, Deckers JW, Hoes AW, et al. Classification of heart failure in population based research: an assessment of six heart failure scores. Eur J Epidemiol 1997;13: 491–502. 14. Eriksson H, Caidahl K, Larsson B, et al. Cardiac and pulmonary causes of dyspnoea—validation of a scoring test for clinical-epidemiological use: The Study of Men Born in 1913. Eur Heart J 1987;8:1007–14. 15. McKee PA, Castelli WP, McNamara PM, et al. The natural history of congestive heart failure: The Framingham Study. N Engl J Med 1971;285:1441–6. 16. Walma EP, Hoes AW, Prins A, et al. Withdrawing long-term diuretic therapy in the elderly: a study in general practice in the Netherlands. Fam Med 1993;25:661–4. 17. Schocken DD, Arrieta MI, Leaverton PE, et al. Prevalence and mortality rate of congestive heart failure in the United States. J Am Coll Cardiol 1992;20:301–6. 18. Gheorghiade M, Beller GA. Effects of discontinuing maintenance digoxin therapy in patients with ischemic heart disease and congestive heart failure in sinus rhythm. Am J Cardiol 1983;51:1243–50. 19. Carlson KJ, Lee DC, Goroll AH, et al. An analysis of physicians’ reasons for prescribing long-term digitalis therapy in outpatients. J Chronic Dis 1985;38:733–9. 20. Jaski BE. Basics of heart failure. Boston, MA: Kluwer Academic Publishers, 2000. 21. McKee PA, Castelli WP, McNamara PM, et al. The natural history of congestive heart failure: The Framingham Study. N Engl J Med 1971;285:1441–6. 22. McGovern PG, Jacobs DR Jr, Shahar E, et al. Trends in acute coronary heart disease mortality, morbidity, and medical care from 1985 through 1997: The Minnesota Heart Survey. Circulation 2001;104:19–24. 23. Shahar E, Lee S, Kim J, et al. Hospitalized heart failure: rates and long-term mortality. J Card Fail 2004;10:374–9. 24. Wagner S, Cohn K. Heart failure. A proposed definition and classification. Arch Intern Med 1977;137:675–8. 25. Guggenmoos-Holzmann I, van Houwelingen HC. The (in)validity of sensitivity and specificity. Stat Med 2000;19: 1783–92. 26. Torrance-Rynard VL, Walter SD. Effects of dependent errors in the assessment of diagnostic test performance. Stat Med 1997;16:2157–75. 27. Walter SD, Irwig LM. Estimation of test error rates, disease prevalence and relative risk from misclassified data: a review. J Clin Epidemiol 1988;41:923–37. 28. Rindskopf D, Rindskopf W. The value of latent class analysis in medical diagnosis. Stat Med 1986;5:21–7. 29. Uebersax JS, Grove WM. Latent class analysis of diagnostic agreement. Stat Med 1990;9:559–72. 30. Hagenaars J, McCutcheon A. Applied latent class analysis. Cambridge, UK: Cambridge University Press, 2002. 31. McCutcheon A. Latent class analysis. Newbury Park, CA: Sage Publications, 1987. 32. Kaldor J, Clayton D. Latent class analysis in chronic disease epidemiology. Stat Med 1985;4:327–35. 33. Vermunt JK, Magidson J. Latent GOLD 2.0 user’s guide. Belmont, MA: Statistical Innovations, Inc, 2000. 34. Harlan WR, Oberman A, Grimm R, et al. Chronic congestive heart failure in coronary artery disease: clinical criteria. Ann Intern Med 1977;86:133–8. 35. Feinstein AR. Clinimetrics. New Haven, CT: Yale University Press, 1987. 36. Ascherio A, Rimm EB, Giovannucci EL, et al. A prospective study of nutritional factors and hypertension among US men. Circulation 1992;86:1475–84. 37. Aldoori WH, Giovannucci EL, Rimm EB, et al. A prospective study of diet and the risk of symptomatic diverticular disease in men. Am J Clin Nutr 1994;60:757–64. 38. Mosterd A, Cost B, Hoes AW, et al. The prognosis of heart failure in the general population: The Rotterdam Study. Eur Heart J 2001;22:1318–27. 39. Murdoch DR, Love MP, Robb SD, et al. Importance of heart failure as a cause of death. Changing contribution to overall mortality and coronary heart disease mortality in Scotland 1979–1992. Eur Heart J 1998;19:1829–35. Am J Epidemiol 2006;164:184–193 Prognostic Value of the Minnesota Heart Failure Criteria 40. Changes in mortality from heart failure—United States, 1980–1995. MMWR Morb Mortal Wkly Rep 1998;47: 633–7. 41. Pernenkil R, Vinson JM, Shah AS, et al. Course and prognosis in patients > or ¼ 70 years of age with congestive heart failure and normal versus abnormal left ventricular ejection fraction. Am J Cardiol 1997;79:216–19. 42. Hillege HL, Girbes AR, de Kam PJ, et al. Renal function, neurohormonal activation, and survival in patients with chronic heart failure. Circulation 2000;102:203–10. 43. Zannad F, Braincon S, Juilliere Y, et al. Incidence, clinical and etiologic features, and outcomes of advanced chronic heart failure: The EPICAL Study. Epidemiologie de l’Insuffisance Am J Epidemiol 2006;164:184–193 44. 45. 46. 47. 193 Cardiaque Avancee en Lorraine. J Am Coll Cardiol 1999;33: 734–42. Rector TS, Cohn JN. Prognosis in congestive heart failure. Annu Rev Med 1994;45:341–50. Cowie MR, Wood DA, Coats AJ, et al. Survival of patients with a new diagnosis of heart failure: a population based study. Heart 2000;83:505–10. Ho KK, Pinsky JL, Kannel WB, et al. The epidemiology of heart failure: The Framingham Study. J Am Coll Cardiol 1993;22:6A–13A. Killip T 3rd, Kimball JT. Treatment of myocardial infarction in a coronary care unit. A two year experience with 250 patients. Am J Cardiol 1967;20:457–64.