* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Hospital infection Control
Survey
Document related concepts
Transcript
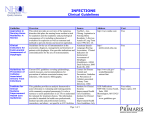
N Hospital infection Control n Nosocomial infections (hospital –acquired infection): An infection acquired in [a] hospital by a patient who was admitted for a reason other than that infection. OR: An infection occurring in a patient in a hospital or other health care facility in whom the infection was not present or incubating at the time of admission. N As a general timeline, infections occurring more than 48 hours after admission are usually considered nosocomial. Frequency of infection: Nosocomial infection occurs worldwide and affects both developed and poor countries. According to studies conducted by WHO, 8.7% of hospitalized patients had nosocomial infection. Factors influencing the development of nosocomial infection: 1-The microbial agents and antibiotic-resistance ability: -Patients are exposed to a variety of microorganisms during a hospital stay: A- Endogenous microbes: Part of a patient’s own flora. B- Exogenous microbes: -Patients, and Visitors. -Medical staff (doctor, nurse, physiotherapist, technician). -Instruments (Endoscopy, catheter, surgical instruments) -Fluids, blood, or food. -Dust, and Insect bite. N Hospital-dwelling microbes: Bacteria: Staphylococcus aureus (MRSA), coagulase-negative Staphylococci, Enterococci (VRE), and Enterobacteriaceae species. Viruses: Hepatitis B and C, Rotaviruses, and Enteroviruses. Fungi: Candida albicans. N Hospital-dwelling bacteria could develop antibiotics resistance ability due to conjugation process. Conjugation: Transfer of bacterial plasmid from one bacterium to another by sex pili. Plasmid: Extracircular supercoiled DNA that carry some important gene such as the reporter genes (CAT gene). N 2. Patient susceptibility: Important patient factors influencing acquisition of infection are: 1-Age : infancy and old age. 2-Immune status: chronic diseases like malignant tumor, diabetes, renal failure immunosuppressive therapy and AIDS. 3-Underlying disease : injuries to skin (burn, wound), ischemia. 4-Malnutrition. 5-Diagnostic and therapeutic interventions: biopsies, catheterization, I.V. cannulation, endoscopic examination, incubation/ventilation. n 3. Environmental Factors: -Different factors play a role in establishment of Nosocomial infections: 1-Crowded conditions. 2-Frequent transfer of patients from one unit to another. 3-Concentration of susceptible patients: (newborn infants, burn patient, intensive care). 4-Microbial flora may contaminate objects, devices that may come in susceptible site of the patient. Sources of Hospital-acquired Infections: Nimer CONTAMINATED HOSPITAL ENVIRONMENT Instruments, Fluids, Food, Air, Medications Invasive medical devices : Iatrogenic Patient Normal flora Cutaneous, GIT, Genitourinary, Respiratory Plasmid transfer Medical Personnel: Colonized, Infected, Transient, Carriers. Urinary Catheter, Intravenous catheter, Endotracheal tubes, Endoscopes Common Nosocomial Infections: 1. Urinary tract infections (UTI): This is the most common nosocomial infection it account for 40 % of hospital acquired infections; 80% of infections are associated with the use of an indwelling catheter. Organisms : E.coli, multi-resistant Klebsiella, Pseudomonas aeruginosa, Enterobacter and Candida albicans. Source: Endogenous flora or exogenous from other patients, health care provider, instrument, etc. N Diagnosis: positive urine culture (1 or 2 species) with at least 105 bacteria/ ml, with or without clinical symptoms. Prevention: 1-Remove the indwelling urinary catheter as soon as possible. 2-Use aseptic technique for inserting or manipulating the catheter. 3-Maintain an unobstructed urinary flow. 4-Ensure that the patient is taking sufficient amount of fluids per day (3-4 L). 5-Give proper antibiotic therapy for proper course. N 2.Nosocomial Pneumonia: Nosocomial pneumonia is the second most common nosocomial infection accounting for 15 % of all nosocomial infections. It is associated with mortality rates that range from 20-50 %. It occurs in several patient groups, the most important are patients on ventilator in intensive care units (ICU), where the Incidence rate of pneumonia is 3% per day. N Organisms: Staph aureus, Pseudomonas , Enterobacter, Klebsiella pneumoniae, Candida albicans and Haemophilus influenzae. Source: endogenous from upper air way, and exogenous from contaminated respiratory equipment, patients, visitors, etc. Diagnosis: isolation of microbe from clinical specimens, and presence of signs and symptoms of infect. n Prevention: 1-Wear gloves; for contact with respiratory secretions. 2-Wash hands after contact with respiratory secretions, even if gloves have been worn. 3-Maintain open airway. 4-Isolate patient with potentially transferred respiratory infections. N Other hospital-acquired infections: 1-Surgical site infections: Staphylococcus aureus, Staphylococcus epidermidis (Intravenous catheter). 2-Nosocomial Bacteremia. 3-Skin and soft tissue infections: Open sores (ulcers, burns and bedsores). 4-Gastroenteritis : The most common nosocomial infection in the children, where rotavirus is a chief pathogen. N 5-Nosocomial Bloodborne diseases: A-Hepatitis B virus: -Transmission rate was 25%, reduced due to application of vaccination, the practice of not recapping needle, and Hepatitis B surface antigen screening test. B-Hepatitis C: Rate is 3%. Anti-viral drugs at first 8 hrs reduce the infection by 60%. C-HIV: Rate is 0.3% Infection Control : -Biological safety precautions. -Hand hygiene. -Clean & contaminated area. -Management of blood & body fluid spillage. -Immunization of health care workers. -Post exposure management for health care workers. Biological safety precautions: 1-All clinical specimens should be considered as potentially hazardous. 2-Wear Lab coat, gloves, shoes (Protective purpose). 3- Remove gloves when using the telephone or photocopier. 4- Skin cuts on the hands, must be covered with a waterproof dressing prior to start working. n 5-Never perform any action which may bring your hands into contact with your face, eyes or mouth, such as eating, smoking or adjusting contact lenses. 6-Remove laboratory coat and gloves and wash hands before leaving your working area. Hand hygiene: When Do We Need to Wash Our Hands? -Before eating -Before starting work -Before and after any patient contact -After contact with potentially contaminated materials like blood, urine, CSF. -Before wearing gloves. -After removing gloves. -Before and after performing any medical procedure -Before leaving work. When Do We Need to Wash Our Hands? N Types of Hand Hygiene (Decontamination): 1-Routine care (minimal): -Hand washing with non antiseptic soap. -Or quick hygienic hand disinfection by rubbing with alcoholic solution. 2-Antiseptic hand cleaning (moderate) – aseptic care of infected patients: -Hygienic hand washing with antiseptic soap. -Quick hand disinfection by rubbing with alcoholic solution. 3-Surgical scrub (surgical care): Surgical hand and forearm washing with antiseptic soap and sufficient time and duration of contact (3 – 5 minutes). Clean & contaminated area: Control of spreading of infection could be achieved by classifying hospital environment into one of four zones: Zone A: no patient contact. Normal cleaning . (e.g. administration, library). Zone B: Care of patients, who are not infected and not highly susceptible. Wet disinfection with detergent. Zone C: infected patients (isolation wards). Clean with a detergent/disinfectant solution, with separate cleaning equipment for each room. N Zone D: High–susceptible patient (protective isolation) or protected areas such as: Operating room, delivery rooms, intensive care units, premature baby units, and haemodialysis unit. -Clean using a detergent/disinfectant solution and separate cleaning equipment. Blood and body fluid spillage, and contamination management : PURPOSE: To protect healthcare workers, patients and visitors from unnecessary exposures to bloodborne pathogens and other potentially infectious body fluids. Three types: 1-Low grade disinfection: Quaternary ammonium: Bactericidal effect. used for low amount- blood spillage. N 2-Intermediate grade disinfection: Phenol and 70-90% alcohol ;Bactericidal and Virucidal effect. Used for low amount -blood spillage (less than 50ml). 3-High grade disinfection: Formaldehyde ,Glutaraldehyde, Sodium hydrochlorite , and hydrogen peroxide. : Sporicidal ,Mycobactericidal, Fungicidal, and bactericidal effect. Used for: high blood spillage (more than 50ml), and fungal decontamination. NOSOCOMIAL INFECTION SURVEILLANCE: The development of a surveillance is an essential first step to identify local problems , and evaluate the effectiveness of the infection control activity. Objectives: The purpose of surveillance program is to detect, record, and report hospital acquired infection aiming to reduce them and their costs. N 2. Strategy of Surveillance: A surveillance system must meet the following criteria: Simplicity: to minimize costs and work load, and promote unit participation by feedback. Flexibility: to allow changes when appropriate. Acceptability: Evaluated by ICC according to data analysis. Consistency: use standardized definitions and methodology Sensitivity. Specificity. Infection Control Committee: 1-Management 2-Epidemiologist 3-Physicians 4-Other health care workers(Laboratory, or Nurse). 5-Clinical microbiologist 6-Pharmacy 7-Central supply 8-Maintenance Tasks (most important) of the committee -To review and approve a yearly program of activity for surveillance and prevention. -To review epidemiological surveillance data and identify areas for intervention. Role of the physician: 1-Direct patient care using practices which minimize infection. 2-Appropriate practice of hygiene: (hand washing, and isolation). 3-Supporting the infection control team. 4-Protecting their own patients from other infected patients and from hospital staff who may be infected. 5-Obtaining appropriate microbiological specimens when an infection is present or suspected.