* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Consultation in University-Based and Community
Middle East respiratory syndrome wikipedia , lookup
Bioterrorism wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Chagas disease wikipedia , lookup
Onchocerciasis wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Schistosomiasis wikipedia , lookup
Marburg virus disease wikipedia , lookup
Oesophagostomum wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
Leptospirosis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
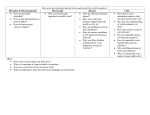
391 Consultation in University-Based and Community-Based Infectious Disease Practices: A Prospective Study Daniel J. Sexton, G. Ralph Corey, Christopher W. Ingram, Vickie M. Morris, and Hubert B. Haywood III Division of Infectious Diseases, Duke University Medical Center, Durham; and Raleigh Infectious Diseases Associates PA, Raleigh, North Carolina Estimates on the current and future manpower requirements for infectious disease consultants vary widely [1-4]. Such approximations have been based more on opinion than on fact because data that quantify and characterize the actual work of infectious disease physicians are sparse. Indeed, even the exact number of clinicians practicing in the subspecialty of infectious diseases in the United States is unknown. A questionnaire and telephone survey sponsored by the Infectious Diseases Society of America in 1987 provided useful information on the numbers, type, and practice patterns of infectious disease physicians but did not include information on the types of patients seen by these clinicians [5]. Such data could be useful to persons involved in the training of infectious disease physicians, to policy planners, and to the social architects who may design future medical care systems by bureaucratic or government edicts. Because of a lack of such data, we undertook a study to examine the rates, timing, and type of inpatient consultations by infectious disease specialists in two settings: a community-based consultative practice and the consult service of a large university medical center. Methods Clinicians were asked to complete a standard data form for each inpatient consultation during the period from 1 Sep- Received 8 April 1994; revised 21 June 1994. Reprints or correspondence: Dr. Daniel J. Sexton, Duke University Medical Center, Box 3605, Durham, North Carolina 27710. Clinical Infectious Diseases 1995;20:391-3 © 1995 by The University of Chicago. All rights reserved. 1058-4838/95/2002-0025$02.00 tember 1992 to 31 March 1993. These clinicians included 16 infectious disease physicians at Duke University Medical Center, which consists of a 1,000-bed university hospital and a 350-bed university-affiliated Veterans Administration hospital, and three infectious disease physicians from Raleigh Infectious Diseases Associates who practice at three community hospitals that range in size from 150 to 550 beds. Information was collected concerning the time a consultation was requested, the type of physician or service requesting a consultation, and known or suspected pathogens, disease processes, and affected organ systems. The data form allowed physicians to designate multiple pathogens, disease processes, and/or affected organ systems for individual patients. In addition, data were collected on whether recommendations were made to adjust or initiate antimicrobial therapy as a result of the consultation, whether the patient had a nosocomial infection, and whether the patient was in an intensive care unit at the time of consultation. Patients at the university hospitals were seen by infectious disease fellows and faculty; patients at the three community hospitals were seen by one of three infectious disease consultants in a private practice group that was established in 1991. Differences between proportions were calculated with use of the x 2 test, and P values of .05 were considered statistically significant. Results Sixteen university-based faculty members completed a total of 859 consultations, whereas the three infectious disease physicians in private practice completed a total of 507 con- Downloaded from http://cid.oxfordjournals.org/ at Penn State University (Paterno Lib) on May 12, 2016 Infectious disease physicians in university and community practices completed a standard data form following each of 1,366 inpatient consultations during a 7-month period. The rate of consultation was higher in the university practice than in the community practice (3.4 vs. 1.8 per 100 discharges, respectively). Known or suspected bacterial pathogens accounted for more than half of all consultations in both practice groups. The three organ systems most commonly affected by infection were pulmonary (20% in university practice vs. 19% in community practice), skin and soft tissue (13% in university practice vs. 20% in community practice), and musculoskeletal (12% in university practice vs. 16% in community practice). Bloodstream infection, pneumonia, unexplained fever, osteomyelitis, urinary tract infection, and cellulitis were the six most common disease processes that led to consultation in both practice groups. The percentage of patients with noninfectious diseases and the percentage for whom a change in antimicrobial therapy was advised was nearly identical in both practice settings. Physicians in private practice performed more consultations on weekends (20% vs. 11% in university practices, P < .001) and between 6:00 P.M. and 7:00 A.M. (15% vs. 6% in university practices, P < .001). The scope and diversity of the work of consultants in community practices are nearly identical to those of their colleagues in university-based practices. 392 Sexton et al. Table 1. Referring service for consultations in infectious diseases, by type of practice: 1 September 1992 to 31 March 1993. No. (%) of consultations Referring service 177 101 97 81 65 43 32 31 36 23 27 24 51 71 (21) (12) (11) (9) (7) (5) (4) (4) (4) (3) (3) (3) (6) (8) Community practice 176 (35) 39 (8) 17 (3) 42 (8) 33 (7) 31 (6) 23 (5) 24 (3) 9 (2) 30 (1) 31 (4) 10 (<1) 28 (6) 50 (10) sultations during the same 7-month period. The rate of consultations in university practice was 3.4/100 discharges; the consultation rate in private practice was 1.8/100 discharges. For the university-based specialists, consultations were requested by a total of 23 different services or subspecialties; for the private practice physicians, consultations were requested by a total of 19 different services or subspecialties. For the university-based group, 47% of their consultations were by referral from general internists and medical subspecialists and 40% were by referral from general surgeons and surgical subspecialists. The private group saw more patients by referral from general internists and medical subspecialists (63%) and fewer patients from general surgeons and surgical subspecialists (28%) (table 1). A similar percentage of patients in both groups were in intensive care units at the time of consultation ( 1 8% in university practice vs. 20% in private practice). Infectious disease physicians in private practice performed more consultations on weekends than university-based specialists (20% vs. 1 1 %, respectively, P < .001). There was also a significant difference between the two groups in the percentage of consultations requested between 6 P.M. and 7 A.M. ( 1 5% in private practice vs. 6% in university practice, P < .001). A microbiological diagnosis had been established at the time of consultation for 41% of patients seen by the private group and for 38% of patients seen by the university group. A total of 369 pathogens were identified or suspected in patients seen by private practice specialists; 662 pathogens were identified or suspected by university-based consultants (table 2). Staphylococcus aureus was the most common pathogen identified or suspected in both patient groups. The frequency of other pathogens identified was similar among both groups with only one relevant exception: more inpatients seen by university-based consultants were infected with the human immunodeficiency virus (HIV) (9% vs. 2% in private practice, P < .05). However, during the study period, a total of 28 patients with HIV infection were admitted by the infectious disease physicians in private practice. Patients from both clinical settings had infectious diseases that involved a wide array of organ systems. The most commonly involved organ systems in patients seen by university vs. private practice physicians were pulmonary (20% vs. 19%), skin and soft tissue (13% vs. 20%), and musculoskeletal (12% vs. 1 6%), respectively. Bloodstream infection, pneumonia, unexplained fever, osteomyelitis, urinary tract infection, and cellulitis were the six most common disease processes that led to consultation in both practice groups (table 3). Slightly more patients seen by university-based consultants had nosocomial infections (33% vs. 26% in private practice). Known or suspected bacterial pathogens accounted for more than half of all consultations in both practice groups (55% in university practice vs. 62% in private practice). Some- Table 2. Categories of disease and known or suspected pathogens found in patients seen in infectious disease consultations, by type of practice: 1 September 1 992 to 31 March 1993. No. (%) of consultations Category of disease or pathogen Category of disease Bacterial Viral Fungal Mycobacterial Protozoan* Noninfectious disease Pathogen Staphylococcus aureus HIV Candida Enterococci Coagulase-negative staphylococci Streptococci Anaerobes Pseudomonas Escherichia coli Mycobacterium tuberculosis Nontuberculous mycobacteria Klebsiella Enterobacter Pneumocystis carinii Other bacteria CMV/HSV/VZV Other fungi University practice Community practice 473 (55) 99 (12) 73 (9) 38 (4) 16 (2) 120 (14) 313 (62) 32 (6) 37 (7) 15 (3) 7 (1) 45 (9) 113 (15) 79 (9) 43 (5) 42 (5) 41 (5) 38 (4) 31 (4) 32 (4) 32 (4) 17 (2) 19 (2) 19 (2) 15 (2) 12(1) 78 (9) 23 (3) 28 (3) 75 (13) 8 (2) 23 (5) 31 (6) 34 (7) 45 (9) 24 (5) 30 (6) 15 (3) 12 (2) 1 (<1) 8 (2) 7 (1) 3 (<1) 2 (6) 12 (2) 9 (2) NOTE. HIV = human immunodeficiency virus; CMV = cytomegalovirus; HSV = herpes simplex virus; VZV = varicella zoster virus. * Inclues P. carinii. Downloaded from http://cid.oxfordjournals.org/ at Penn State University (Paterno Lib) on May 12, 2016 General medicine Orthopedics General surgery Cardiology Cardiovascular surgery Family medicine Neurosurgery Hematology-oncology Pulmonary Obstetrics-gynecology Neurology Psychiatry Other surgical subspecialties Other medical subspecialties University practice CID 1995;20 (February) Consultation in Infectious Disease Practices CID 1995;20 (February) Table 3. Known or suspected disease processes in patients seen in infectious disease consultations, by type of practice: 1 September 1992 to 31 March 1993. No. (%) of consultations Disease process 140 131 129 83 81 80 76 66 58 59 47 94 (16) (15) (15) (10) (9) (9) (9) (8) (7) (7) (5) (11) Community practice 79 (16) 87 (17) 128 (25) 36 (7) 57 (11) 26 (5) 31 (7) 51 (10) 50 (10) 8 (2) 19 (4) 30 (6) what surprisingly, 14% of university consultations and 9% of private practice consultations were for noninfectious diseases (such as drug fever, rheumatologic disorders, noninfectious pulmonary diseases, or pretransplantation evaluations). Infectious disease specialists in private practice recommended a change in antimicrobial therapy in 66% of all consultations; a change in therapy was advised for 59% of patients seen by university consultants. Discussion We were surprised to find so many similarities between the inpatient consultation practices of infectious disease specialists in university-based practice and those of specialists in private practice. The only remarkable differences found between the two groups were in the percentages of patients with HIV infection and in the frequency of night and weekend requests for consultation. In an earlier report, one of the authors noted that the rate of infectious disease consultation was higher in a private practice group in Oklahoma City (3.1 consults per 100 discharges) than in the university-based practice at Duke University Medical Center (2.3 consults per 100 discharges) [6]. Opposite findings were noted in our study. The private group practice surveyed in the current report was established in 1991; thus, its rate of inpatient consultation may currently be lower than that of older, more established private practices in infectious diseases. Furthermore, the rate of inpatient infectious disease consultations at Duke University Medical Center has increased by 48% since 1987. Most patients seen in consultations by each group had bacterial disease, particularly infections with gram-positive cocci. A microbiological diagnosis had been established at the time of consultation for approximately 40% of all patients. These findings suggest that infectious disease physicians are consulted almost as frequently for their expertise in therapy design as for their diagnostic skill. Indeed, physicians from both groups recommended a change in existing therapy in almost two-thirds of consultations. These data have implications for directors of training programs in infectious diseases. Fellowship programs in infectious diseases should prepare trainees to assist in the management of a broad array of subspecialty-related infections; the programs should also provide in-depth education on the problems most often seen by infectious disease consultants such as skin, soft tissue, musculoskeletal, and pulmonary infections. As almost one-third of all consultations were directly or indirectly related to nosocomial infections, training in the principles and management of hospital-acquired infections is important. Since surgical consultations represented 28%-40% of all consultations, thorough education about the principles of surgical infections is necessary. Finally, as —10% of consultations were for noninfectious diseases, a wide knowledge of general internal medicine is mandatory for infectious disease clinicians. Our study did not examine the outcome of the consultation process. Further studies that examine how the specialized skills of infectious disease specialists impact patient care and hospital outcomes are needed. Although such studies are difficult to design and undertake, they could be important to the continuing success of clinical infectious disease practices in both university medical centers and the community. Our data illustrate that the scope and diversity of the work of infectious disease specialists in community-based practice are nearly identical to those of their colleagues in universitybased practice. Although future changes in reimbursement policies and managed care contracts may substantially alter the way all subspecialists practice, infectious disease clinicians currently have diverse and challenging work that requires a broad knowledge of infectious diseases and frequent interaction with numerous other subspecialists and clinicians. References 1. Beeson PB. Too many specialists, too few generalists. Pharos 1991; 54: 2-6. 2. Ervin FR. The bell tolls for the infectious diseases clinician. J Infect Dis 1986; 153:183-5. 3. Eickhoff TC. Whither infectious diseases? Some data at last. J Infect Dis 1992; 165:201-4. 4. Petersdorf RG. Whither infectious diseases? Memories, manpower, and money. J Infect Dis 1986; 153:189-95. 5. Hamory BH, Hicks LL, Manpower and Training Committee, Infectious Diseases Society of America. Infectious disease manpower in the United States-1986. 1. Description of infectious disease physicians. J Infect Dis 1992; 165:205-17. 6. Sexton DJ. Rates of infectious disease consultations in hospitals of different sizes and types, 1986-1987 [letter]. Rev Infect Dis 1991; 13:527. Downloaded from http://cid.oxfordjournals.org/ at Penn State University (Paterno Lib) on May 12, 2016 Bloodstream infection Pneumonia Unexplained fever Osteomyelitis Urinary tract infection Cellulitis Intraabdominal infection Wound infection CNS infection HIV infection Abscess Other University practice 393