* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Treatment with beta-adrenergic blocking agents after
Survey
Document related concepts
Transcript
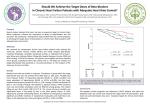
JACC Vol. 25, No. 6 May 1995:1327-32 1327 MYOCARDIAL INFARCTION Treatment With Beta-Adrenergic Blocking Agents After Myocardial Infarction: From Randomized Trials to Clinical Practice SAMI VISKIN, MD,* ILAN KITZIS, MD,? ELI LEV, MD, ZEEV ZAK, MD, KARIN HELLER, MD, Y A E L V I L L A , MSc,~ A L E J A N D R O BERNARD BELHASSEN, ZAJARIAS, MD,§ SHLOMO LANIADO, MD, FACC, MD, F A C C Tel Aviv, Israel; Syracuse, New York; and Mexico City, Mexico Objectives. Our aim was to determine the percent of patients with myocardial infarction who are treated with beta-adrenergic blocking agents in dosages proved to be effective in preventing death after a heart attack. Background. In the prospective randomized trials showing that beta-blocker treatment improves survival rates after myocardial infarction, relatively high dosages of these agents were used. However, it is not known whether these dosages are used in current clinical practice. Methods. In a retrospective analysis of clinical data from 606 consecutive survivors of myocardial infarction at four university hospitals in three countries, we assessed the number of infarct survivors receiving prospectively defined "effective dosages" of beta-blockers. We defined these dosages as those that demonstrated improved survival rates of infarct survivors who received active drug in large, prospective, double-blind, placebo-controlled trials. Results. Only 58% of infarct survivors with no contraindications to beta-blockers received these drugs at the time of hospital discharge, and only 11% received dosages equivalent to >50% of the effective dosages. Independent predictors of failure to prescribe beta-blockers to infarct survivors without contraindications to these drugs were the use of diuretic agents, transient heart failure, impaired left ventricular function and increased patient age. Among patients receiving beta-blockers, only the use of propranoiol predicted prescription of a low beta-blocker dosage. Conclusions. Failure to prescribe beta-blockers after myocardial infarction is common but in most cases is not due to clear contraindications. Many patients not receiving beta-blockers belong to subgroups that would derive the greatest benefit from such treatment. Finally, even when beta-blockers are prescribed, the dosages used are considerably lower than those proved to be effective in preventing death after myocardial infarction. (J Am Coil Cardioi 1995;25"1327-32) Prospective randomized trials have shown that beta-blockers improve the long-term prognosis of patients with myocardial infarction (1): mortality, cardiac death and sudden cardiac death are reduced by 21%, 24% and 30%, respectively (1,2). In addition, treatment with beta-blockers reduces the risk of reinfarction by 25% (1). Therefore, infarct survivors who have no specific contraindications to beta-blockers should routinely be offered such therapy (3,4). However, although data on the beneficial effects of betablockers have existed for almost 2 decades (5), many infarct survivors are not being treated with these agents. A recent survey of medical practices in 16 hospitals in Massachusetts (6) and two multicenter trials in the United States (7) and Europe (8) demonstrated that only 44% to 56% of patients were receiving beta-blocker therapy after a myocardial infarction. These numbers are surprising because clear contraindications to such treatment were found in only 18% of patients enrolled in prospective beta-blocker trials (9,10). Although several studies have found predictors of failure to prescribe beta-blockers, including impaired left ventricular ejection fraction (11), evidence of heart failure (6,11) and increased patient age (6,12,13), we know of no published data on the dosages of beta-blockers generally prescribed after a myocardial infarction. Such data are important because trials showing improvement in survival rates with beta-blocker treatment invariably used relatively high dosages (9,14-16). Therefore, the aim of this study was to analyze the percent of infarct survivors who receive beta-blockers in dosages comparable to those proved to be effective in improving long-term survival. From the Departmentsof Cardiologyand EmergencyMedicine,SouraskyTel AvivMedicalCenter and SacklerSchoolof Medicineand :]:Departmentof Statistics, Tel AvivUniversity,Tel Aviv. Israel; +State Universityof New York Health Science Center, Syracuse, New York: and §lnstituto Nacional de Cardiologialgnacio Chavez,MexicoCity,Mexico.Dr. Viskinis a recipientof a fellowship from the American PhysiciansFellowship for Medicine in Israel. Brookline,Massachusetts. Manuscript receivedJuly 14, 1994;revisedmanuscriptreceivedDecember9. 1994, acceptedDecember15, 1994. *Presentaddressand addressfor correspondence:Dr. SamiViskin,Department of Cardiology,ElectrophysiologyDivision. Universityof California, San Francisco, 500 Parnassus Avenue,Box 1354,San Francisco,California94143. ©1995 by the AmericanCollegeof Cardiology Methods We reviewed the files of consecutive patients discharged with a diagnosis of acute myocardial infarction from one American, one Mexican and two Israeli hospitals. The patients had been treated in wards of Internal Medicine and Cardiology at the State University of New York Health Science Center, 0735-1097/95/$950 0735-1097(94)00552-2 1328 V1SKIN ET AL. BETA BLOCKERS AFTER MYOCARDIAl_ INFARCTION Syracuse, New York (166 patients), lnstituto Nacional de Cardiologia Ignacio Chavez, Mexico City, Mexico (71 patients), the Chaim Sheba Medical Center, Tel-Hashomer, Israel (113 patients) and the Souras~-Tel Aviv Medical Center, Tel Aviv, Israel (256 patients) during the last 6 months of 1993. Definitions. We defined contraindication to beta-blocker treatment according to the criteria used in the large prospective studies on beta-blocker treatment after myocardial infarction (9,10,14,15). Thus, the presence of any of the following classified a patient as having contraindications: 1) a diagnosis (or clinical signs) of asthma or chronic obstructive lung disease; 2) heart failure not controlled with diuretic drugs (furosemide >80 mg/day) or with digoxin and diuretic drugs (any dosage); 3) the presence of atrioventricular (AV) block of any degree, heart rate <50 beats/min or systolic blood pressure <100 mm Hg (unless transient) before treatment with betablockers. The type and daily dosage of beta-blocker recommended at the time of hospital discharge were recorded as a percent on the basis of the "effective dosage." We defined "demonstrated effective dosages," (or, in short, "effective dosages") of betablockers as the dosages used in large prospective double-blind placebo-controlled beta-blocker trials that demonstrated improved survival in the patients receiving active drug. Accordingly, we defined "effective dosages" as follows: propranolol, 160 m~' day (9,15); metoprolol, 200 mg/day (14), or atenolol, 100 mg/day (17). We found no patients receiving timolol, sotalol, pindolol, practolol, oxprenolol or acebutolo[ at the time of hospital discharge. Statistics. The following variables were analyzed for their value in predicting absence of beta-blocker treatment among patients without contraindications to beta-blockers: age, gender, hospital from which the patients were discharged, infarct location, Q wave infarction, left ventricular ejection fraction, results of coronary angiography, revascularization procedures, lowest heart rate recorded, presence of arrhythmias, pulmonary edema, heart failure and hypotension at any time during the hospital stay and use of other medication (diuretic drugs, calcium channel blocking agents, vasodilators, digoxin, nitrates, aspirin or anticoagulant agents). Univariate predictors were examined by chi-square test for discrete variables and t test or analysis of variance for continuous variables. The results are given as odd ratio and p values. In addition to the variables mentioned, the type of beta-blocker used was tested for prediction of the dosage of beta-blocker (expressed as percent of effective dosage) prescribed. Pearson correlation was performed to evaluate the relation between two continuous variables. Multivariate predictors of failure to prescribe beta-blockers were selected by logistic regression; stepwise regression was used to define the most important independent predictor of the dosage of beta-blocker prescribed. Statistical significance was defined as a p value <0.05. JACC Vol. 25, No. 6 May 1995:1327-32 Results Patient characteristics. During the study period, 606 patients (mean [+_SD] age 64 +_ 14 years) were discharged after a myocardial infarction. Of these, 69% were male and 78% were <75 years old; in 31%, the infarct involved the anterior wall, in 59% it was inferior or inferoposterolateral and in 9% it was not localized. A Q wave infarction occurred in 45% of patients. Transient complications among infarct survivors included bradyarrhythmias in 22%, atrial or ventricular tachyarrhythmias in 16%, hypotension in 10%, heart failure in 21%, pulmonary edema in 14% and cardiogenic shock in 2%. Data on left ventricular ejection fraction were available for 54% of patients. The mean ejection fraction was 45 _+ 19%; 90% and 71% of infarct survivors, respectively, had an ejection fraction >30% and >40%. Cardiac catheterization was performed during the hospital stay for myocardial infarction in 49% of patients: Single-, double- and triple-vessel coronary disease was found in 41%, 29% and 23%, respectively, of these patients, and normal coronary arteries were reported in 6%. During the hospital stay for infarction, coronary bypass surgery was performed in 7% of infarct survivors (14% of those undergoing catheterization); coronary angioplasty was attempted in 15% and was successful in 12% (29% and 23%, respectively, of those undergoing catheterization). Treatment with beta-blockers after myocardial infarction. Contraindications to treatment with beta-blockers were present in 18% of infarct survivors. They included bronchial asthma or chronic obstructive lung disease in 7%, heart failure controlled only with the use of >80 mg of furosemide daily or the use of digoxin in 7%, sinus bradycardia in 4%, AV block in 5% and hypotension at the time of hospital discharge in 5%. Many patients had more than one contraindication. Only 51% of all infarct survivors received beta-blocker treatment at the time of hospital discharge. Moreover, only 6% of all infarct survivors received an effective dosage of these drugs (Fig. 1). The percent of infarct survivors receiving beta-blockers was similar in all four hospitals (48%, 53% and 57% in the Israeli, the American and the Mexican hospitals, respectively; p = NS). However, the type of beta-blocker used varied among hospitals: Metoprolol was used in >85% of treated patients in the American and Mexican hospitals, whereas propranolol was the drug most commonly used (63% of treated patients) in the two Israeli hospitals. Atenolol was given to 26%, 11% and 5% of patients receiving beta-blockers in the Israeli, American and Mexican hospitals, respectively. The mean daily dosages used were 105 _+ 56 mg of metoprolol, 50 _+ 34 mg of propranolol and 65 + 57 mg/day of atenolol. Except for atenolol, which tended to be used in a higher dosage in the American hospital (111 _+ 122 mg/day, p : 0.05), the dosage of beta-blockers prescribed for infarct survivors was similar in the four hospitals studied (p = 0.2 and p = 0.13 for propranolol and metoprolol, respectively). Although 82% of infarct survivors had no contraindications to beta-blocker treatment, only 58% of this group received beta-blockers. Moreover, most patients receiving beta-blockers JACC Vol. 25. No. 6 May 1995:1327-32 50 VISKIN ET AL. BETA-BLOCKERS AFFER MYOCARDIAL INFARCTION 1329 Table 1. Predictors of Treatment With Beta-Blockers Among Infarct Survivors Without Contraindications T 49 45 Variable • 40 Odds Ratio (95% confidence limits) All Patients Univariate Analysis ~J Patients Without 35 Contraindications 3O 24.9 ~25 22 19.3 a. 2 0 Use of diuretic drugs Transient heart failuret Age >70 years LVEF not measured Use of calcium channel blockers Pulmonary edema LVEF <30% 15 10 7.9 5 2.8 3.3 Successful PTCA Electrical complications Female gender 0.25 (0.15-0.42)* 0.27 (0.16-0.47)* 0.30 (0.20-0.44)* 0.45 (0.31-0.64)* 0.45 (0.3l-0.66)* 0.33 (0.16-0.69):[: 0.32 (0.11-0.87)§ 0.60 (0.34-1.05)[[ 0.62 (0.38-1.04)1[ 0.69 (0.47-1.03)11 Multivariate Analysis (logistic regression) 0 0 1--25 26--50 51--75 >75 Percentage of Effective Dosage (%) Figure 1. Distribution of infarct survivors according to the dosage of beta-blocker prescribed at the time of hospital discharge. Dosages of beta-blockers are shown as percent of effective dosage (see Methods for definition of effective dosage). Solid bars = all patients surviving a myocardial infarction; open bars - all infarct survivors who had no contraindications to beta-blocker treatment. received a dosage significantly lower than those proved to be effective in preventing death (Fig. 1): Sixty-seven percent of infarct survivors without contraindications to beta-blockers (and 61% of those <70 years old) received a dosage equivalent to -<25% of the effective dosage of beta-blockers, whereas a dosage equivalent to >50% of the effective dosage was given to only 11% of infarct survivors without contraindications to beta-blockers regardless of age. Use of diuretic agents was the most important independent predictor of failure to prescribe beta-blockers to infarct survivors without contraindications to beta-blockers (Table 1). Other variables representing left ventricular dysfunction (transient or compensated heart failure, left ventricular ejection fraction <30% or pulmonary edema during the hospital stay) also predicted failure to prescribe beta-blockers at the time of hospital discharge (Table 1). Of note, persistent left heart failure despite treatment would classify a patient as having contraindications to beta-blockers. We found no significant correlation between any of the variables predicting failure to prescribe beta-blockers (Table 1) and the beta-blocker dosage actually prescribed (Table 2). By Pearson analysis, no correlation was found between the last heart rate recorded and the dose of beta-blocker prescribed. The only independent variable that predicted use of low (or high) beta-blocker dosage was the type of beta-blocker used (Table 2): The mean dosage of propranolol was equivalent to <33% of the effective dosage, whereas patients receiving metoprolol received (on average) the equivalent of 50% of the effective dosage. Finally, the only variable that predicted the use of propranolol (rather than metoprolol or atenolol) was the use of diuretic drugs. Age >70 years Use of diuretic drugs 0.62 (0.50-0.87):I: 0.66 (0.50-0.88)~: 0.76 (0.62-0.93)§ 0.64 (0.4%0.88)§ LVEF <30% Transient heart failure An odds ratio value <1 denotes that the respective variable predicted failure to prescribe beta-blockers: *p < 0.0001. tPersistent heart failure despite treatment would classify a patient as having a contraindication to beta-blocker therapy. ;p < 0.005. §p < 0.05. liP - 0.07; all other variables tested (see Methods) did not significantly predict the use of beta-blockers. LVEF = left ventricular ejection fraction; PTCA - percutaneous transluminal coronary angioplasty. Discussion Although beta-blockers should be part of the standard long-term treatment after a myocardial infarction (3,4), roughly 50% of >600 patients surviving a myocardial infarction in three countries were discharged without such treatment. These figures are similar to those reported in multicenter trials (7,8). However, the main finding in our study is that failure to recommend beta-blockers at the time of hospital discharge is typically not due to clear contraindications. More- Table 2. Percent of Effective Dosage of Beta-Blockers Administered to Infarct Survivors Without Contraindications Percent of Effective Dosage* (mean _+ SD) Univariate Analysis City Tct Aviv Syracuse, New York Mexico City Type of beta-blocker Metoprolol Propranolol Atenolol 42 _+27] 60 -+ 55 44 _+ 18] p < 0.01 p < 0.05 52 _+ 28] 31 _+ 21 65 + 571 p < 0.0005 p < 0.0005 Multivariate Analysis (stepwise regression) Type of beta-blocker p < 0.0001 *See Methods for definition of effective dosage. No other variable tested (Table 1) correlated significantlywith the prescribed dosage of beta-blocker. 1330 V1SKIN ET AL. BETA-BLOCKERS A F T E R M Y O C A R D I A L INFARCTION over, many of the patients not receiving beta-blockers belong to patient subgroups that would derive the greatest benefit from such treatment. Finally, even when beta-blockers are prescribed, the dosages used are considerably smaller than those proved to be effective by prospective trials, with only 6% of infarct survivors receiving effective dosages. What are effective dosages of beta-blockers? We defined as effective only those dosages proved to be effective in reducing mortality in prospective, randomized, double-blind placebocontrolled trials (9,14,15). It is possible that lesser dosages are also effective in prolonging survival after infarction, but this hypothesis remains to be proved. According to our definition, dosages of metoprolol, 200 rag/day (14), and propranolol, 160 rag/day (15), represented effective doses. However, higher dosages of propranolol (180 to 240 rag/day) were prescribed to the majority of patients in the Beta-blocker Heart Attack Trial (9). Thus, we may have overestimated the low percent of patients receiving effective dosages of propranolol in our study. Nine percent of patients in our study received atenolol. For these patients, we considered effective a dosage of 100 rag/day, a regimen that has been found (17) to have effects on the 1-year survival of infarct survivors comparable to those of 160 mg/day of propranolol. However, those data come from a small study with a high withdrawal rate (17). Also, 100 rag/day of atenolol decreased the 1-year cardiovascular mortality in the ISIS-I study (18), but the randomization period in that study was limited to the in-hospital period. In fact, only 35% of patients in ISIS-1 received long-term treatment with betablockers. Therefore, our definition of 100 rag/day of atenolol as effective dosage was based mainly on published data on "equipotency" with propranolol and metoprolol (19-21). However, these equipotency data were derived from the drugs' effects on blood pressure (19) and on tachycardia (induced by exercise [19,20] or isoproterenol infusion [21]) and do not necessarily apply to postinfarction patients. Why are so many infarct survivors discharged without beta-blocker therapy? Only a minority of infarct survivors have clear contraindications to beta-blocker treatment. Such patients comprised only 18% of our study group and of those in the largest beta-blocker trials (9,10). If diabetes and peripheral vascular disease are added to the list of contraindications, up to 27% of infarct survivors may be considered to have contraindications (22). However, published data suggest that infarct survivors with these conditions should not be deprived of the potential benefits of beta-blocker treatment. Although some studies (10,14) excluded patients with severe intermittent claudication, peripheral vascular disease itself was not a contraindication to enrollment in large beta-blocker trials (9,14). Yet symptomatic deterioration of peripheral vascular disease as a reason for drug discontinuation was not more common in patients receiving beta-blockers than in those receiving placebo (9,14,23). Moreover, reduction of mortality and reinfarction rates by beta-blocker treatment appears to be especially pronounced in diabetic patients (24-27). In our study, only 58% of infarct survivors without contra- JACC VoI. 25, No. 6 May 1995:1327-32 indications to beta-blockers were receiving these drugs. Predictors of failure to prescribe beta-blockers included the presence of impaired left ventricular function (as indicated by treatment with diuretic agents, transient or controlled heart failure or left ventricular ejection fraction <30%) and increased patient age. It is plausible that physicians avoid recommending beta-blockers to patients with impaired left ventricular function and to elderly patients, mainly because of their concern for potential iatrogenic complications. These observations deserve further comment. Infarct survivors with impaired left ventricular function are less likely to receive beta-blockers. Is that justifiable? Our results are in accordance to the report by Lichstein et al. (11) on the use of beta-blockers in a multicenter trial. In that study (11), the percent of infarct survivors receiving beta-blockers ranged from 57% among patients with good left ventricular function to 21% among patients with a left ventrieular ejection fraction <30%. The danger of causing overt heart failure with beta-blockers appears to be overestimated: The rate of precipitation of heart failure of enough severity to warrant drug discontinuation was <5% in the large beta-blocker trials (9,10,14). Even among infarct survivors with marked cardiomegaly (28) or with a history of congestive heart failure (23), clinical heart failure was rarely precipitated (in 8% and 15% of patients, respectively) and was not more common than in patients treated with placebo (23,28). In fact, some data (11) suggest that betablocker treatment of postinfarction patients with impaired ejection fraction may prevent, rather than precipitate, the development of clinical heart failure. Finally, by withholding beta-blocker treatment from patients with impaired left ventricular function, we may be depriving the very patients who have the most to gain from such therapy (2,28,29). The large prospective beta-blocker trials did not provide data on the ejection fraction of randomized patients (9,10,14). However, other variables that correlate with large infarcts (i.e., higher serum enzyme levels [14] or cardiomegaly [9,10] invariably correlated with a greater absolute reduction in mortality with beta-blocker therapy (9,10,14). For example, in the Norwegian Multicenter Study, 2 lives were saved for each 100 patients with normal heart size treated with timolol, whereas among patients with cardiomegaly, 10 lives were saved per 100 patients treated (28). Should elderly patients be treated with beta-blockers after myocardial infarction? Physicians seem to be reluctant to prescribe beta-blockers to elderly patients (6,12). In our study only 38% of infarct survivors without contraindications to beta-blockers who were ->70 years old received these agents, whereas 68% of similar younger patients received such treatment. Although the value of beta-blockers for improving survival in elderly infarct survivors remains to be proved (prospective beta-blocker trials excluded patients >70 (9,14,15) or 75 (10,16,30) years old, subgroup analysis of most prospective trials does not suggest a decreased benefit from beta-blockade with increasing age (9,10,14,16). In fact, it is the youngest JACC Vol. 25, No. 6 May 1995:1327-32 patients (those <50 [2], <60 [23] or <65 [14] years old) who may, because of their generally good prognosis, derive the smallest benefit from beta-blocker treatment. Finally, use of beta-blockers was the best predictor of survival among patients who were >70 years of age at the time of myocardial infarction in a nonrandomized study (12), and a trend toward increased survival with beta-blocker use was also reported for patients >75 years old (13). Bradycardia and symptomatic peripheral vascular disease seem to be the only adverse effects of beta-blockers more common with increasing age (31). Therefore, with close followup, increased age should not be viewed as a contraindication to beta-blockade (31). Only a minority of infarct survivors receive effective dosages of beta-blockers. To our knowledge, there have been no previous published data on the dosages of beta-blockers commonly prescribed after infarction. Our observation that only 6% of patients received a dosage equivalent to those proved effective in preventing death after infarction should be confirmed by further studies. The only independent predictor of prescription of a low dosage was the type of beta-blocker used: Patients receiving propranolol received a significantly lower dosage. This trend was apparently influenced by the dose of beta-blockers available in tablets: A 10 mg tablet of propranolol is equivalent to only 6% of the effective dosage (32). In contrast, patients receiving the smallest metoprolol dose available in tablets (i.e., 50 mg [32]) are receiving 25% of the effective daily dosage. Our study did not examine why physicians prefer one beta-blocker over another. It is possible that propranolol was preferred for patients conceived to be at higher risk for adverse effects, as suggested by the more common use of propranolol (rather than other beta-blockers) among patients receiving diuretic agents. Limitations and clinical implications of our study. Our study focused on the clinical practices of four hospitals in three countries, and the data may not apply to the treatment of infarct survivors elsewhere. However, the percent of infarct survivors receiving beta-blockers in our study was very similar to that reported in large studies (7,8,33). Also, we limited our evaluation of drug treatment to that recommended at the time of hospital discharge; thus, it is possible that more betablockers were given during follow-up visits. However, in the European Cooperative Study (8), the percent of infarct survivors receiving beta-blockers at 3 months and 1 year after infarction was essentially that reported at the time of hospital discharge. In addition, a recent survey of treatment practices in England (22), indicated that family physicians were administering beta-blockers to only 39% of infarct survivors without contraindications. Therefore, we believe that our results regarding the underuse of beta-blockers after myocardial infarction represent common clinical practice and identify a major gap between what we have learned from prospective trials and current treatment of patients. This gap ought to be closed by continuing medical education. Alternatively, prospective studies should be made of infarct survivors randomized to receive VISK1N ET AL. BETA-BLOCKERS AFTER MYOCARDIAL INFARCTION 1331 either the "effective dosage" defined by large clinical trials or the relatively low dosage of beta-blockers commonly used. References 1. Yusuf S, Peto R, Lewis J, Collins R, Sleight P. Beta blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis 1985;27:335-71. 2. The Beta-blocker Pooling Project Research Group. The Beta-Blocker Pooling Project (BBPP): subgroup findings from randomized trials in postinfarction patients. Eur Heart J 1988;9:8-16. 3. Moss AJ. Benhorin J. Prognosis and management after a first myocardial infarction. N Engl J Med 1990;322:743-53. 4. Yusuf S, Sleight P, Hcld P, McMahon S. Routine medical management of acute myocardial infarction. Lessons from overviews of recent randomized controlled trials. Circulation 1990;82(Suppl I1):II-117-34. 5. Lau J, Antman EM, Jimenez-Silva J, Kupelnick B, Mosteller F, Chalmers TC. Cumulative meta-analysis of the therapeutic trials for myocardial infarction. N Engl J Meal 1992;327:248-54. 6. Gurwitz JH, Goldberg RJ, Chen Z, Gore JM, Alpert JS. Beta-blocker therapy in acute myocardial infarction: evidence of underutilization in the elderly. Am J Med 1992;93:605-10. 7. The Multicenter Diltiazem Postinfarction Trial Research Group. The effect of diltiazem on mortality and reinfarction after myocardial infarction. N Engl J Mcd 1988;319:385 92. 8. Arnold AER, Simoons ML, Van de Werf F, et al, for the European (ooperative Study Group. Recombinant tissue-type plasminogen activator and immediate angioplasty in acute myocardial infarction. One year followup. Circulation 1992;86:111-20. 9. Bcta-blocker Heart Attack Trial Research Group. A randomized trial of propranolol in patients with acute myocardial infarction. MortaliW results. JAMA 1982;247:1707-14. 10. The No~'egian Multicenter Study Group. Timolol-induced reduction in mortality and rcinfarction in patients surviving acute myocardial infarction. N Engl J Med 1981;304:81)I-7. 11. Lichstein E, Hager D, Gregory JJ, Fleiss JL, Rolnitzky LM, Bigger JT, for the Multicenter Diltiazem Post-Infarction Research Group. Relation between beta-adrenergic blocker use, various correlates of left ventricular function and the chance of developing congestive heart failure. J Am Coll Cardiol 1990;16:1327-32. 12. Montague T J, lkuta RM. Wong RY, Bay KS, Teo KK, Davies NJ. Comparison of risk and patterns of practice in patients older and younger than 70 ycars ~ith acute myocardial infarction in a two year period (1987-1989). Am J Cardiol 1991;68:843-7. 13. Smith SC. Gilpin E, Ahnvc S, Dittrieh H, Nicod P, Hcnning H, ct al. Outlook after acute myocardial infarction in the ve~' elderly compared to that in patients aged 65 to 75 years. J Am Coll Cardiol 1990;16:784-92. 14. Olsson G, Rehnqvist N, Sjogrcn A, Erhardt L, Lundman T. Long-term treatment with metoprolol after myocardial infarction: effect on 3 year mortality and morbidity. J Am Coil Cardiol 1985;5:1428-37. 15. ttansteen V, Moinichen E, Lorentsen E, et al. One year's treatment with propranolol after myocardial infarction: preliminary report of Norwegian multicenter trial. BMJ 1982;284:155-61). 16. Hjalmarson A, Elmfeldt D, Herlitz J, et al. Effect on mortaliD' of metoprolol in acute myocardial infarction: a double blind randomized trial. Lancet 1981;2:823-7. 17. Wilcox RG, Roland JM, Banks DC, Hampton JR, Mitchell JRA. Randomized trial comparing propranolol with atenolol in immediate treatment of suspected myocardial infarction. Br Med J 1981);280:885-8. 18. ISIS-I (First International Study of Infarct Survival) Collaborative Group. Randomized trial of intravenous atcnolol among 16 027 cases of suspected acute myocardial infarction: ISIS-1. Lancet 1986;2:57-67. 19. Wilcox RG. Randomized study of six beta-blockers and a thiazide diuretic in essential hypertension. Br Med J 1978;2:383-8. 20. Tantucci C, Bruni B, Dottorini ML, et al. Comparative evaluation of cardinsclectivity of metoprolol OROS and atcnolol: a double blind, placebocontrolled crossover study. Am Heart J 1990;120:467-72. 21. Waal Maning HJ. Hypertension: which beta-blocker? Drugs 1976;12:412-41. 22. Eccles M, Bradshaw C. Use of secondary prophylaxis against myocardial infarction in the north of England. Br Med J 1991;302:91 2. 1332 VISKIN ET AL. BETA-BLOCKERS AFTER MYOCARDIAL INFARCTION 23. Beta-blocker Heart Attack Trial Research Group. A randomized trial of propranolol in patients with acute myocardial infarction. I1. Morbidity results. JAMA 1983;250:2814-9. 24. Kjekshus J, Gilpin E, Cali G, Blackey AR, Henning H, Ross J. Diabetic patients and beta-blockers after acute myocardial infarction. Eur Heart J 1990;11:43-50. 25. Malmberg K, Herlitz J, Hjalmarson A, Ryden L. Effects of metoprolol on mortality and late infarction in diabetics with acute myocardial infarction. Retrospective data from two large studies. Eur Heart J 1989;10:423-8. 26. Rodda BE for the Norwegian Multicenter Study Group. The timolol myocardial infarction study: an evaluation of selected variables. Circulation 1983;67(Suppl I):1-101-6. 27. Furberg CD, Byington RP for the BHAT Research Group. What do the subgroup analyses reveal about differential responses to beta-blocker therapy? The Beta-blocker Heart Attack Trial experience. Circulation 1983; 67(Suppl I):I-98-101. 28. Gundersen T. Influence of heart size on mortality, and reinfarction in JACC Vol. 25, No. 6 May 1995:1327-32 29. 30. 31. 32. 33. patients treated with timolol after myocardial infarction. Br Heart J 1983; 50:135-9. Chadda K, Goldstein S, Byington R, Curb D. Effect of propranolol after acute myocardial infarction in patients with congestive heart failure. Circulation 1986;73:503-10. Boisse JP, Leizorovicz A, Picolet H, Peyrieux JC, for the APSI Investigators. Secondary prevention after high-risk acute myocardial infarction with low dose acebutolol. Am J Cardiol 1990;66:251-60. Gundersen T, Abrahamsen AM, Kjekshus J, Ronnevik PK, for the Norwegian Multicenter Study. Timolol related reduction in mortality and reinfarction in patients aged 65-75 years surviving acute myocardial infarction. Circulation 1982;66:1179-84. Physicians' Desk Manual. 47th ed. New Jersey: Medical Economics Comp. Inc; 1992. Pashos CL, Normand SLT, Garfinkle JB, Newhouse JP, Epstein AM, McNeil BJ. Trends in the use of drug therapies in patients with acute myocardial infarction: 1988 to 1992. J Am Coll Cardiol 1994;23:1023-30.