* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download module #25 congestive heart failure
Coronary artery disease wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Electrocardiography wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Heart failure wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
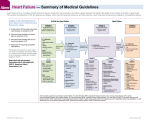
Facilitator version MODULE #25 CONGESTIVE HEART FAILURE Created by Dr. Manish Sharma 01/31/2014 OBJECTIVES: 1. 2. 3. 4. 5. 6. Understand the definition and classification of heart failure Be able to initiate initial diagnostic evaluation in heart failure Understand the role of BNP or NT-proBNP in the evaluation and treatment of heart failure Understand the guideline-directed medical therapy (GDMT) for heart failure Understand device therapy for heart failure Understand treatment options for end-stage heart failure REFERENCES: 1. ACCF/AHA Practice Guideline: 2013 ACCF/AHA Guideline for the Management of Heart Failure: Executive Summary 2. McMurray, John J.V. “Systolic Heart Failure.” N Engl J Med 2010; 362: 228-238. January 21, 2010. 3. Aurigemma, Gerard P and Gaasch, William H. “Diastolic Heart Failure.” N Engl J Med 2004; 351: 1097-1105. September 9, 2004. CASE *M.J. is a 55 year-old African American male with past medical history of Hypertension and Diabetes Mellitus type 2 who presents to the ED with one month history of progressively worsening shortness of breath and lower extremity swelling. Previously, he had no limitations in activity. Now, he gets short of breath with walking to the bathroom or climbing one flight of stairs. He also notes worsening breathing when lying in bed and has been waking up at night due to shortness of breath. He does not report any fever, chills, palpitations, chest pain, cough, nausea or vomiting. He smokes one pack of cigarettes per day. He has not taken his Hydrochlorothiazide and Metformin, regularly. Three months ago, his hemoglobin A1c was 11%. His father suffered a heart attack at the age of 50. On physical examination, he appears comfortable sitting up right at rest. His blood pressure is 155/95 mm Hg. His heart rate is 85 bpm, regular. His respiratory rate is 18 per minute. He is afebrile. His BMI is 32. His oxygen saturation is 85% on room-air and this improves to 94% on 2 LPM via NC. Neck exam demonstrates elevated JVP. Auscultation of the chest demonstrates rales posteriorly in the lower onethird of the lung fields. Cardiac exam demonstrates normal S1 and S2. There is S3 present. There is also a II/VI systolic ejection murmur at the lower left sternal border radiating to the axilla. Abdomen is soft and no tenderness is palpated. There is 2+ pitting edema of the legs extending to the knees. What is the most likely diagnosis? --The most likely diagnosis is acute decompensated heart failure (ADHF). Heart failure (HF) is a complex clinical syndrome that results from any structural or functional impairment of ventricular filling or ejection of blood. The cardinal manifestations of HF are dyspnea and fatigue, which may limit exercise tolerance, and fluid retention, which may lead to pulmonary and/or splanchnic congestion and/or peripheral edema. HF is largely a clinical diagnosis based on careful history and physical examination. There is no single diagnostic test for HF. EF is considered important in classification of patients with HF because of prognosis, response to therapies and because most clinical trials selected patients based on EF. TABLE 1: Definition of HFrEF and HFpEF Classification EF (%) Description I. Heart failure with Also referred to as systolic HF. Randomized controlled trials have mainly enrolled patients reduced ejection fraction ≤40 with HFrEF, and it is only in these patients that efficacious therapies have been (HFrEF) demonstrated to date. Also referred to as diastolic HF. Several different criteria have been used to further define II. Heart failure with preserved ejection fraction (HFpEF) ≥50 HFpEF. The diagnosis of HFpEF is challenging because it is largely one of excluding other potential noncardiac causes of symptoms suggestive of HF. To date, efficacious therapies have not been identified. 41 a. HFpEF, borderline to 49 These patients fall into a borderline or intermediate group. Their characteristics, treatment patterns, and outcomes appear similar to those of patients with HFpEF. It has been recognized that a subset of patients with HFpEF previously had HFrEF. These b. HFpEF, improved >40 patients with improvement or recovery in EF may be clinically distinct from those with persistently preserved or reduced EF. Further research is needed to better characterize these patients. EF indicates ejection fraction; HF, heart failure; HFpEF, heart failure with preserved ejection fraction; and HFrEF, heart failure with reduced ejection fraction. Which tests would you order at this time? --CBC, UA, Serum electrolytes (including Calcium and Magnesium), BUN, Serum Creatinine, Glucose, Fasting lipid profile, LFTS, TSH, BNP or NT-proBNP, Troponin I, Hemoglobin A1c . --ECG (12-lead), CXR, and Two-dimensional Echocardiogram with Doppler flow What is the role of BNP or NT-proBNP in the evaluation and treatment of heart failure? --It is useful in supporting clinical decision making regarding the diagnosis of HF, especially in the setting of clinical uncertainty. --It is useful for establishing prognosis or disease severity in chronic HF or ADHF. --It is useful in achieving optimal dosing of guideline-directed medical therapy (GDMT) in select clinically euvolemic patients followed in a well-structured HF disease management program. What is his NYHA functional class and what is his ACCF/AHA stage? --M.J. is in NYHA functional class III and ACCF/AHA stage C. Table 2: Comparison of ACCF/AHA Stages of HF and NYHA Functional Classifications ACCF/AHA Stages of HF A B At high risk for HF but without structural heart disease or symptoms of HF Structural heart disease but without signs or symptoms of HF NYHA Functional Classification None I I C Structural heart disease with prior or current symptoms of HF II III IV No limitation of physical activity. Ordinary physical activity does not cause symptoms of HF. No limitation of physical activity. Ordinary physical activity does not cause symptoms of HF. Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in symptoms of HF. Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity causes symptoms of HF. Unable to carry on any physical activity without symptoms of HF, or symptoms of HF at rest. D Refractory HF requiring specialized interventions IV Unable to carry on any physical activity without symptoms of HF, or symptoms of HF at rest. ACCF indicates American College of Cardiology Foundation; AHA, American Heart Association; HF, heart failure; and NYHA, New York Heart Association *CBC/CHEM 10 (including creatinine) normal. Glucose is 230 mg/dL. TSH nl. Troponin I normal. LFTS normal. Hemoglobin A1c is 12%. NT-proBNP is 12,000 pg/mL. Total cholesterol is 230 mg/dL, LDL 150 mg/dL, Triglycerides 315 mg/dL and HDL 25 mg/dL. UA is normal except for glycosuria. ECG shows q waves in the inferior leads. CXR shows diffuse increased interstial opacities, including kerley B lines; prominent and indistinct pulmonary vasculature and tiny pleural effusions. Echocardiogram shows normal LV size. There is inferior and lateral wall hypokinesis. LVEF is 35%. What are the immediate goals of treatment? --The immediate goals of treatment are to improve symptoms due to fluid retention, initiate guidelinedirected medical therapy (GDMT), and to evaluate for the etiology of ADHF. *You have admitted M.J. to the cardiac monitoring unit. He is treated with IV Lasix and started on Lisinopril. His dyspnea and lower extremity edema improves. Discuss the role of diuretics in the treatment of ADHF? --Diuretics are used to improve symptoms of fluid retention. Loop diuretics are the most frequently used type of diuretic. Loop diuretic can be augmented with thiazide diuretic if needed. Discuss the role of angiotensin converting enzyme inhibitors (ACE-Is)/angiotensin receptor blockers (ARBs) in the treatment of HF? --ACE-Is are indicated for all patients with HFrEF regardless of functional status (NYHA) or symptom status (CONSENSUS 1987, SOLVD-T 1991). ARBs can be substituted in patients who are intolerant to ACE-Is (CHARM 2003). ACE-Is/ARBs should be gradually titrated to target doses shown to reduce morbidity and mortality in clinical trials. Routine laboratory monitoring for hyperkalemia and kidney function is indicated after initiating or increasing the dose of ACE-Is/ARBs. --The ARB, Candesartan, is an agent that has been studied in a large RCT of HFpEF treatment and was associated with a reduction in hospitalization (CHARM-Preserved). What are some of the common causes of heart failure? --Myocardial ischemia, valvular heart disease, infections of myocardium (viral or bacterial), hypothyroidism, and infiltrative cardiac diseases such as hemochromatosis and amyloidosis are a few of the causes of HF. *Now his symptoms have resolved. He is ambulating in the hallways without dyspnea or any limitations. He is started on Metoprolol Succinate XR. Discuss the role of B-blockers in the treatment of HF --Like ACE-Is, B-blockers are indicated for all patients with HFrEF regardless of functional class (NYHA) or symptom status. B-blockers (Metoprolol Succinate extended release (MERIT-HF 1999), Carvedilol (COPERNICUS 2001), and Bisoprolol (CIBIS-2 1999)) have proven to show morbidity and mortality benefit in heart failure treatment trials. B-blockers should not be initiated in the setting of heart failure with decompensation. B-blockers should be gradually titrated to target doses shown to reduce morbidity and mortality in clinical trials. *M.J. undergoes a cardiac catheterization which shows multi-vessel CAD and he gets a CABGx3V prior to discharge. He is discharged from the hospital on Asprin, Lasix, Lipitor, Lisinopril, Metoprolol Succinate XR, Glargine and Aspartate insulin. He is given instructions on low-fat, low-cholesterol and no added salt diet. He is given instructions on monitoring for symptoms of heart failure. He is taught to monitor his weight at home. He is advised to stop smoking. He follows up one week after hospital discharge in the CHF clinic. He is doing well and has no symptoms. His heart failure medications are titrated to target doses. *Five years later, M.J. presents to the ED with two days of worsening dyspnea. He is admitted to the hospital with the diagnosis of NSTEMI and ADHF. He undergoes another cardiac catheterization and is now found to have non-revascularizable vessels. His ECG now shows NSR, a new LBBB with a QRS interval of 150 mseconds. His Echocardiogram now shows anteroapical and inferolateral wall hypokinesis with LVEF of 25%. Discuss the role of Aldosterone receptor antagonists in the treatment of HFrEF --Addition of aldosterone receptor antagonist, Spironolactone, to standard therapy in HFrEF and NYHA class III-IV results in reduction in mortality, hospitalization and improved NYHA functional class (RALES 1999). --Eplerenone is a selective aldosterone receptor antagonist with less chance of gynecomastia but is more expensive. Eplerenone is approved for treatment of HF after acute MI (EPHESUS 2003). However, recent studies have demonstrated reduction in mortality and hospitalization in treatment of HFrEF and NYHA II functional status when added to standard therapy. *M.J. is treated for NSTEMI and ADHF. He is discharged from the hospital on Epeleronone, Lasix, Asprin, Plavix, Lipitor, Lisinopril, Metoprolol Succinate XR, Glargine and Aspartate insulin. He remains symptomatic with minimal exertion despite maximal medical therapy. *What is M.J’s Seattle Heart Failure Survival score? --Seattle Heart Failure Model is a validated tool which predicts prognosis for patients with HF and the degree to which it is altered with certain pharmacological or mechanical interventions. M.J’s five year survival is calculated to be 70% with the characteristics described in appendix 1: *Are there any other medications for HFrEF that M.J. would benefit from? --The addition of Isosorbide dinitrate and Hydralazine to standard therapy in African-American patients with HFrEF and NYHA class III-IV results in reduction in mortality, readmission for HF, and improvement in the quality of life (A-HeFT 2004). --Digoxin is another option. It reduces symptoms in patients with HFrEF and also decreases rates of hospitalization (DIG 1997). -- For summary, see Table 3 in appendix 1. Is there any device that M.J. could benefit from? --If M.J. continues to have symptoms while on chronic GDMT then he may benefit from CRT-ICD (cardiac resynchronization therapy with biventricular pacing and implantable cardioverter-defibrillator). Implantable cardioverter-defibrillator (ICD) is indicated in selected patients (cardiomyopathy with LVEF <= 35% and NYHA II or III symptoms on chronic GDMT with expected survival of more than one year) for prevention of sudden cardiac death and to reduce total mortality (SCD-HeFT 2005). Cardiac resynchronization therapy (CRT) has shown to reduce mortality, hospitalization and improvement in functional class in selected patients (cardiomyopathy with LVEF <=35%, NSR with LBBB and QRS duration >= 150mseconds and NYHA II, III or ambulatory IV symptoms on chronic GDMT (COMPANION 2004, CARE-HF 2005, MADIT-CRT 2009). Discuss treatment options for patients with end-stage heart failure? --Left-Ventricular Assist Devices (LVADs) have been used in carefully selected patients with end-stage heart failure who are not candidates for cardiac transplantation to improve overall survival and quality of life, so called destination therapy (REMATCH 2001). LVADs have been used as a bridge to cardiac transplantation in end-stage heart failure patients. --Cardiac Transplantation --Palliative care and hospice to establish patient’s end-of-life goals and improve quality of life MKSAP 16 QUESTIONS: #15—Treat HFpEF – Answer A #17—Treat HFrEF with B-blocker therapy- Answer C #24—Treat HFrEF with Spironolactone – Answer B #36—Treat HFrEf – Answer D #54—Treat HFrEf with device therapy – Answer A #58—Treat ADHF with diuretic therapy – Answer B #75—Treat HFrEf by referral for evaluation for mechanical circulatory support and cardiac transplantation – Answer C #80—Hospital discharge after treatment of ADHF – Answer A #97—Treat HFrEF (Asymptomatic/NYHA functional class I-II) – Answer B #102—Treat HFrEF with hydralazine-isosorbide dinitrate – Answer C #120—Treat HTN in a patient with HFrEF – Answer A Appendix 1: Below is the guideline directed medical therapy (GDMT) and the magnitude of benefit demonstrated in RCTs: Table 3: Medical Therapy for Stage C HFrEF: Magnitude of Benefit Demonstrated in RCTs GDMT RR Reduction in Mortality (%) NNT for Mortality RR Reduction Reduction in HF Hospitalizations (Standardized to 36 mo) (%) ACE inhibitor or ARB 17 26 31 Beta blocker 34 9 41 30 6 35 43 7 33 Aldosterone antagonist Hydralazine/nitrate ACE indicates angiotensin-converting enzyme; ARB, angiotensin-receptor blocker; GDMT, guideline-directed medical therapy; HF, heart failure; HFrEF, heart failure with reduced ejection fraction; NNT, number needed to treat; RCTs, randomized controlled trials; and RR, relative risk. Adapted with permission from Fonarow et al.201 Post Module Evaluation Please place completed evaluation in an interdepartmental mail envelope and address to Dr. Wendy Gerstein, Department of Medicine, VAMC (111) or give to Dr. Patrick Rendon at UNM Hospital. 1) Topic of module:__________________________ 2) On a scale of 1-5, how effective was this module for learning this topic? _________ (1= not effective at all, 5 = extremely effective) 3) Were there any obvious errors, confusing data, or omissions? Please list/comment below: ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________ 4) Was the attending involved in the teaching of this module? Yes/no (please circle). 5) Please provide any further comments/feedback about this module, or the inpatient curriculum in general: 6) Please circle one: Attending Resident (R2/R3) Intern/extern Medical student