* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Electroconvulsive Therapy
Mental disorder wikipedia , lookup
Diagnostic and Statistical Manual of Mental Disorders wikipedia , lookup
Child psychopathology wikipedia , lookup
Psychiatric and mental health nursing wikipedia , lookup
Classification of mental disorders wikipedia , lookup
Conversion disorder wikipedia , lookup
Glossary of psychiatry wikipedia , lookup
Dissociative identity disorder wikipedia , lookup
Mental status examination wikipedia , lookup
Narcissistic personality disorder wikipedia , lookup
Community mental health service wikipedia , lookup
Generalized anxiety disorder wikipedia , lookup
Deinstitutionalisation wikipedia , lookup
History of psychosurgery in the United Kingdom wikipedia , lookup
Major depressive disorder wikipedia , lookup
Emergency psychiatry wikipedia , lookup
Bipolar II disorder wikipedia , lookup
Moral treatment wikipedia , lookup
History of mental disorders wikipedia , lookup
History of psychiatry wikipedia , lookup
Abnormal psychology wikipedia , lookup
History of psychiatric institutions wikipedia , lookup
Electroconvulsive therapy wikipedia , lookup
Controversy surrounding psychiatry wikipedia , lookup
David J. Impastato wikipedia , lookup
History of electroconvulsive therapy in the United Kingdom wikipedia , lookup
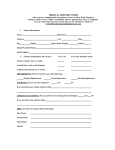
Electroconvulsive Therapy: Its Safety, Efficacy, and Role in Mental Health Tiffany Moore, MSN, APRN, FNP-C; Rhea Ferry, DNP, APRN, FNP Contributor: Billie Madler, DNP, APRN, FNP-C INTRODUCTION ECT SAFETY BURDEN OF MENTAL HEALTH • NIH reports 26.2% of U.S. population 18 and older has a diagnosable mental health disorder • Mortality is 0.19 per 10,000 • No absolute contraindications • Relative risk factors • 20.9 million Americans have a mood disorder (depression, bipolar disorder and dysthymic disorder) • Half with a mental health disorder meet diagnostic criteria for two mental health disorders • Numerous treatment option Psychotherapy Medications Those with cardiovascular disease have been treated with ECT safely. However, cardiology consult prior to ECT beneficial. Those with cerebrovascular disease may benefit from neurology consult prior to treatment. ECT causes a transient increase in cerebral blood flow to some parts of the brain and a transient increase in intracranial pressure Brain stimulation treatment, such as electroconvulsive therapy Transcranial magnetic stimulation or vagal nerve stimulation ELECTROCONVULSIVE THERAPY • Depression ranked fourth in disease burden, expected to rise to second by 2020 • Many patient are unresponsive or intolerant to pharmacologic measures • Bipolar disorder is the 12th most common diagnosis by WHO2.4 million people diagnosed with schizophrenia INDICATIONS/EFFICACY OF ECT • Electroconvulsive therapy (ECT) Introduced in 1938 by Ugo Cerletti, an Italian neurologist • Depression Usually used 2nd line Should be consider for 1st line treatment in: • Electrodes, on one or both sides of the head, sends a measured charged electrical current through brain • Purpose of ECT is to produce a generalized cerebral seizure with a bilateral tonic-clonic convulsion. • Controversial despite being safe and effective • 150,000 ECT treatment per year • In use for 75 years Crude history Unknown cognitive effects Uncertain mechanism of action ECT COMPLICATIONS • • • • Performed different that in the past Vitals are monitored EKG and EEG leads for monitoring IV access used to administer sedation and subsequent paralytic Before neuromuscular blockers were used routinely, nearly 30% of ECT patient suffered spinal compression fractures • Mouth guards routine practice • After patient sedated and paralyzed, electrodes are placed • Patients are monitored for 30-60 minutes after an ECT and the majority are able to be discharged home • Complications Confusion and memory problems are the most common complications Headaches and nausea - prophylactic analgesics and antiemetics can reduce Dehydrated, severely malnourished patients Patients with a complicating medical condition Patients presenting with delusional depression Those who have been unresponsive to antidepressants Patients with acute suicidal ideation, catatonia or a major depressive episode with psychotic features Patients who request ECT as first line treatment Can even be considered the first-line treatment in post-stroke depression (PSD), as this disorder can often be resistant to medications Pregnant mothers with severe depression may be candidates Those >65 and who are severely ill typically respond better or faster than patients who are <65 In patients with major depressive disorder, remission rates with ECT are high, especially in those who present with psychotic features • Controversy sustained for several reasons: ECT PROCEDURE Median age 30 Substance abuse and anxiety often comorbidities Incidence greater in women than men Occurs across the lifespan, but is the leading cause of disability in 15-44 years olds • Bipolar/Mania ECT with mania is used when patients are intolerant or refractory to lithium or other anti-manic medications Should be considered earlier when potential of self-harm or harming others, or when symptoms appear life threatening • Schizophrenia ECT not commonly used in the US for schizophrenia, but used in some countries as 1st line CONCLUSIONS • The historical implementation of ECT therapy led to a less favorable perspective of this treatment strategy. There was a period of diminished use of ECT, however, over the last 10 years there has been an increase of ECT use. It may be used as first line therapy in some scenarios. It has been established that ECT has a role in mental health treatment, yet further research is needed.