* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download cardiac AP and basis of ECG 2
Survey
Document related concepts
Transcript
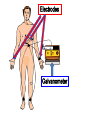
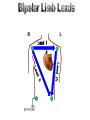
بسم هللا الرحمن الرحيم ﴿و ما أوتيتم من العلم إال قليال﴾ صدق هللا العظيم االسراء اية 58 By Dr. Abdel Aziz M. Hussein Assist Prof. Medical Physiology Pulmonary circuits Heart is the pump Systemic circuits • The heart is a hollow muscular organ Site: • Left side of the thoracic cavity partly behind the sternum. Size and weight: • It is in the size of a man's fist Atria • It weighs about 320 gm in males. • In female it weighs about 250gm. Chambers: Ventricles • 4 chambers = 2 atria + 2 ventricles • Its wall consists of 3 layers; Epicardium Endocardium Myocardium 1. Nodal fibers Atria 2. Conducting fibers Ventricle 3. Contractile fibers Myocardium is composed of 3 types of ms fibers; a) Nodal ms fibers e.g. Sinoatrial (SA) node and Atrioventricular node. • SAN is the normal pacemaker of heart from which the cardiac impulse initiated. b) Conducting ms fibers include AV bundle, bundle branches and Purkinje fibers. • These fibers conduct the cardiac impulse from atria to ventricles. c) Contractile ms fibers • They consist of atria and ventricles. • The primary function of cardiac muscle cell is to contract to pump blood into arteries • Electrical changes within the cardiac muscle cell initiate this contraction. • There are 2 types of membrane potentials on the cardiac muscle cell 1. One during rest called resting membrane potential (RMP) 2. And the second during action called action potential or cardiac impulses • RMP is the potential difference across cell membrane during rest i.e. inside the membrane is negative and outside is positive • Its value differs according to type of muscle fiber e.g. in SAN it is -65 mv, and in ventricle ms is -90 mv • It is measured by galvanometer with 2 microelectrodes one is inserted inside the cell and the other is placed outside the muscle cell • Ionic basis of RMP 1. K+ diffusion to outside (main cause) 2. Na+ diffusion to inside (little effect) 3. Electrogenic Na+-K+ pump • Action potentials occur when the membrane potential suddenly depolarizes and then repolarizes back to its resting state. • So cardiac potential consists of 2 phases; 1. Depolarization phase (inside cell become +ve and outside become –ve) mainly due to Na and Ca influx (inflow inside cell) 2. Repolarization phase (inside cell become -ve and outside become +ve) mainly due to K efflux (outflow outside the cell) RMP Depolarization Repolarization Depolarization phase Repolarization phase • The excitation wave (depolarization followed by repolarization) is initiated by the pace maker of the heart (SAN). • Then it spreads through the atrial fibers in a rapid rate (1m/sec) to converge on the AVN. • The conduction in the AVN is very slow (0.05 m/sec). • The depolarization wave then travels rapidly down the AV bundle, bundle branches (1m/sec) and the purkinje fibers (4m/sec) to all parts of the ventricles. • The body is a good conductor of electricity because tissue fluids have a high concentration of ions that move (creating a current) in response to potential differences. • The potential difference of about 120 mV between a depolarized and a resting area of heart muscle generates in the area of the heart an electric field that projects and conducted to the body surface. • These potential differences can be detected by electrodes put on the skin surface and amplified and recorded as a tracing on paper or on a monitor Def. •ECG is a record of the electrical activities of the cardiac muscle •Apparatus: •The apparatus used for recording the electrical activities of the heart is called electrocardiograph or ECG •ECG apparatus consists of; 1. Recording galvanometer 2. Electrodes Electrodes Galvanometer ◊ Def., •It is the particular arrangement of 2 electrodes of the ECG galvanometer. ◊ Types : Bipolar Limb leads Unipolar leads They measure the potential difference between 2 limbs at different levels of potential. 1. Lead I (RA (-) and LA (+)) 2. Lead II (RA (-) and LF (+)) 3. Lead III (LA (-) and LF (+)) Lead I •Einthoven`s triangle is an equilateral triangle, the sides of which represent the 3 bipolar leads & the heart lies in its centre. •Einthoven`s law the sum of voltage in lead I and Lead III = voltage in lead II Lead I Lead II Lead III V leads + VR + VL + ECG Central t. - •They measure the potential at one point. •The potential at one pole (-ve) of ECG is made zero by connecting it to central terminal that receives electordes from (RA, LA, and LF) •Positive pole (exploring electrode may be placed at; 1. Limbs → unipolar limb (VR, VL and VF) 2. Chest → unipolar chest (V1- V6) •They measure the potential at limbs (RA, LA and LF) •The voltage of potentials recorded by these leads is weak, so it must be augmented to form aVR, aVL, and aVL •This done by disconnection of electrode connected to central terminal to limb to be augmented aVR VR + ECG Central term. - V1 V2 V3 V6 V4 V5 MAL MCL AAL •6 unipolar chest leads from V1 to V6. 1. V1 (Rt 4th intercostal space) 2. V2 (Lt 4th intercostal space) 3. V3 (midway between V2 and V4) 4. V4 (Lt 5th intercostal space midclavicular line 5. V5 (Lt 5th intercostal space anterior axillary line ) 6. V6 (Lt 5th intercostal space midaxillary line ) I aVR aVL V1 V2 V3 V4 V5 III II aVF V6 •ECG paper is composed of a number of 1 and 5 mm squares •It calibrated so that, •Each small square (horizontal)= 0.04 sec. •Each small square (vertical )= 0.1 mv • Consists of; 1. Waves (P,Q,R,S,T,U) 2. Segment (S-T segment) 3. Intervals (P-R interval, Q-T interval) R P T Q S U 1- P wave: represents atrial depolarization. 2- QRS complex: represents ventricular depolarization. 3- T wave: represents ventricular repolarization 4- U wave: represents repolarization of papillary muscles • • • • B) S-T segment: normally is isoelectric C) P-R interval: It represents the time of conduction of impulse from SAN to ventricles Normally 0.12 to 0.2 sec • It gives valuable information about; 1) The anatomical orientation of the heart 2) The relative size of the heart chambers. 3) A variety of disturbance of rhythm and conduction. 4) The extent, location and progress of ischemic damage of the myocardium. 5) The effects of altered electrolyte concentrations and drugs •T wave is inverted •Deep Q •S-T segment is not isoelectric i.e. elevated or depressed Remember THANKS