* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Contribution of Choline
Survey
Document related concepts
Transcript
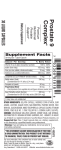
Contribution of Choline-Binding Proteins to Cell Surface Properties of Streptococcus pneumoniae Edwin Swiatlo, Franklin R. Champlin, Steven C. Holman, W. William Wilson and James M. Watt Infect. Immun. 2002, 70(1):412. DOI: 10.1128/IAI.70.1.412-415.2002. These include: REFERENCES CONTENT ALERTS This article cites 25 articles, 13 of which can be accessed free at: http://iai.asm.org/content/70/1/412#ref-list-1 Receive: RSS Feeds, eTOCs, free email alerts (when new articles cite this article), more» Information about commercial reprint orders: http://journals.asm.org/site/misc/reprints.xhtml To subscribe to to another ASM Journal go to: http://journals.asm.org/site/subscriptions/ Downloaded from http://iai.asm.org/ on February 27, 2014 by PENN STATE UNIV Updated information and services can be found at: http://iai.asm.org/content/70/1/412 INFECTION AND IMMUNITY, Jan. 2002, p. 412–415 0019-9567/02/$04.00⫹0 DOI: 10.1128/IAI.70.1.412–415.2002 Copyright © 2002, American Society for Microbiology. All Rights Reserved. Vol. 70, No. 1 Contribution of Choline-Binding Proteins to Cell Surface Properties of Streptococcus pneumoniae Edwin Swiatlo,1* Franklin R. Champlin,2 Steven C. Holman,3 W. William Wilson,3 and James M. Watt2 Department of Medicine, University of Mississippi Medical Center and VA Medical Center, Jackson, Mississippi 39216,1 and Departments of Biological Sciences2 and Chemistry,3 Mississippi State University, Starkville, Mississippi 39762 Nonspecific interactions related to physicochemical properties of bacterial cell surfaces, such as hydrophobicity and electrostatic charge, are known to have important roles in bacterium-host cell encounters. Streptococcus pneumoniae (pneumococcus) expresses multiple, surface-exposed, choline-binding proteins (CBPs) which have been associated with adhesion and virulence. The purpose of this study was to determine the contribution of CBPs to the surface characteristics of pneumococci and, consequently, to learn how CBPs may affect nonspecific interactions with host cells. Pneumococcal strains lacking CBPs were derived by adapting bacteria to a defined medium that substituted ethanolamine for choline. Such strains do not anchor CBPs to their surface. Cell surface hydrophobicity was tested for the wild-type and adapted strains by using a biphasic hydrocarbon adherence assay, and electrostatic charge was determined by zeta potential measurement. Adherence of pneumococci to human-derived cells was assessed by fluorescence-activated cell sorter analysis. Strains lacking both capsule and CBPs were significantly more hydrophobic than nonencapsulated strains with a normal complement of CBPs. The effect of CBPs on hydrophobicity was attenuated in the presence of capsule. Removal of CBPs conferred a greater electronegative net surface charge than that which cells with CBPs possessed, regardless of the presence of capsule. Strains that lack CBPs were poorly adherent to human monocytelike cells when compared with wild-type bacteria with a full complement of CBPs. These results suggest that CBPs contribute significantly to the hydrophobic and electrostatic surface characteristics of pneumococci and may facilitate adherence to host cells partially through nonspecific, physicochemical interactions. Pneumococci express a family of choline-binding proteins (CBPs) which are surface exposed and possibly function as specific adhesins for glycoconjugates on eukaryotic host cells (9, 17). Some members of this family specifically bind the secretory component of immunoglobulin A (10) and complement components (20, 22). Much information about the interaction of CBPs with host proteins or receptors has recently become available, but little is known about how this family of surface proteins contributes to the physical properties of the pneumococcal cell surface. This study was undertaken to examine the contribution of CBPs to the overall hydrophobicity and surface charge of pneumococci. The ability of pneumococci, with or without CBPs, to adhere to human monocytelike cells was also studied. The results suggest that CBPs contribute significantly to the chemistry of the subcapsular compartment of pneumococci and enhance interaction with eukaryotic cells. A possible additional mechanism for the protective effect of capsule polysaccharide is implied. Bacterial strains and media. Pneumococcal strains used in this study have been previously described. Pneumococcal strain D39 is a capsule type 2 clinical isolate (2), and strain Rx1 is a functionally unencapsulated derivative of D39 (19). WU2 is a clinical type 3 isolate (5), and JD908 is an isogenic mutant which produces no detectable extracellular capsule (7). Strain A66 is a capsule type 3 clinical isolate (2), and A66R2 is an unencapsulated mutant (14). All strains were grown at 37°C in Todd-Hewitt broth with 0.5% yeast extract (THY) and frozen at ⫺80°C after supplementation with glycerol to a 20% final concentration. Unadapted pneumococci were grown in chemically defined medium (CDM; JRH Biosciences, Lenexa, Pathogenic bacteria interact with eukaryotic cells by a variety of mechanisms, most notably the specific binding of bacterial adhesins to ligands on the host cell surface. In addition to these specific interactions, the physicochemical properties of the bacterial cell surface can significantly influence the outcome of bacterium-host cell contact. Net cell surface charge and hydrophobicity are two properties of bacterial surfaces which are known to be important in this interaction (3, 13). The polysaccharide capsules of pathogens such as Streptococcus pneumoniae (pneumococcus) are, generally, negatively charged polymers which are thought to protect the bacterial cell from humoral immune mechanisms (11). The net negative charge of capsule polysaccharide may also function to electrostatically repel pneumococci from phagocytic cells, which typically have a net negative charge of ⫺18 to ⫺12 mV at their surface (13, 24). This has been shown for encapsulated group A streptococci (25). In addition to electrostatic interactions, cells may associate by nonspecific hydrophobic interactions. Using adherence to hexadecane droplets, it has been shown that surface proteins of group A streptococci confer a hydrophobic character to the bacterial surface in the absence of capsule (15). Bacterial surfaces with a high degree of hydrophobicity may adhere more efficiently to phagocytes (12), host tissue cells (8), and biomedical materials such as polyethylene (23). * Corresponding author. Mailing address: VA Medical Center, Research and Education (151), 1500 Woodrow Wilson Dr., Jackson, MS 39216. Phone: (601) 984-5560. Fax: (601) 984-5565. E-mail: swed @sprintmail.com. 412 Downloaded from http://iai.asm.org/ on February 27, 2014 by PENN STATE UNIV Received 3 August 2001/Returned for modification 13 September 2001/Accepted 25 September 2001 VOL. 70, 2002 413 FIG. 1. GelCode Blue (Pierce, Rockford, Ill.) stain of SDS-polyacrylamide gel electrophoresis of concentrated culture supernatants from mid-log-phase Rx1 grown in CDM with either choline or ethanolamine. Growth in CDM-EA results in most of the CBPs free in the extracellular medium. Lanes: 1 and 5, molecular size markers (in kilodaltons); 2, CDM-C with no bacterial inoculum, 3, growth in CDM-EA; 4, growth in CDM-C. Cells which were adapted to grow in EA were washed in a 2% choline solution, and the eluate was concentrated 30-fold and was analyzed by SDS-polyacrylamide gel electrophoresis with silver staining. This method has been used as an alternative for eluting CBPs off the pneumococcal surface (28). After adaptation to EA, no stainable proteins could be detected by a choline wash (data not shown). Removal of CBPs results in a significant alteration in the hydrophobic character of the pneumococcal cell surface, which is seen primarily when capsule has been removed (Fig. 2). For strains D39 and A66, removal of CBPs had little effect on the hydrophobicity of the cell surface. Either with or without CBPs, D39 and A66 have very hydrophilic surfaces as observed by their weak adherence to a nonpolar hydrocarbon. In contrast, removal of CBPs from WU2 results in a cell surface which is significantly more hydrophobic, suggesting a contribution of CBPs to the highly hydrated surface of this type 3 strain. Unencapsulated mutants of pneumococci readily demonstrate the contribution of CBPs to cell surface hydrophobicity. For each unencapsulated strain, tested removal of CBPs resulted in greater adherence to hydrocarbon; thus, a more hydrophobic cell surface. The differences between cells with and without CBPs were significant for Rx1 and JD908 (P ⬍ 0.01) but not quite so for A66R2 (P ⫽ 0.064). Cell surface charge for selected strains was examined by measuring zeta potential. The electronegative surface of D39 was mostly unchanged by removing CBPs (Table 1). As was the case in the hydrocarbon adherence assay, removing CBPs in the face of an intact capsule had little effect on the cell surface charge. The exception was WU2, which had significantly more electronegative charge when CBPs were removed. When capsule is removed, the effect of CBPs on cell surface charge is marked. The overall surface charge became more electronegative in the absence of CBPs, as seen by a decrease in surface voltage of more than 10 mV for Rx1 (Table 1). The effect of the full complement of CBPs on adhesion to a human monocyte-like cell line was measured by flow cytometry Downloaded from http://iai.asm.org/ on February 27, 2014 by PENN STATE UNIV Kans.) which was supplemented with choline chloride to a final concentration of 0.02% (CDM-C). Adaptation to ethanolamine (CDM-EA) was done by serially transferring aliquots of pneumococcal cultures growing in CDM in which the choline concentration was decreased in a stepwise manner to a final concentration of ⬍0.0001%, and the ethanolamine concentration was concurrently increased to a final concentration of 0.5% (4). Culture supernatants of pneumococci growing in CDM-C or CDM-EA were passed through a 0.45-m-poresize, low-protein-binding filter, concentrated 30-fold, and analyzed by electrophoresis in 10% polyacrylamide gels after boiling in sodium dodecyl sulfate (SDS) (1). Hydrocarbon adhesion assay. Cell surface hydrophobicity was measured by bacterial adherence to hexadecane with slight modifications to a previously described procedure (16). Bacteria were grown in 5 ml of THY to approximately mid-log phase, collected by centrifugation, and washed twice in phosphate-buffered saline (PBS, pH 7.0). Washed cells were resuspended in 1 ml of PBS, and optical density at 620 nm (OD620) was measured. This measurement served as the control (C0). Subsequently, 200 l of hexadecane was added and the mixture was vortexed for 1 min. After the phases were allowed to separate, the OD620 of the lower aqueous phase was measured (CH). The percent hydrocarbon adherence was determined by the following formula: [(C0 ⫺ CH)/C0] ⫻ 100. Cell surface charge measurement. Net bacterial cell surface charge was measured as the electrical potential of the interface between the bacterial surface and the aqueous environment (zeta potential) (26). The zeta potential was estimated with an automated Zetasizer apparatus (Malvern Instruments, Southborough, Mass.). Exponentially growing pneumococcal cultures in THY were washed twice in PBS (pH 7.0) and resuspended in PBS to an OD620 of 1. Samples were run at 25°C and a field strength of 19.2 V/cm. Other parameters of the Zetasizer were adjusted according to the manufacturer’s specifications. Cell adhesion. Unadapted and EA-adapted pneumococcal cells were washed twice in PBS (pH 7.0) and incubated at 37°C in 10 M 5-chloromethylfluorescein diacetate (CMFDA; Molecular Probes, Inc., Eugene, Oreg.) for 60 min in PBS. Cells were then washed twice in dye-free PBS. Fluorescein-labeled pneumococci were incubated with U937 cells (21) at a ratio of 103:1 (bacteria to cells) for 5 min at 37°C in RPMI medium supplemented with 10% fetal calf serum. After incubation the U937 cells were collected by centrifugation and were then washed and resuspended in Hanks balanced salt solution for analysis by flow cytometry (FACScan; Becton Dickinson, San Jose, Calif.). Differences between means were determined by two-sample t tests. A P value of ⬍0.05 was considered significant. Growth of pneumococci in a defined medium which contains ethanolamine (CDM-EA) as the sole amino alcohol effectively removes most surface-exposed CBPs. These proteins can be detected in concentrated culture supernatants (Fig. 1) from exponentially growing pneumococcal cultures. Bacteria grown in CDM-C release no detectable protein in concentrated culture supernatants, although the limit of sensitivity of the protein stain (10 ng) does not entirely preclude this possibility. Culture medium which contains EA still has an exceedingly small concentration of choline (⬍0.0001%) which may be sufficient for some CBPs to remain attached to the cell surface. NOTES 414 NOTES INFECT. IMMUN. TABLE 2. Mean fluorescence intensity of U937 cells incubated with CMFDA-labeled pneumococci grown in either CDM-C or CDM-EAa Strain Peak channel 2,018.0 2,310.3 30.8 2,017 2,307 29 Rx1 Rx1(A) U937 888.6 14.9 27.2 1,176 11 28 WU2 WU2(A) U937 236.3 84.9 33.6 294 79 32 JD908 JD908(A) U937 2,280.8 479.9 19.0 2,227 478 19 D39 Rx1 U937 480.6 1,267.1 24.8 429 1,186 24 a1 of fluorescently labeled pneumococci incubated with U937 cells for 5 min. This short incubation was necessary to minimize the number of CBPs which would be surface expressed when pneumococci were reintroduced into a choline-containing medium. As seen in Table 2, for most strains grown in CDM-EA the mean fluorescence intensity was significantly less than for the corresponding strain grown with choline. D39 attachment to human cells was unchanged whether bacteria were grown in CDM-C or -EA. When D39 was compared TABLE 1. Net cell surface charge as represented by zeta potentiala Strain Zeta potential (mV) D39 ...........................................................................................⫺11.3 D39(A)1....................................................................................⫺12.3 Rx1............................................................................................⫺13.3 Rx1(A) .....................................................................................⫺23.6 WU2 .........................................................................................⫺33.4 WU2(A) ...................................................................................⫺42.9 a All values are the mean of three independent experiments. 1, Adapted to grow in CDM-EA. , Adapted to grow in CDM-EA; 2, U937 cells with no added bacteria. directly to Rx1 in the same experiment with the same U937 culture, the mean fluorescence with Rx1 was more than 2.5fold greater than that of U937 cells with D39 (Table 2, bottom). Bacteria that colonize or infect humans may simultaneously utilize different mechanisms to maintain close association with host cells. In addition to specific receptor-ligand interactions, the physicochemical properties of bacterial surfaces can modulate the affinity of pathogens for host cells (8, 12, 16). There are more than 90 pneumococcal serotypes, each defined by a chemically distinct polysaccharide capsule. Nearly all of these polymers impart a strong electronegative charge to the cell surface. Pneumococci also express a number of surface-exposed proteins which are noncovalently attached to phosphorylcholine moieties of teichoic and lipoteichoic acids (9). Certainly, some of these proteins may have cognate ligands on eukaryotic cells and function as adhesins. However, data presented here also show that the full complement of CBPs has a profound effect on the physical characteristics of the pneumococcal cell surface. Bacterial cells which do not display CBPs on their surface are significantly more hydrophobic than those which display normal amounts of CBPs. This effect is greatest in pneumococci which lack a capsule, except for strain WU2, in which the CBPs measurably contribute to the hydrophilic character of the cell surface. Pneumococci which lack CBPs also have a more negatively charged cell surface, as measured by zeta potential. Again, this is best measured in unencapsulated strains but is also seen for the fully encapsulated strain WU2. The contribution of the full complement of CBPs to surface electrochemistry is a net positive charge. At least one CBP, PspA, is known to have an overall positive charge in the animoterminal domain which is surface exposed (27). The net positive charge of CBPs may serve to stabilize the negatively charged polysaccharide polymers. Alternatively, the positive charges may promote the surface exposure of CBPs by reducing electrostatic repulsion which would otherwise keep func- Downloaded from http://iai.asm.org/ on February 27, 2014 by PENN STATE UNIV Geometric mean (FL1-H) D39 D39(A)1 U9372 FIG. 2. Adherence of pneumococcal strains to hexadecane. The percent adherence was determined as described in Materials and Methods. The diagonally striped bars are unadapted (CDM-C), and stippled bars represent adapted cultures (CDM-EA). Standard error bars are calculated from the means of at least three independent measurements in each group. Fluorescence intensity VOL. 70, 2002 We thank David Briles and Janet Yother for providing strains and Brenda Chapman for assistance with cell culture. We also appreciate many insightful discussions with Larry McDaniel. This work was supported by a grant from the Department of Veterans Affairs. REFERENCES 1. Ausubel, F., R. Brent, R. E. Kingston, et al (ed.). 1993. Current protocols in molecular biology. John Wiley & Sons, Inc., New York, N.Y. 2. Avery, O. T., C. M. MacLeod, and M. McCarty. 1944. Studies on the chemical nature of the substance inducing transformation of pneumococcal types. Induction of transformation by a desoxyribonucleic acid fraction isolated from pneumococcus type III. J. Exp. Med. 79:137–158. 3. Beachey, E. H. (ed.). 1980. General concepts and priniciples of bacterial Editor: E. I. Tuomanen 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 415 adherence in animals and man, vol. 6. Chapman & Hall, London, United Kingdom. Briles, D. E., J. D. King, M. A. Gray, L. S. McDaniel, E. Swiatlo, and K. A. Benton. 1996. PspA, a protection-eliciting pneumococcal protein: immunogenicity of isolated native PspA in mice. Vaccine 14:858–867. Briles, D. E., M. Nahm, K. Schroer, J. Davie, P. Baker, J. Kearney, and R. Barletta. 1981. Antiphosphocholine antibodies found in normal mouse serum are protective against intravenous infection with type 3 Streptococcus pneumoniae. J. Exp. Med. 153:694–705. Cundell, D. R., N. P. Gerard, C. Gerard, I. Idanpaan-Helkklla, and E. I. Tuomanen. 1995. Streptococcus pneumoniae anchor to activated human cells by the receptor for platelet-activating factor. Nature 377:435–438. Dillard, J. P., and J. Yother. 1994. Genetic and molecular characterization of capsular polysaccharide biosynthesis in Streptococcus pneumoniae type 3. Mol. Microbiol. 12:959–972. Fletcher, J. N., J. R. Saunders, H. Embaye, R. M. Odedra, R. M. Batt, and C. A. Hart. 1997. Surface properties of diarrhoeagenic Escherichia coli isolates. J. Med. Microbiol. 46:67–74. Gosink, K. K., E. R. Mann, C. Guglielmo, E. I. Tuomanen, and H. R. Masure. 2000. Role of novel choline binding proteins in virulence of Streptococcus pneumoniae. Infect. Immun. 68:5690–5695. Hammerschmidt, S., S. R. Talay, P. Brandtzaeg, and G. S. Chhatwal. 1997. SpsA, a novel pneumococcal surface protein with specific binding to secretory immunoglobulin A and secretory component. Mol. Microbiol. 25:1113– 1124. Kamerling, J. P. 2000. Pneumococcal polysaccharides: a chemical view, p. 81–114. In A. Tomasz (ed.), Streptococcus pneumoniae: molecular biology & mechanisms of disease. Mary Ann Liebert, New York, N.Y. Kotiranta, A., M. Haapasalo, K. Kari, E. Keruso, I. Olsen, T. Sorsa, J. H. Meurman, and K. Lounatmaa. 1998. Surface structure, hydrophobicity, phagocytosis, and adherence to matrix proteins of Bacillus cereus cells with and without the crystalline surface protein layer. Infect. Immun. 66:4895–4902. Magnusson, K.-E. 1989. Physicochemical properties of bacterial surfaces. Biochem. Soc. Trans. 17:454–458. Muckerman, C. C., S. S. Springhorn, B. Greenberg, and S. A. Lacks. 1982. Transformation of restriction endonuclease phenotype in Streptococcus pneumoniae. J. Bacteriol. 152:183–190. Ofek, I., E. Whitnack, and E. H. Beachey. 1983. Hydrophobic interactions of group A streptococci with hexadecane droplets. J. Bacteriol. 154:139–145. Rosenberg, M., D. Gutnick, and E. Rosenberg. 1980. Adherence of bacteria to hydrocarbons: a simple method for measuring cell-surface hydrophobicity. FEMS Microbiol. Lett. 9:29–33. Rosenow, C., P. Ryan, J. N. Weiser, S. Johnson, P. Fontan, A. Ortqvist, and H. R. Masure. 1997. Contribution of novel choline-binding proteins to adherence, colonization and immunogenicity of Streptococcus pneumoniae. Mol. Microbiol. 25:819–829. Sahly, H., R. Podschun, T. A. Oelschlaeger, M. Griewe, H. Parolis, D. Hasty, J. Kekow, U. Ullmann, I. Ofek, and S. Sela. 2000. Capsule impedes adhesion to and invasion of epithelial cells by Klebsiella pneumoniae. Infect. Immun. 68:6744–6749. Shoemaker, N. B., and W. R. Guild. 1974. Destruction of low efficiency markers is a slow process occurring at a heteroduplex stage of transformation. Mol. Gen. Genet. 128:283–290. Smith, B. L., and M. K. Hostetter. 2000. C3 as a substrate for adhesion of Streptococcus pneumoniae. J. Infect. Dis 182:497–508. Sundstrom, C., and K. Nilsson. 1976. Establishment and characterization of a human histiocytic lymphoma cell line (U-937). Int. J. Cancer 17:565–577. Tu, A. H., R. L. Fulgham, M. A. McCrory, D. E. Briles, and A. J. Szalai. 1999. Pneumococcal surface protein A inhibits complement activation by Streptococcus pneumoniae. Infect. Immun. 67:4720–4724. Vacheethasanee, K., J. S. Temenoff, J. M. Higashi, A. Gary, J. M. Anderson, R. Bayston, and R. E. Marchant. 1998. Bacterial surface properties of clinically isolated Staphylococcus epidermidis strains determine adhesion on polyethylene. J. Biomed. Mater. Res. 42:425–432. van Oss, C. J. 1978. Phagocytosis as a surface phenomenon. Annu. Rev. Microbiol. 32:19–39. Whitnack, E., A. L. Bisno, and E. H. Beachey. 1981. Hyaluronate capsule prevents attachment of group A streptococci to mouse peritoneal macrophages. Infect. Immun. 31:985–991. Wilson, W. W., M. M. Wade, S. C. Holman, and F. R. Champlin. 2001. Status of methods for assessing bacterial cell surface charge properties based on zeta potential measurements. J. Microbiol. Methods 43:153–164. Yother, J., G. L. Handsome, and D. E. Briles. 1992. Truncated forms of PspA that are secreted from Streptococcus pneumoniae and their use in functional studies and cloning of the pspA gene. J. Bacteriol. 174:610–618. Yother, J., and J. M. White. 1994. Novel surface attachment mechanism of the Streptococcus pneumoniae protein PspA. J. Bacteriol. 176:2976–2985. Downloaded from http://iai.asm.org/ on February 27, 2014 by PENN STATE UNIV tional domains inaccessible below the capsular surface. Overall, capsule is the major determinant of pneumococcal surface chemistry and surface proteins appear to have minor effects in its presence. An exception is the type 3 strain WU2, in which CBPs have an effect on surface hydrophobicity and charge. The surface of the other type 3 strain tested, A66, was essentially unchanged when CBPs were removed. The CBPs have a particularly large effect on adherence of pneumococci to human monocytes. For capsule type 2 strain D39, the effect is only seen when capsule is removed. For WU2, the effect of CBPs on adherence is measurable both in the presence and absence of capsule. This result is in agreement with the studies of hydrophobicity and surface charge for WU2. It is possible that WU2 represents a unique phenotype for type 3 strains or that type 3 strains as a group are heterogeneous in the manner by which CBPs contribute to cell surface chemistry and adhesion. Certainly, some of the effect of CBPs on cell adhesion is related to the loss of specific adhesins from the pneumococcal cell. However, given the striking effect that CBPs have on the physical characteristics of pneumococcal cells, it is plausible that the full complement of CBPs may promote bacterium-host cell interaction by electrostatic and/or hydrophobic interactions as well. An alternative explanation for these results is that the presence of ethanolamine in teichoic acids may be responsible for the alterations in surface chemistry. Phosphorylethanolamine is incorporated into teichoic acids in the same location as phosphorylcholine via a phosphodiester linkage to N-acetyl-D-galactosamine. The result of this substitution would not be predicted to have any net effect on surface charge or hydrophobicity. The observations presented here suggest an additional function for the polysaccharide capsule of pneumococci. In addition to protection from host humoral immune components, the pneumococcal capsule may inhibit interactions of surface proteins with phagocytes during invasive disease. In the context of colonization, where inflammation and phagocytes are minimal at the mucosal surface, the CBPs may provide a favorable surface chemistry for adhesion in addition to receptor-ligand interactions. In this case pneumococci may down-regulate the quantity of capsular polysaccharide to potentiate adhesion. In some model systems it has been shown that bacterial adherence to cultured mammalian cells is impeded by capsule (6, 18). Further work on the regulation of pneumococcal capsule expression in different in vivo environments will be necessary to address this question. NOTES