* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Long-term analysis of left ventricular ejection fraction in patients with
Cardiac contractility modulation wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Cardiac surgery wikipedia , lookup
Jatene procedure wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Myocardial infarction wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
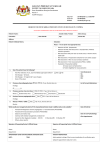
European Heart Journal (2013) 34, 3370–3377 doi:10.1093/eurheartj/eht201 CLINICAL RESEARCH Interventional cardiology Long-term analysis of left ventricular ejection fraction in patients with stable multivessel coronary disease undergoing medicine, angioplasty or surgery: 10-year follow-up of the MASS II trial Cibele Larrosa Garzillo 1, Whady Hueb 1*, Bernard J. Gersh 2, Eduardo Gomes Lima 1, Paulo Cury Rezende 1, Alexandre Ciappina Hueb 1, Ricardo D’Oliveira Vieira1, Desiderio Favarato 1, Alexandre Costa Pereira1, Paulo Rogério Soares1, Carlos Vicente Serrano Jr. 1, José Antônio Franchini Ramires1, and Roberto Kalil Filho 1 1 Department of Atherosclerosis, Heart Institute of the University of São Paulo, Av. Dr. Eneas de Carvalho Aguiar 44, AB, Sala 114, Cerqueira César, São Paulo/SP 05403-000, Brazil; and 2Mayo Clinic, Rochester, MI, USA Received 8 February 2013; revised 11 April 2013; accepted 22 May 2013; online publish-ahead-of-print 4 July 2013 See page 3339 for the editorial comment on this article (doi:10.1093/eurheartj/eht297) Background Assuming that coronary interventions, both coronary bypass surgery (CABG) and percutaneous coronary intervention (PCI), are directed to preserve left ventricular function, it is not known whether medical therapy alone (MT) can achieve this protection. Thus, we evaluated the evolution of LV ejection fraction (LVEF) in patients with stable coronary artery disease (CAD) treated by CABG, PCI, or MT as a post hoc analysis of a randomized controlled trial with a follow-up of 10 years. ..................................................................................................................................................................................... Methods Left ventricle ejection fraction was assessed with transthoracic echocardiography in patients with multivessel CAD, participants of the MASS II trial before randomization to CABG, PCI, or MT, and re-evaluated after 10 years of follow-up. ..................................................................................................................................................................................... Results Of the 611 patients, 422 were alive after 10.32 + 1.43 years. Three hundred and fifty had LVEF reassessed: 108 patients from MT, 111 from CABG, and 131 from PCI. There was no difference in LVEF at the beginning (0.61 + 0.07, 0.61 + 0.08, 0.61 + 0.09, respectively, for PCI, CABG, and MT, P ¼ 0.675) or at the end of follow-up (0.56 + 0.11, 0.55 + 0.11, 0.55 + 0.12, P ¼ 0.675), or in the decline of LVEF (reduction delta of 27.2 + 17.13, 29.08 + 18.77, and 27.54 + 22.74). Acute myocardial infarction (AMI) during the follow-up was associated with greater reduction in LVEF. The presence of previous AMI (OR: 2.50, 95% CI: 1.40– 4.45; P ¼ 0.0007) and during the follow-up (OR: 2.73, 95% CI: 1.25–5.92; P ¼ 0.005) was associated with development of LVEF ,45%. ..................................................................................................................................................................................... Conclusion Regardless of the therapeutic option applied, LVEF remains preserved in the absence of a major adverse cardiac event after 10 years of follow-up. ..................................................................................................................................................................................... Clinical Trial URL: http://www.controlled-trials.com. Registration number ISRCTN66068876. Registration ----------------------------------------------------------------------------------------------------------------------------------------------------------Keywords Left ventricular ejection fraction † Coronary artery disease † Coronary bypass surgery † Percutaneous coronary intervention † Medical therapy * Corresponding author. Tel: +55 1126615032, Fax: +55 1126615188, Email: [email protected] Published on behalf of the European Society of Cardiology. All rights reserved. & The Author 2013. For permissions please email: [email protected] 3371 Ventricular function in MASS II trial Introduction Studies of ageing of the cardiovascular system in healthy subjects, with focus on left ventricular ejection fraction (LVEF), are controversial. Some authors demonstrated that systolic function usually remains preserved, with worsening of diastolic function1 – 3 due mainly to adaptative mechanisms, such as myocyte hypertrophy and changes in diastolic dynamics. However, Cheng et al.,4 studying left ventricular function changes in patients without known cardiovascular disease, found a paradoxical increase in LVEF with ageing. Another study5 demonstrated a reduction in LVEF with ageing in patients with and without diabetes, after ruling out the presence of myocardial ischaemia. On the other hand, in the population with coronary artery disease (CAD), many of whom have associated comorbidities, the evolution of LVEF is unclear. It is assumed that ventricular function deterioration could occur, if associated with the presence of continued but unalleviated chronic myocardial ischaemia. Since ventricular function is the most important predictor of longterm survival in patients with CAD, regardless of the number of arteries affected or the degree of arterial stenosis,6 – 10 all therapeutic strategies that confer additional protection for the ischaemic myocardium are relevant in an attempt to improve long-term prognosis. In this setting, revascularization procedures, percutaneous coronary intervention (PCI) and coronary artery bypass graft (CABG), have the potential to contribute to the reduction of myocardial ischaemia and, in this way, possibly prevent progressive impairment of LVEF. A post hoc substudy from the (Optimal Medical Therapy With and Without Percutaneous Coronary Intervention) COURAGE trial11 compared the occurrence of the primary endpoint [death or acute myocardial infarction (AMI)] in patients with CAD randomized to optimal medical therapy (OMT) with or without PCI, according to the presence and extent of ischaemia at baseline. Surprisingly, regardless of the ischaemic extent, even in the subgroup of patients with moderate-to-severe ischaemia, the addition of PCI to OMT failed to demonstrate any additional benefit in long-term prognosis. Further study on the effectiveness of available treatments for CAD in patients with documented myocardium ischaemia of greater extension and severity, the ongoing ISCHEMIA trial,12 will compare the efficacy of different therapeutic strategies is patients with moderate-to-severe ischaemia. Additionally, the role of revascularization procedures in regard to their potential to protect the function of the ischaemic myocardium is not well established. In fact, there are very few studies that aimed to investigate, in depth, the role of such interventions on ventricular function during a long period of followup.13,14 Other trials comparing CABG and PCI strategies,15 – 17 or conservative vs. interventional therapies,18 – 21 focused on primary endpoints, such as mortality, occurrence of acute myocardial infarction, or the need of additional revascularization. The aim of this study was to evaluate the changes in LVEF, by sequential echocardiography, in patients with chronic multivessel coronary heart disease and initially preserved ventricular function, who underwent three therapeutic options (CABG, PCI, or MT alone) participants of the MASS II trial, during 10 years of follow-up. The second Medical, Angioplasty, or Surgery Study (MASS II) is a single-centre study designed to compare the long-term effects of MT, stent angioplasty, or surgical strategies among patients with multivessel CAD with stable angina and preserved ventricular function who are appropriate candidates for all three therapies.20,21 Methods MASS II patient selection Briefly, patients with angiographically documented proximal multivessel coronary stenosis of .70% by visual assessment and documented ischaemia were considered for inclusion. Patients were enrolled and randomized if the surgeons, attending physicians, and interventional cardiologists agreed that revascularization could be attained by either strategy.20,21 Patients gave written informed consent and were randomly assigned to a treatment group. The Ethics Committee of the Heart Institute (InCor) of the University of São Paulo Medical School in São Paulo, Brazil, approved the trial, and all the procedures were performed in accordance with the Helsinki Declaration. Clinical criteria for exclusion included mandatory revascularization, ventricular aneurysm that required surgical repair, LVEF ,40%, a history of PCI, CABG, congenital, or valvular heart disease; left main coronary artery stenosis of 50% or more, or another co-existing condition that was a contraindication to CABG or PCI. Treatment intervention In MASS II, all the patients were placed on an optimal medical regimen after randomization until the end of follow-up. Patients were randomized to continue with aggressive MT alone or to undergo PCI or CABG in addition to MT. Investigators were required to perform optimum coronary revascularization. For patients assigned to PCI, the procedure was available within 3 weeks after randomization and was performed according to a standard protocol.22 Devices used for catheter-based therapeutic strategies included stents, lasers, directional atherectomy, and balloon angioplasty. For patients assigned to CABG, the procedures were available within 12 weeks after randomization, and revascularization performed with standard surgical techniques,23 using saphenous vein grafts, internal mammary arteries, and other arterial conduits. No off-pump CABG was performed. Follow-up Adverse and other clinical events were tracked from randomization. Patients were evaluated and angina symptoms were graduated24 with follow-up visits every 6 months for at least 10 years at Heart Institute. Patients underwent the treadmill exercise test according to a modified Bruce protocol, electrocardiography and routine blood tests on regular basis. Myocardial infarction was defined as the presence of significant new Q waves in at least two ECG leads or symptoms compatible with MI associated with creatine kinase-MB fraction concentrations that were more than three times the upper limit of the reference range. The vital status of each patient was ascertained on 28 February 2011. The predefined primary endpoints were the incidence of total mortality, Q-wave MI, or refractory angina that required revascularization. Secondary endpoints included angina status, death due to a cardiac cause, and cerebrovascular accident. Left ventricular ejection fraction assessment Most participants of the MASS II trial underwent transtoracic echocardiography with colour Doppler before randomization. Of those, left ventricular function was evaluated at two different time periods: the first, at the beginning of the study, and the second, after 10 years of follow-up. 3372 C.L. Garzillo et al. Table 1 Baseline characteristics of the 350 patients with left ventricular ejection fraction reassessed according to treatment in MASS II PCI (n 5 131) CABG (n 5 111) MT (n 5 108) P-value ............................................................................................................................................................................... Demographic variables Age, years 58.42 + 9.04 58.10 + 7.68 57.87 + 8.76 0.886 Age ≥65 years (%) 30.53 22.52 25 0.346 Male (%) Current or past smoker (%) 63.36 37.61 68.47 35.45 70.37 32.82 0.485 0.738 History of MI (%) History of hypertension (%) 50.38 58.78 43.24 57.66 37.96 49.07 0.152 0.275 Treated diabetes mellitus (%) 24.43 36.04 34.26 0.106 History of angina (%) 92.37 89.19 80.56 0.018 ............................................................................................................................................................................... Clinical history and status ............................................................................................................................................................................... Laboratory values Total cholesterol (mmol/L) 5.92 + 1.27 5.58 + 1.14 5.74 + 1.06 0.485 LDL cholesterol (mmol/L) 3.95 + 1.14 3.77 + 1.06 3.80 + 0.88 0.521 HDL cholesterol (mmol/L) Triglycerides (mmol/L) 0.95 + 0.26 5.04 + 2.53 0.93 + 0.23 4.50 + 2.07 0.95 + 0.21 4.91 + 2.64 0.213 0.082 55.83 53.46 49.49 0.59 ............................................................................................................................................................................... Positive treadmill test (%) ............................................................................................................................................................................... Angiographic profile Double-vessel disease (%) 41.98 43.24 45.37 0.870 Triple-vessel disease (%) Double-vessel with proximal LAD disease (%) 58.02 78.18 56.76 77.08 54.63 85.71 0.870 0.579 Coronary collateral circulation (%) 38.58 42.57 43.30 0.736 LDL, low-density lipoprotein; HDL, high-density lipoprotein; LAD, left anterior descending coronary artery. Some patients had both angina and positive treadmill tests. Unless otherwise indicated, data are mean + SD. All echocardiographic parameters assessed were predefined and images were analysed in a core lab, by expert physicians. Left ventricular ejection fraction was measured by the biplane method (Simpson) when the endocardial border of the left ventricle was welldefined and whenever regional wall-motion abnormalities were present, or alternatively by the Teichholz method.25 Statistical analysis Baseline characteristics were summarized for all patients as percentages for categorical variables and as means with standard deviations for continuous variables. Comparisons between means of the groups used Student’s t test for parametric26 and the Mann– Whitney test for nonparametric variables. The means of three or more groups were compared by one-way ANOVA, followed by the Bonferroni multiple comparison test for parametric variables. For non-parametric variables, we used the Kruskal– Wallis test, followed by multiple comparisons based on Dunn’s test. Tests were two-sided. The evaluation of homogeneity between proportions was performed using the x2 or the Fisher exact test.26 To evaluate the behaviour of groups along the evaluations (initial and 10 years) analysis of variance with repeated measures was used.27 An additional analysis was performed using logistic regression to evaluate the association of several variables to determine LVEF dysfunction, defined as LVEF ≤45% in 10 year survivors. All data were analysed according to the intention-to-treat principle and values of P , 0.05 were considered statistically significant. Statistical analysis was performed with SPSS 15.0 for Windows. Results Patients characteristics Between May 1995 and May 2000, 611 eligible patients who met all entry criteria were randomly assigned to one of three therapeutic strategies: PCI, MT, or CABG. After a mean follow-up of 10.32 (+1.43) years, 422 patients were alive and 350 patients had their LVEF reassessed by echocardiography (108 patients from the MT group, 111 from CABG, and 131 from PCI). For several reasons, 72 patients could not have their LVEF reassessed, most commonly due to patient refusal, geographic inaccessibility and severe noncardiac illness. Randomization created balanced treatment groups with respect to important prognostic characteristics (Table 1), except for the angina status (less frequent in the MT group). Among patients eligible at 10.32 years to undergo LVEF evaluation, baseline characteristics of those who underwent LVEF assessment (n ¼ 350) were compared with those who did not (n ¼ 72). All variables analysed were similar in prevalence, except for diabetes, which 3373 Ventricular function in MASS II trial Table 2 Comparison of baseline characteristics and events between patients with and without left ventricular ejection fraction measurements Variable LVEF available (n 5 350) LVEF missing (n 5 72) P-value 67.4% 57.96 + 8.7 73.6% 60 + 9 0.374 0.073 History of 55.14% hypertension (%) 65.3% 0.146 Treated diabetes (%) 31.4% 47.2% 0.013 Previous AMI (%) 44.28 37.5 0.353 Current or past smoker (%) 35.14 31.9 0.701 Double-vessel disease (%) 42.85 47.2 Triple-vessel disease 57.14 52.8 Proximal LAD disease 90 86.1 0.445 Total cholesterol (mmol/L) 5.77 + 1.16 5.84 + 1.42 0.649 LDL cholesterol (mmol/L) 3.83 + 1.03 3.90 + 1.16 0.630 HDL cholesterol (mmol/L) 0.96 + 0.23 0.96 + 0.26 0.828 Triglycerides (mmol/L) PCI treatment (%) 4.86 + 2.56 5.09 + 3.36 0.554 37.42 29.2 0.278 CABG treatment (%) 31.42 40.3 MT treatment (%) 31.14 30.6 New AMI (%) Additional PCI (%) 12.28 15.71 6.94 8.33 0.193 0.104 Additional CABG (%) 13.71 8.33 0.213 ................................................................................ Male sex (%) Age (years) 0.532 Table 3 Major adverse cardiac events at 10 years PCI (n 5 131) (%) CABG (n 5 111) (%) MT (n 5 108) (%) P-value 13 (9.92) 36 (27.48) 9 (8.11) 10 (9.01) 16 (14.81) 15 (13.89) 0.255 ,0.001 15 (11.45) 4 (3.60) 31 (28.70) ,0.001 64 (48.45) 23 (20.72) 62 (57.41) ,0.001 3 (2.29) 7 (6.31) 6 (5.56) ................................................................................ AMI Additional PCI Additional CABG Combined events CVA 0.277 AMI, acute myocardial infarction; CVA, cerebrovascular accident; combined events are the sum of AMI, additional PCI or CABG. The overall major adverse cardiac and cerebrovascular events at 10-year follow-up of the patients who had their LVEF reassessed, according to one of three therapeutic strategies are shown in Table 3. The groups did not differ with respect to the occurrence of acute myocardial infarction. However, they differ regarding the need of additional revascularization (less frequent in the CABG group). follow-up (P ¼ 0.675, Table 4). Regardless of the treatment strategy, the three groups experienced the same pattern and magnitude of ventricular function variation (P ¼ 0.641), with a decline of LVEF (P , 0.001), represented by the reduction delta (27.2 + 17.13, 29.08 + 18.77, and 27,54 + 22.74 for PCI, CABG, and MT, respectively, Table 4 and Figure 1). Analysis of other variables identified a modest decline in LVEF overall and consistent across subgroups, except for AMI during the follow-up. Among those patients the extent of the reduction in LVEF was statistically significantly greater (Table 5). When those variables were correlated with the development of ventricular dysfunction, defined as LVEF ≤45%, the presence of previous AMI and AMI during the follow-up were associated with a greater chance of worsening of ventricular function (Figure 2). Other demographic and anatomic factors were not different between those with and without a decline in LVEF. Diastolic function was re-evaluated after 10 years of follow-up in 300 patients who had this measure obtained at baseline. One hundred and ten patients had diastolic dysfunction at baseline and 90% of those maintained this dysfunction at re-evaluation. On the other hand, 190 patients had normal diastolic function at baseline: in 34 patients (17.89%) this measure remained preserved, and 155 patients (82.11%) presented diastolic dysfunction in the end of the follow-up (47, 59, and 49 patients respectively, in the MT, PCI, and CABG group, with no difference in evolution according to treatment applied, P ¼ 0.331). Of the 350 patients with LVEF reassessed after 10 years of followup, 252 had ischaemia evaluated with the treadmill exercise test according to a modified Bruce protocol. There was no difference in the prevalence of positive tests, irrespective of treatment applied (Table 6). Besides, patients with ischaemia demonstrated by treadmill tests presented the same evolution of ventricular function, compared with the patients with no ischaemia at the end of the follow-up (Table 6). Left ventricular ejection fraction assessment Discussion The echocardiographic assessment identified similarity of LVEF in the three groups, both in the beginning and at the end of the 10-year This single institution study evaluated long-term evolution of left ventricular function, which was initially preserved, in patients with LDL, low-density lipoprotein; HDL, high-density lipoprotein; LAD, left anterior descending coronary artery; AMI, acute myocardial infarction. Unless otherwise indicated, data are mean + SD. was more frequent in patients without LVEF reassessment (Table 2). The need of additional revascularization and new AMI was similar between the groups. Treatment outcomes 3374 Table 4 C.L. Garzillo et al. Left ventricular ejection fraction evolution according the treatment assigned PCI CABG MT P-value ............................................................................................................................................................................... LVEF baseline LVEF 10 years Reduction delta (%) 0.61 + 0.07 0.61 + 0.08 0.61 + 0.09 0.675 0.56 + 0.11 27.2 + 17.13 0.55 + 0.11 29.08 + 18.77 0.55 + 0.12 27.54 + 22.74 0.675 0.631 Reduction delta ¼ 100 × (LVEF 10 year – LVEF baseline)/LVEF baseline. Table 5 Reduction of left ventricular ejection fraction according to the presence of several variables Variable (n) Reduction delta (%) P-value ................................................................................ Male (235) Female (115) Figure 1 Left ventricular ejection fraction at baseline and the 10th year, according to treatment assigned: P ¼ 0.675: mean left ventricular ejection fraction similar among groups in the beginning and end of the follow-up; P ¼ 0.641: similar evolution among the groups; P , 0.001: left ventricular ejection fraction decrease over time multivessel CAD who underwent one of three therapeutic strategies (PCI, CABG, or MT alone), participants of the MASS II randomized trial. Final results have shown that, regardless of the treatment option, LVEF remained preserved at the end of follow-up, albeit with an overall significant modest decline. This was observed irrespective of the coronary angiographic anatomy at the time of baseline and the need of additional revascularization. However, patients affected by AMI had a worse outcome, with a greater reduction of LVEF in comparison with all other subgroups. Moreover, patients with previous AMI or with AMI during the followup had a greater chance of developing ventricular dysfunction, characterized as LVEF ≤45%. Also, the need of CABG during the follow-up was marginally associated with the development of LVEF ≤45% in the multivariated model (P ¼ 0.05). Considering that our population is composed by patients with severe CAD and other comorbidities, and that abnormalities in endothelium-dependent vasodilation have been described in epicardial vessels and microcirculation in patients with known CAD, as well as in those with only risk factors for atherosclerosis,28 – 30 it can be inferred that both revascularization strategies (PCI and CABG) were of little relevance in the protection of the ischaemic myocardium, since ventricular function remained preserved in the absence of AMI. It is possible that the endothelial dysfunction provoked 28.71 + 20.00 26.23 + 18.36 0.278 ,65 years (258) 27.51 + 19.48 0.336 ≥65 years (92) Diabetes (109) 29.00 + 19.56 27.27 + 18.96 0.779 Non-diabetes (241) 28.18 + 19.75 Smoking Non-smoking 24.30 + 18.13 28.77 + 18.15 0.089 Previous AMI 29.25 + 14.52 0.248 No previous AMI Double-vessel without proximal LAD (30) Double vessel with proximal LAD disease (122) Triple-vessel disease (198) 26.82 + 16.13 29.29 + 17.63 0.727 26.78 + 20.05 28.37 + 19.46 Presence of coronary collateral circulation (144) 28.10 + 18.55 Absence of coronary collateral circulation (206) Additional PCI (61) 27.75 + 20.15 28.30 + 18.97 No Additional PCI (289) 27.81 + 19.62 0.825 0.884 Additional CABG (50) No additional CABG (300) 211.15 + 23.08 27.36 + 18.81 0.152 New AMI (38) 218.29 + 21.22 0.001 No AMI during follow-up (312) 26.63 + 18.91 Reduction delta ¼ 100 × (LVEF 10 year– LVEF baseline)/ LVEF baseline. by the epicardial vessel atherosclerosis in our patients could be responsible for the slight decrease in LVEF observed in all subgroups, irrespective of the treatment option and the presence of other risk profiles. In fact, the results shown by LVEF analysis demonstrate that, regardless of the therapeutic option, ventricular function was significantly impaired only when there was a history of AMI (prior to randomization or during the follow-up). One possible explanation for this result is that the subgroup with previous AMI included patients with LVEF slightly .45%, so that any decline in ventricular function, as a continuous variable, would led to LVEF value ,45%. 3375 Ventricular function in MASS II trial Figure 2 Association of several variables and development of left ventricular ejection fraction dysfunction (LVEF ≤45%). Double/triple indicates double vs. triple-vessel disease; Col. Circ., presence of coronary collateral circulation; MT/Revasc., medical treatment vs. revascularization (either PCI or CABG), according to treatment assigned from randomization; Add. PCI, additional PCI; Add CABG, additional CABG. Table 6 Ischaemia assessment with treadmill test after 10 years follow-up Ischaemic changes present Ischaemic changes absent P-value PCI (n) MT (n) 17 17 79 56 0.728 CABG (n) 16 67 Reduction delta 25.18 + 17.83 27.27 + 18.31 ................................................................................ 0.468 Reduction delta ¼ 100 × (LVEF 10 year– LVEF baseline)/ LVEF baseline. In this subgroup, as well as in all other patients in the MASS II trial, a slight decrease in LVEF was observed independently of the occurrence of AMI during the follow-up, but in the presence of this event the magnitude was greater. In this same way, investigators of the Bypass Angioplasty Revascularization Investigation (BARI) trial evaluated the LVEF (initially preserved) in 1220 subjects with multivessel coronary heart disease, 5 years after randomization for balloon PCI or CABG. They found a similarity in LVEF at that time period between the groups. However, attention was not drawn to the slight reduction in ventricular function observed in the comparison of baseline values of LVEF and the 5th year evaluation.13 Despite the similarity of those results with the present study, the BARI trial did not analyse a group with optimal medical treatment alone. In MASS II, LVEF of patients from the MT group demonstrated the same pattern of changes as those who underwent revascularization procedures. Another subset analysis of 100 of the 988 patients from the SoS trial (Stent or Surgery trial) evaluated the LVEF 30 days, 4 and 10 years after CABG or PCI with bare metal stents. They found an initial improvement in ventricular function after 30 days in both groups that was sustained at 4 and 10 year’s revaluation. It is important to note, however, that those results represent only one of the 53 sites of the trial and were confined to only 68 of the original 100 patients from that specific site.14 The COURAGE nuclear substudy31 also assessed ventricular function measurements at baseline and 6– 18 months after interventions. Results identified a similarity in rest and post-stress LVEF between patients in OMT, with or without PCI. Despite the short follow-up period, those results indicated that, similar to the findings of the present study, PCI did not confer any additional protection to the ventricular function. However, the nuclear substudy of COURAGE included only 314 of the 2287 participants of the original trial and additionally, measurements of ventricular function were missing in 141 patients at baseline and in 26 at follow-up. It is possible that the population selected for this substudy does not represent the entire population of the COURAGE trial. In the present study, of the 422 patients alive with a mean follow-up of 10 years and eligible for LVEF reassessment, echocardiography was not performed in 17% (72 patients). Although the prevalence of diabetes was greater in the group without revaluation of the ventricular function, this variable did not impact on poorer evolution of ventricular function in those with LVEF reassessed, and the variables responsible for worst outcome (AMI prior to randomization and during the 3376 follow-up) were similar between patients with and without LVEF revaluated. This would suggest that results presented here, i.e. the absence of a difference according to initial treatment assignment can probably be extrapolated to those patients who did not undergo LVEF reassessment. Noteworthy, this analysis of measurements performed at 10 years did not include any patient who died before that time. These results therefore apply only to patients alive at 10 years. It is possible that patients with lower LVEF died before our evaluation. Recent randomized clinical trials confirm equivalent long-term clinical outcomes for stable CAD patients treated with intensive medical management with or without coronary revascularization.18,19 In the MASS II trial, patients in CABG and PCI groups were under medication therapy as aggressive as patients of the MT group. The current findings indicate that an initial conservative strategy is effective for the prevention of MACE, as well as for the preservation of ventricular function in patients with stable CAD. Besides, it is possible that the intensive treatment for all other comorbidities could protect ventricular function of those patients. Additionally, the potential benefit of revascularization procedures over ventricular function could be lost after 10 years follow-up, considering graft patency and stent stenosis, as well as progression of atherosclerosis in native arteries. Clinical implications and conclusions Since LVEF is a major predictor of prognosis in patients with stable CAD, the impact of strategies on ventricular function is of interest and relevance.6,7,9 In this way, revascularization techniques were believed to be of greater importance. The MASS II trial has already shown similar survival of MT patients, when compared with PCI and CABG after a follow-up of 10 years.21 The current study demonstrated that initial medical treatment was equivalent to revascularization procedures in respect to long-term evolution of LVEF. Also, we have found that the occurrence of AMI was the only variable associated with deterioration of LVEF. Thus, aggressive MT and lifestyle prescriptions with comprehensive risk factor control are valuable and should not be underestimate in the treatment of patients with stable multivessel CAD. Acknowledgements Medical writing support was provided by Ann Conti Morcos of MorcosMedia during the preparation of this paper, supported by Zerbini Foundation. Funding This work was supported by a research grant from the Zerbini Foundation, São Paulo, Brazil. There is no relationship with industry. Funding was provided by the Zerbini Foundation. Conflict of interest: none declared. References 1. Lakatta EG, Levy D. Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part II: the aging heart in health: links to heart disease. Circulation 2003;107:346 –354. C.L. Garzillo et al. 2. Lakatta EG. Changes in cardiovascular function with aging. Eur Heart J 1990;11 (Suppl C): 22–29. 3. Pugh KG, Wei JY. Clinical implications of physiological changes in the aging heart. Drugs Aging 2001;18:263 – 276. 4. Cheng S, Fernandes VR, Bluemke DA, McClelland RL, Kronmal RA, Lima JA. Age-related left ventricular remodeling and associated risk for cardiovascular outcomes: the Multi-Ethnic Study of Atherosclerosis. Circ Cardiovasc Imaging 2009;2: 191 –198. 5. Stefanidis A, Bousboulas S, Kalafatis J, Baroutsi K, Margos P, Komninos K, Pappas S, Papasteriadis E. Left ventricular anatomical and functional changes with aging in type 2 diabetic adults. Eur J Echocardiogr 2009;10:647 –653. 6. Hammermeister KE, DeRouen TA, Dodge HE. Variables predictive of survival in patients with coronary artery disease: selection by univariate and multivariate analysis from the clinical, electrocardiographic exercise, arteriographic and quantitative angiographic evaluation. Circulation 1979;59:421 –430. 7. Weiner DA, Ryan T, McCabe CH, Chaitman BR, Sheffield LT, Ferguson JC, Fisher LD, Tristani F. Prognostic importance of clinical profile and exercise test in medically treated patients with coronary artery disease. J Am Coll Cardiol 1984;3:772 – 779. 8. Mock MB, Ringgvist I, Fisher LD, Davis KB, Chaitman BR, Kouchoukos NT, Kaiser GC, Alderman E, Ryan TJ, Russell RO, Mullin S, Fray D, Killip T 3rd. Survival of medically treated patients in the coronary artery surgery study (CASS) registry. Circulation 1982;66:562 –568. 9. Daly CA, De Stavola B, Sendon JL, Tavazzi L, Boersma E, Clemens F, Danchin N, Delahaye F, Gitt A, Julian D, Mulcahy D, Ruzyllo W, Thygesen K, Verheugt F, Fox KM; Euro Heart Survey Investigators. Predicting prognosis in stable angina— results from the Euro heart survey of stable angina: prospective observational study. BMJ 2006;332:262 –267. 10. Detre K, Peduzzi P, Murphy M, Hultgren H, Thomsen J, Oberman A, Takaro T. Effect of bypass surgery on survival in patients with low-and high risk subgroups delineated by use of simple clinical variables. Circulation 1981;63:1329 –1338. 11. Shaw LJ, Weintraub WS, Maron DJ, Hartigan PM, Hachamovitch R, Min JK, Dada M, Mancini GB, Hayes SW, O’Rourke RA, Spertus JA, Kostuk W, Gosselin G, Chaitman BR, Knudtson M, Friedman J, Slomka P, Germano G, Bates ER, Teo KK, Boden WE, Berman DS. Baseline stress myocardial perfusion imaging results and outcomes in patients with stable ischemic heart disease randomized to optimal medical therapy with or without percutaneous coronary intervention. Am Heart J 2012;164:243 –250. 12. Hochman J, Maron D for the ISCHEMIA trial Investigators. International study of comparative health effectiveness with medical and invasive approaches. Study in progress. http://www.ischemiatrial.org. 13. Gibbson RJ, Miller DD, Liu P, Guo P, Brooks MM, Schwaiger M. Similarity of ventricular function in patients alive 5 years after randomization to surgery or angioplasty in the BARI trial. Circulation 2001;103:1076 –1082. 14. Buszman P, Wiernek S, Szymanski R, Bialkowska B, Buszman P, Fil W, Stables R, Bochenek A, Martin J, Tendera M. Percutaneous versus surgical revascularization for multivessel coronary artery disease: a single center 10 year follow-up of SOS trial patients. Catheter Cardiovasc Interv 2009;74:420 – 426. 15. The Bypass Angioplasty Revascularization Investigation (BARI) Investigators. Comparison of coronary bypass surgery with angioplasty in patients with multivessel disease. N Engl J Med 1996;335:217 –225. 16. SoS Investigators. Coronary artery bypass surgery versus percutaneous coronary intervention with stent implantation in patients with multivessel coronary artery disease (the Stent or Surgery trial): a randomised controlled trial. Lancet 2002; 360:965 – 970. 17. Daemen J, Boersma E, Flather M, Booth J, Stables R, Rodriguez A, Rodriguez-Granillo G, Hueb WA, Lemos PA, Serruys PW. Long-term safety and efficacy of percutaneous coronary intervention with stenting and coronary artery bypass surgery for multivessel coronary artery disease: a meta-analysis with 5-year patient-level data from the ARTS, ERACI-II, MASS-II, and SoS trials. Circulation 2008;118:1146 –1154. 18. BARI 2D Study Group, Frye RL, August P, Brooks MM, Hardison RM, Kelsey SF, MacGregor JM, Orchard TJ, Chaitman BR, Genuth SM, Goldberg SH, Hlatky MA, Jones TL, Molitch ME, Nesto RW, Sako EY, Sobel BE. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med 2009;360:2503 – 2515. 19. Boden WE, O’Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, Knudtson M, Dada M, Casperson P, Harris CL, Chaitman BR, Shaw L, Gosselin G, Nawaz S, Title LM, Gau G, Blaustein AS, Booth DC, Bates ER, Spertus JA, Berman DS, Mancini GB, Weintraub WS; COURAGE Trial Research Group. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007;356: 1503 –1516. 20. Hueb W, Soares PR, Gersh BJ, Cesar LAM, Luz PL, Puig LB, Martinez EM, Oliveira SA, Ramires JAF. The Medicine, Angioplasty, or Surgery Study (MASS-II): a randomized, controlled clinical trial of three therapeutic strategies for multivessel coronary artery disease. J Am Coll Cardiol 2004;43:1743 –1751. 3377 Ventricular function in MASS II trial 21. Hueb W, Lopes N, Gersh BJ, Soares PR, Ribeiro EE, Pereira AC, Favarato D, Rocha AS, Hueb AC, Ramires JA. Ten-year follow-up survival of the Medicine, Angioplasty, or Surgery Study (MASS II): a randomized controlled clinical trial of 3 therapeutic strategies for multivessel coronary artery disease. Circulation 2010; 122:949 –957. 22. Douglas JR Jr, King SB III, Roubin GS. Technique of percutaneous transluminal angioplasty of coronary, renal, mesenteric, and peripheral arteries. In: Hurst JW, Schlant RC, Rackely CE, eds. The Heart. 7th ed. New York, NY: McGraw-Hill; 1990:2131 –2153. 23. Jones EL, Craver JM, King SB III, Douglas JS, Bradford JM, Brown CM, Bone DK, Hatcher CR Jr. Clinical, anatomic and functional descriptors influencing morbidity, survival and adequacy of revascularization following coronary bypass. Ann Surg 1980;192:390 –402. 24. Campeau L. Grading of angina pectoris. Circulation 1976;54:522 – 523. Letter. 25. Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, Gutgesell H, Reichek N, Sahn D, Schnittger I. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 1989;2:358 –367. 26. Rosner B. Fundamentals of Biostatistics. 2nd ed. Boston: PWS Publishers, 1986. 27. Timm NH. Multivariate Analysis with Applications in Educations and Psychology. Monterrey, CA: Brooks/Cole, 1975. 28. Panza JA. Coronary atherosclerosis: extending to the microcirculation? Eur Heart J 2010;31:905 –907. 29. Rubinshtein R, Yang EH, Rihal CS, Prasad A, Lennon RJ, Best PJ, Lerman LO, Lerman A. Coronary microcirculatory vasodilator function in relation to risk factors among patients without obstructive coronary disease and low to intermediate Framingham score. Eur Heart J 2010;31:936–942. 30. Camici PG, Crea F. Coronary microvascular dysfunction. N Engl J Med 2007;356: 830 –840. 31. Shaw LJ, Berman DS, Maron DJ, Mancini GB, Hayes SW, Hartigan PM, Weintraub WS, O’Rourke RA, Dada M, Spertus JA, Chaitman BR, Friedman J, Slomka P, Heller GV, Germano G, Gosselin G, Berger P, Kostuk WJ, Schwartz RG, Knudtson M, Veledar E, Bates ER, McCallister B, Teo KK, Boden WE; COURAGE Investigators. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation 2008;117:1283 –1291. CARDIOVASCULAR FLASHLIGHT doi:10.1093/eurheartj/eht229 Online publish-ahead-of-print 3 October 2013 ............................................................................................................................................................................. Unruptured sinus valsalva aneurysm in bicuspid aortic valve as an unusual cause of seasonal dyspnoea Kyung Hwa Kim*, Jong Bum Choi, and Jah Hong Kuh Department of Thoracic and Cardiovascular Surgery, Research Institute of Clinical Medicine, Chonbuk National University Medical School, 20 Geonji-Ro, Geumam-dong, Deokjin-gu, Jeonju 561-180, Republic of Korea * Corresponding author. Tel: +82 632502522, Fax: +82 632501480, Email: [email protected] A 44-year-old woman presented with an intracardiac cystic mass. She has been taking inhaled steroid during 2 years because of seasonal dyspnoea, with positive response to the methacholine bronchial provocation test. The chest X-ray showed no abnormal finding (Panel A). The echocardiogram showed a thin-walled saccular lesion in the right atrium and its’ cystic mass was extended from the ascending aorta and protruded into the right atrium (Panel B). A cardiac MRI revealed that the cystic mass was connected to the non-coronary sinus and was not located in the right atrium and confirmed the presence of an unruptured 30-mm diameter sinus valsalva aneurysm (SVA) (Panel C). We performed a bidirectional approach, in which both the aorta and the right atrium were opened and both the ends of the defect were separately repaired. The intra-operative exploration revealed a bicuspid aortic valve type 1, L/R with a thin-walled SVA (Panel D, left upper). First, following the excision of the aneurismal sac at its base in the low-pressure cardiac chamber (right atrium), the aortic end of the non-coronary sinus fistula was patched by means of a semi-circular-shaped prosthetic patch, tailored on a 21 aortic valve sizer, through aortotomy (Panel D, left lower). Then the resultant defect at its base in the right atrium was repaired by vascular patch (Panel D, right lower). She remains asymptomatic 2 years without any inhaled steroid after surgery. Also follow-up MRI demonstrate good geometric aortic sinus without aortic dilatation (Panel E). This case showed unruptured SVA association with the bicuspid aortic valve as an unusual cause of seasonal dyspnoea. Published on behalf of the European Society of Cardiology. All rights reserved. & The Author 2013. For permissions please email: [email protected]