* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
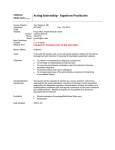
Download Psychiatric Appointment Form Powerpoint
David J. Impastato wikipedia , lookup
Psychological evaluation wikipedia , lookup
Dissociative identity disorder wikipedia , lookup
Factitious disorder imposed on another wikipedia , lookup
Conversion disorder wikipedia , lookup
History of psychiatry wikipedia , lookup
Moral treatment wikipedia , lookup
Developmental disability wikipedia , lookup
Classification of mental disorders wikipedia , lookup
Glossary of psychiatry wikipedia , lookup
Anti-psychiatry wikipedia , lookup
History of mental disorders wikipedia , lookup
Mental health professional wikipedia , lookup
Deinstitutionalisation wikipedia , lookup
Diagnostic and Statistical Manual of Mental Disorders wikipedia , lookup
Political abuse of psychiatry wikipedia , lookup
Mental status examination wikipedia , lookup
Psychiatric rehabilitation wikipedia , lookup
Psychiatric and mental health nursing wikipedia , lookup
Abnormal psychology wikipedia , lookup
Cases of political abuse of psychiatry in the Soviet Union wikipedia , lookup
History of psychiatric institutions wikipedia , lookup
Pyotr Gannushkin wikipedia , lookup
Political abuse of psychiatry in Russia wikipedia , lookup
Psychiatric survivors movement wikipedia , lookup
Psychiatric hospital wikipedia , lookup
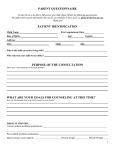
Providing Context at Psychiatric Appointments What Psychiatric Prescribers Need To Know When Assessing and Treating Individuals With Developmental Disabilities What Is In A Snapshot? Psychiatric appointments occur out of context. Psychiatric appointments are brief and in the moment. Sometimes people ‘aim to please’ when meeting with professionals. Without context, what is directly observed during a psychiatric appointment can be challenging to evaluate. Cognitive Delays & Provision of Verbal Context Abstractions such as time frames, reasons why, and relative seriousness of events might be distorted. Memory gaps and inability to fully describe a situation might impact what is shared. A patient might not understand questions in a diagnostic interview. Lack of trust with a clinician or saying “Yes” as a strategy to please might distort what is shared. Deep Listening Though psychiatric prescribers necessarily depend on others to provide context, it is important that patients with developmental disabilities are accorded respect and are the central treatment focus. Supports to Persons With Developmental Disabilities Family supports. Medicaid Personal Care and COPES supports. Adult Family Home supports. Group Homes and Boarding Home supports. Supported Living supports. Community Protection supports. Treatment Modalities Be sure that physical pain, neurological conditions, and other physiological issues are being treated. Ask if there is a Functional Assessment, Positive Behavior Support Plan, and a Cross-Systems Crisis Plan for patients with very challenging symptoms. Address the adequacy of residential, educational, and vocational supports. Is the patient using counseling therapies? Access Speech Therapy, OT and PT when helpful. Psychiatric treatment is not a stand alone solution. How Systems Skew Psychiatric Assessments and Treatments In frustration, support providers may over- state symptoms to effect a strong response. Unrealistic expectations are sometimes placed on psychiatric prescribers. There is a tendency to look for the most powerful pill. There is the idea that using medicine is the easiest (cheapest?) way to fix problems. Changes in Community Mental Health Services More money is being spent on pharmaceuticals and less money is being spent on mental health case management per client. Mental health caseloads have essentially doubled in Washington State in the past fifteen years. Collaboration and consultation between mental health case managers and prescribers for each client has substantially decreased. Requesting Contextual Information at Appointments Psychiatric prescribers depend on families and agency staff to provide supports to individuals with developmental disabilities at psychiatric appointments. Patients are better served if families and/or support providers understand psychiatric treatments. Good care requires good sharing of information – both ways. Psychiatric Appointment Information Sheet - GOALS Minimize unnecessary psychotropic medication use. Limit the number, dose and toxicity of necessary psychotropic medications as possible. Obtain as accurate and detailed information as possible to make medication decisions. Identify treatable psychiatric conditions. Identify environmental, social and medical causes of concerning behaviors. Determine efficacy of existing psychotropic therapy. Identify any side effects Demographic Information Patient Name Psychiatric Prescriber Appt. Date Person(s) Completing Form Relationship to Patient Who else provided input? Guardian (if any) Guardian phone # Date of last visit General Information Who is providing information? How well do they know the patient? Are there differing opinions or an agenda? What is the patient’s weight and why is it important? Basic Medical Information Recent Weight & Date when weighed Date of last Blood Draw Pharmacy Name and Phone Number Name(s) of other involved medical specialists (general practitioner, neurologist, gastroenterologist, dentist, etc.) Medications and Diagnosis List all current psychiatric meds, dosages, & times administered. List all current non-psychiatric meds, dosages, & times administered. Current DSM Diagnosis (if any): Axis I: Axis II: Axis III: Reasons For The Appointment Please address the following issue(s): Describe other efforts to address symptoms of concern: How is the client doing in general Great OK Doing Poorly Since the last appt. is the client doing: Better Same Worse Information From Patient’s Support System How is the patient doing now? Has anything changed since the last appointment? Stress Related To Life Events Loss of job Significant change in support staff Victim of crime or assault Change in family circumstance Increased stress at home Exposed/witness to violence Move to a new residence Law enforcement contact Death in family Medical tests/MD visits/ER visits Loss of preferred activity Death or loss of a friend Change in physical health Other - Physiological Symptoms Constipation Dizziness/fainting Nausea/Vomiting Slurred speech Diarrhea Rapid or slow pulse Rectal bleeding/discomfort Stumbling/unsteady gait Abdominal pain Weight gain/loss Urinary difficulties/excess Edema/swelling Chest pains Tingling/numbness Stiffness Tremor/shaking/ticks Seizures Fatigue Headache Physical weakness Injury requiring medical response Physiological Symptoms - II Unusual facial/ mouth/eye movement Unusual movements of extremities Drooling Dry mouth Increased thirst Unusual tastes/smells Appetite change Choking on food Dental pain Change in skin color Rash/Itching Breast discharge Sexual function difficulties Menstrual changes Excessive sleepiness Loud snoring Breathing abnormalities Wheezing or cough Sweating or chills Hearing/vision changes Hair loss/unusual growth Other - What Physiological Symptoms Can Tell Us Is the patient experiencing a medical condition as a potential cause of behavioral concerns? Is a psychotropic medication causing a physiological symptom? Is a psychotropic medication causing a medical condition? What physiological symptoms are associated most commonly with what psychotropic medications Behavioral Symptoms Assaultive Behavior Peculiar rituals Anger outburst(s) Listless, low energy Sleep/awake change Criminal activity SIB causing self-harm Has dangerous friends Poor attention to hygiene Increased irritability Restlessness or anxiety Pacing/repetitive Nightmares Obsessively organized Suicidal behavior Indiscriminate sexual activity Reported hallucinations Intrusive/pressured Elopement or Wandering Excessive neediness/dependent Crying/tearfulness Behavioral Symptoms II Substance Abuse Isolative, withdrawn Medication refusal(s) Low response, flat affect Changes in food/drink intake Repeated police/ER contacts ↓ interest in activities Making false accusations Property destruction Work/recreation activity refusals Talking about death/dying Hoarding/stealing/collecting Possible delusions/paranoia Labile, rapid change in mood Dramatic reduction in need for sleep Poor phone use (making 911 calls) Pressured/rapid speech Disorganized/tangential speech Stripping/exposing self in public Change in sexual activity Other - What Behavioral Symptoms Can Tell Us Behavioral symptoms as side effects of medication. Behavioral symptoms associated with various psychotropic medications. Behavioral symptoms associated with various psychiatric diagnoses. When is it appropriate to treat behavioral symptoms with psychotropic medication? Which behavioral symptoms are most likely to respond to psychotropic medication and which are not? Why are changes in circumstance important to consider in making decisions about psychotropic medications? Team Building Accurate psychiatric assessment and treatment of individuals with developmental disabilities is best done with a team approach. Detailed information sharing improves the quality of care. For a number of reasons there are powerful pressures on the mental health system to pursue efficiencies, decreasing time resources for adequate assessment and monitoring of psychiatric services. Formalizing ways to share information across systems may be a helpful structure for collaborations.