* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Coronary Circulation
Survey
Document related concepts
History of invasive and interventional cardiology wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Myocardial infarction wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Coronary artery disease wikipedia , lookup
Transcript
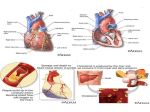
Coronary Blood Flow Models Dr. Jazmin Aguado-Sierra Brief History of Coronary Blood Flow Modelling • Scaramucci, J. (1695) was the earliest physiologist to postulate that during systole, the contracting myocardium inhibits its own blood flow. • Porter, WT. (1898) observed that time averaged flow increased with heart contraction and hence increased coronary flow. • Sabiston and Gregg (1957) concluded that contraction is an impeding factor to coronary blood flow. Coronary Systolic Flow Impediment (CSFI) Systolic flow is lower than diastolic flow. The inhibition of blood flow during systole, due to contraction, is the CSFI. Intramural blood volume varies throughout the cardiac cycle. In systole, blood volume is squeezed out of the intramyocardial vessels, but intramural blood volume is restored during diastole. The level of perfusion impediment depends on the balance between these two processes. At higher HR, there will be less net intramural vascular volume and thereby on average coronary resistance will be increased. Coronary Blood Flow Models • Systolic Extravascular Resistance (Gregg, 1957) • Vascular waterfall mechanism (Downey & Kirk, 1975) • Intramyocardial pump (Spaan, 1981) • Time-varying elastance (Suga, 1973; Krams, 1989) • Latest models Systolic Extravascular Resistance (Gregg, 1957) • It assumes that coronary resistance in systole is higher than in diastole due to extravascular compression, without specifying the mechanism. • It assumed the compression effect fades away quickly in diastole, so that at the end of diastole, the coronary resistance could be measured unrelated to the compression effect. Vascular Waterfall Mechanism (Downey & Kirk, 1975) • Intramyocardial pressure reduces coronary blood flow by creating vascular waterfalls; thus, the primary impediment to coronary blood flow is pressure in the ventricle. Flow is proportional to the difference between the perfusion pressure and the tissue pressure (waterfall pressure). • This model assumes that intramyocardial pressure (or tissue pressure) changes from zero at the epicardium, to peak at ventricular pressure at the endocardium. Westerhof N. et al, Physiol Rev 2006; 86:1263-1308. Vascular Waterfall Model • It assumes that radial stress in the ventricular wall generates a tissue pressure that is varying over the myocardial wall, from LV pressure at the endocardium, to thoracic pressure at the epicardium. It assumes that the tissue pressure acts on the outer surface of the intramural vessels as a fluid pressure. In case tissue pressure exceeds coronary arterial pressure, coronary flow would cease. • With a lower tissue pressure, only intramural veins are expected to locally collapse and at this collapse point, intramural pressure would be equal to tissue pressure. Downey & Kirk, Circ Res, 1975. Vascular Waterfall Mechanism • It explains the reduction of coronary flow due to increase in resistance, but it is unable to explain the arterial inflow and venous outflow. • It can’t account for retrograde systolic flow. • Ignores resistance variations during cardiac cycle Downey & Kirk, Circ Res, 1975. Intramyocardial Pump (Spaan, 1981) • This model ads the concept of compliance of the intramural vessels to the other models. • The intramural vascular compartment is represented by a lumped compliance. • The resistance of the intramural vessels is distributed into an inflow and an outflow resistance that roughly corresponds to the resistance of the arterioles and venules respectively. • Cardiac contraction squeezes blood volume out of the compliance, reducing arterial inflow and augmenting venous outflow. The elasticity of the intramural vessels would then form a restoration force for intramural volume, augmenting arterial inflow in the subsequent diastole and decreasing venous outflow. Intramyocardial Pump Model • This model assumes that intramyocardial pressure changes from zero at the epicardium, to peak at ventricular pressure at the endocardium. • It explains the arterio-venous lag by introducing the role of compliance. Compliant vessels are filled during diastole and discharged through the low-pressure venous direction in systole. • The capacitor in the electrical analog implies that during maintained contraction (heart arrested in systole) flow is not different from arrest in diastole. Westerhof N. et al, Physiol Rev 2006; 86:1263-1308. Elastance (Krams, 1989) • This model relies on the observation of similar flow impediment in “isovolumic” and “isobaric” states. Krams et al. Am J. Physiol. 1990; 258:H1889-98. Elastance (Krams, 1989) • Applied the concept of Elastance to the coronary artery flow. E • • • P V It emphasizes the effect of timevarying ventricular wall stiffness, which is assumed as independent of the ventricular pressure. The rate of change of vascular volume determines the sum of the decrease in arterial flow and increase of venous outflow. It fails to explain why the epicardial and endocardial flows are not impaired to the same degree. Westerhof N. et al, Physiol Rev 2006; 86:1263-1308. Contractility induced changes in CBF • CBF amplitude is strongly related to levels of contractility. Contractility has ~10 times stronger effect than PLV on amplitude of CBF. • It is the difference in stiffness of cardiac muscle in systole and diastole that determines CBF amplitude. Krams et al. Am J. Physiol. 1989; 258:H1936-1944. Recent Models (Kajiya, 2008) Lumped model of intramyocardial microcirculation. … during systole… White arrows indicate flow direction. Black arrows vessels indicate 10-20% change in diameter. Epicardial arteries and midmyocardial venules change little. My model: Time-Varying Effective Resistance using Wave Intensity Analysis (WIA) • It is derived from one-dimensional theory of flow in elastic tubes; solved using the method of characteristics; holding the advantage of timedomain analysis and retaining the non-linear treatment of flow in arteries. • It allows the analysis of non-periodic, transient flow. • It refers to the analysis of wave energy and wave propagation in the cardiovascular system. • Wave speed is required for separating the wave travel into their forward and backward directions. The Circulation is NOT in Steady State Oscillation Brief Introduction to WIA: Windkessel + Wave P in the ventriculo-arterial coupling • We model Pressure as: P Ao PW k Pex • Using conservation of mass and assuming the system is compliant • And the solution: Wang, J.J., et al. Am. J. Heart Circ. Physiol., 2003, 284, H1358--H1368. Reservoir-Wave separation in systemic arteries P( x, t ) P (t ) p ( x, t ) U ( x, t ) U (t ) u ( x, t ) Asc ao Ao arch Thor ao Page 18 © Imperial College London Abd ao Separation of reservoir and wave pressure along the aorta P (measured pressure) P (reservoir pressure) U (measured velocity) p (wave pressure) The exponential decay in diastole is very similar throughout the arterial system. The wave pressure is driving the inflow to the arterial system. Page 19 Aguado-Sierra J. JEM, 2007. Wave Separation before and after extraction of the Reservoir component Measured waveform Forward wave Reflected wave Reservoir component © Imperial College London Reservoir-Wave separation in the Coronary Arteries P waveforms are almost identical Page 21 Velocity measurements in the Coronary Arteries • Velocity waveforms are particularly determined by the systolic impediment due to myocardial contraction. • It cannot be assumed that the wave pressure (p) drives the blood flow into the coronaries © Imperial College London Page 22 Assumptions: • It is noticeable that velocity in diastole in the coronaries follows the diastolic decay of pressure. Westerhof N. et al, Physiol Rev 2006; 86:1263-1308. • Assuming that the reservoir component of Pressure drives the flow into the coronary arteries and that during diastole, the coronaries hold mostly a resistive behaviour to flow. Calculation of the reservoir-wave separation in the coronary arteries © Imperial College London Page 24 Time-varying Effective Resistance • We can then calculate an effective time-varying resistance imposed by the coronary microcirculation for each of the measurement locations, that can describe the blood flow impediment in the coronary arteries, mainly occurring during systole. P(t ) Pv R ( x, t ) U ( x, t ) Page 25 © Imperial College London Relation between effective resistance and ventricular pressure Effective resistance is different in each vessel and varies depending its spatial location and the region of the myocardium they perfuse. © Imperial College London Page 26 Wave speed calculation and wave separation • If we estimate the wave speed, we can separate the waves into their forward and backward components and we can further use WIA to better understand coronary haemodynamics and the cross talk with myocardial contraction. For example, in the LAD: Τ=1.02 s c∑²= 10.94 m/s a= 9.6 m/s Forward P wave dist Backward P wave Forward U wave prox Backward U wave dist prox Page 27 © Imperial College London Wave travel analysis provides evidence that perfusion into the myocardium is both due to the reservoir component and the active suction of the myocardium during its relaxation. 2 6 4 1 Wave Intensity Analysis in the Coronary Arteries 5 © Imperial College London Modified from Davies et al, Circulation 2006; 113:1768-1778. What models lack: • Effects on CBF of muscle shortening and thickening. • Vascular deformation with contraction, that involves changes of shape, vascular cross sections, branching angles, vessel tortuosity) • Subject specific parameterization. Computational Models (Smith NP, 2004) • Anatomically based, coupled to biomechanics. • Estimation of IMP from mechanical deformation. • Arterioles, capillaries and venules (≈vessels<100μm) are represented with a lumped parameter model (intramyocardial pump). • Solution of Navier-Stokes equations of flow reduced to a 1D case. Computational Models Extra Assignment Use the Intramyocardial Pump Model, and add a variation to it. Ideas can be found in: • Burattini et al. Ann Biomed Eng 13:385-404, 1985. • Bruinsma et al. Basic Res Cardiol 83:510-524,1988. • Chadwick et al. Am J Physiol Heart Circ Physiol 258:H1687-H1698, 1990. • Zinemanas et al. Ann Biomed Eng 22:638-652, 1994. • Zinemanas et al. Am J Physiol Heart Circ Physiol 268:H633-H645, 1995. • Hoffman and Spaan. Physiol Rev 70:331-390,1990. • Arts T and Reneman RS, Bibl Anat 103-107, 1977. • Arts T and Reneman RS, J Biomech Eng 107:50-56, 1985.