* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Non steroidal anti-inflammatory drugs
Pharmaceutical industry wikipedia , lookup
Pharmacognosy wikipedia , lookup
Neuropharmacology wikipedia , lookup
Prescription costs wikipedia , lookup
Drug interaction wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Psychopharmacology wikipedia , lookup
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
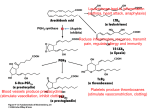
Non steroidal anti-inflammatory drugs Also called non steroidal anti-inflammatory agents/analgesics (NSAIDs) are a drug class that provide analgesic (pain-killing) and antipyretic (fever- reducing) effects, and, in higher doses, anti-inflammatory effects. Two main forms of cyclooxygenases (COX) Cyclooxygenase -1 (COX-1) produces prostaglandins that mediate hemeostatic function,and plays an important role in CI mucosa protection. Cyclooxygenase -2 (COX-2) produces prostaglandins that mediate inflammation, pain, and fever. Mechanism of action of NSAIDs: Most NSAIDs act as nonselective inhibitors of the enzyme cyclooxygenase (COX), inhibiting both the cyclooxygenase1 (COX-1) and cyclooxygenase-2 (COX-2) isoenzymes. This inhibition is competitively reversible , while the mechanism of aspirin is irreversible inhibition. When nonselective COX-1/COX-2 inhibitors (such as aspirin, ibuprofen, and naproxen) lower stomach prostaglandin levels, ulcers of the stomach or duodenum internal bleeding can result. The discovery of COX-2 led to research to development of selective COX-2 inhibiting drugs that do not cause gastric problems characteristic of older NSAIDs. Paracetamol (acetaminophen) is not considered an NSAID because it has little anti-inflammatory activity. It treats pain mainly by blocking COX-2 mostly in the central nervous system. NSAIDS have antipyretic activity and can be used to treat fever. Fever is caused by elevated levels of prostaglandin E2. Antipyretics work by inhibiting the enzyme COX, which causes the general inhibition of PGE2 within the hypothalamus. Ibuprofen has been shown more effective as an antipyretic than paracetamol (acetaminophen). Therapeutic uses 1. Inflammation NSAIDs are first- line drugs used to arrest inflammation and the accompanying pain of rheumatoid arthritis, osteoarthritis, ankylosing spondylitis, and dysmenorrhoea. Pain and inflammation of bursitis and tendonitis also respond to NSAIDs. Treatment of chronic inflammation requires use of these agents at doses above those used for analgesia and antipyresis (the incidence of adverse drug effect is increased). 2. Analgesia NSAIDs alleviate mild-to-moderate pain by decreasing PGE and PGF mediated increases pain receptor sensitivity. 3. Antipyresis NSAIDs reduce elevated body temperature with little effect on normal body temperature. Aspirin (acetylsalicylic acid) *Salicylates are weak acids. *These agents are rapidly absorbed from the intestine as well as from the stomach, where the low PH favors absorption. *Salicylates have a t1/2 of 3-6 h. after short term administration. *Long term administration of high doses or toxic overdose increases the t1/2 to 15-30 h. Uses: Rheumatoid arthritis, Juvenile arthritis. Osteoarthritis. Non acetylated salicylates (5-aminosalicylates) such as mesalamine, and sulfasalazine can be used to treat Crohn’s disease. Salicylic acid is used topically to treat planter wart, fungal infection and corns. Aspirin has significantly greater antithrombotic activity than other NSAIDs. Adverse effects: a. Gastrointestinal effects: most common adverse effects of high dose aspirin use(70% of patients) Nausea, vomiting, diarrhea or constipation, dyspepsia, epigastric pain, bleeding and ulceration. These GI effects are due to a decrease in the production and cytoprotective activity of PG which leads to gastric tissue susceptibility to damage by HCL. The GI effects may contraindicate aspirin use in patients with an active ulcer. Aspirin may be taken with PG to reduce gastric damage. b. Hypersensitivity(intolerance): It is relatively uncommon with the use of aspirin (o.3% of patients) hypersensitivity results in rash, bronchospasm, rhinitis, or an anaphylactic reaction with shock which may be life threatening. The incidence of intolerance is highest in patients with asthma, nasal polyp, or urticaria. ( aspirin should be avoided in such patients) Hypersensitivity is not associated with sodium or magnesium salicylates (non-acetylated salicylates). The use of aspirin to control fever during viral infection in children or adolescent is associated with an increased incidence of Raye’s syndrome, an illness characterized by vomiting, hepatic disturbance, and encephalopathy. Acetaminophen is recommended as a substance for children with fever of unknown etiology. c. Miscellaneous adverse effects and contraindication May decrease the glomerular filtration rate particularly in patients with renal insufficiency. Occasionally produce mild hepatitis. Prolong bleeding time. Salicylates use contraindicated in patients with bleeding disorders.(suppressing platelet adhesion and aggregation) Aspirin is contraindicated in patients with gout. (decreased urate excreation). Drug- drug interaction with salicylates leading to altered effects of (phenytoin, valporic acid, heparin) by increasing plasma conc., leading to prolonged t1/2, therapeutic effects, and toxicity. Other non steroidal anti-inflammatory drugs: Propionic acid derivatives: Ibuprofen, fenoprofen, ketoprofen, naproxen There is no reported interaction of ibuprofen or ketoprofen with anticoagulants. Fenoprofen has been reported to induce nephrotoxic syndrome. Long term use of ibuprofen is associated with an increased incidence of hypertension in women. Sulindac,tolmetin,ketorolac: Sulindac is a prodrug that is oxidized to a sulfone and then to the active sulfide. Has a relatively long t1/2 (16 h.) Tolmetin has minimal effect on platelet aggregation. It is associated with a higher incidence of anaphylaxis than other NSAIDs. Tolmetin has a relatively short t1/2 (1 h.) Ketorolac is a potent analgesic with moderate anti-inflammatory activity. Ketorolac can be administered IV. or topically in an ophthalmic solution. Indomethacin: Use as anti-inflammatory *treatment of ankylosing spondylitis, reiter syndrome, and acute gouty arthritis. *to speed the closure of patent ductus arteriosus.(it inhibits the production of PG that prevent closure of the ductus). Indomethacin is not recommended as a simple analgesic or antipyretic because of the potential for sever adverse effects. Adverse effects: bleeding, ulceration, and headache, occasional adverse effects include tinnitus, dizziness, or confusion. Piroxicam: Piroxicam is an oxicam derivative of enolic acid. Has t1/2 of 45 h. Like aspirin and indomethacin, bleeding and ulceration are more likely with piroxicam than with other NSAIDs. Mefenamic acid: T1/2 of 2 h. A relatively high incidence of GI disturbances is associated with these agents. Nabumetone: Compared with NSAIDs, nabumetone is associated with reduced : ** Inhibition of platelet function ** Incidence of GI bleeding Nabumetone inhibits COX-2 more than COX-1 COX-2 selective agents: Celecoxib, rofecoxib, and valdecoxib. Inhibit COX-2 more than COX-1. The rational behind development of these drugs was that : *Inhibition of COX-2 would reduce the inflammatory response and pain. * Not inhibit the cytoprotective action of PG in the stomach, which is largely mediated by COX-1 Rofecoxib and valdecoxib have been removed from the market due to a doubling in the incidence of heart attack and stroke. Celecoxib remains on the market and is approved for: * Osteoarthritis and rheumatoid arthritis. * Pain including bone pain, dental pain, and headache * Ankylosing spondylitis. Other anti-inflammatory drugs are used in the more advanced stages of some rheumatoid diseases. Gold compounds: (Aurothioglucose, Gold sodium thiomalate, Auranofin) May retard the destruction of bone and joints by unknown mechanism. Aurothioglucose and gold sodium thiomalate are administered IM. Auranofin is administered orally. Side effects: Serious effects (GI disturbances, dermatitis, and mucous membrane lesions), less common effects (aplastic anemia, proteinuria), occasional side effects ( nephrotic syndrome). Penicillamine: Penicillamine is a metabolite of penicillin. Has immunosuppressant activity, but it’s mechanism of action is unknown. The incidence of sever adverse effects is high, these effects are similar to those of the gold compounds. Methotrexate: Is an antineoplastic drug used for rheumatoid arthritis that does not respond well to NSAIDs or glucocorticoids. Methotrexate commonly produces hepatotoxicity. Chloroquine and hydrochloroquine: Are antimalarial drugs Have immunosuppressant activity, but their mechanism of action is unknown. Used to treat joint pain associated with lupus and arthritis. Non opioid analgesics and antipyretics: Acetaminophen (paracetamol): Acetaminophen has no significant anti-inflammatory activity. It causes minimal gastric irritation. Has little effect on platelet adhesion and aggregation. Acetaminophen is administered orally and is rapidly absorbed. Overdose with acetaminophen:accumulation of a minor metabolite,Nacetyl-P-benzoquinone which responsible for hepatotoxicity. Acetaminophen is a substitute for aspirin to treat mild –to –moderate pain for selected patients who are: 1. Intolerant to aspirin. 2. Have a history of peptic ulcer. 3. Are using anticoagulants or uricosuric drug to manage gout. 4. Are at risk for Reye’s syndrome. Disease-modifying antiarthritis drugs (DMAARDs) Tumor Necrosis Factor (TNF-α) is responsible for inducing IL-1 and IL-6 and other cytokines that further the disease. 1. Anti- TNF-α drugs ( infliximab, adalimumab, etanercept) Infliximab: Specifically binds TNF-α thereby blocking it’s action. Infliximab approved for use for rheumatoid arthritis, Crohn’s disease, psoriasis, ather autoimmune diseases. Infliximab administered by IV.infusion at 2week interval initially and repeated at 6-8 weeks. 2. Anti-IL1 drugs (anakinra) Is a competitive antagonist of the IL-1 receptor. It is approved for use for the treatment of rheumatoid arthritis. It has a relatively short t1/2 and administered S/C daily. Drugs used for gout: Gout: is a familial disease characterized by recurrent hyperuricemia, arthritis, and sever pain. It is caused by deposits of uric acid in joints, cartilage, and the kidney. Acute gout is treated with nonsalicylate NSAIDs, particularly indomethacin and colchicine. Chronic gout is treated with *Uricosuric agents: They increase the elimination of uric acid (probenecid , sulfinpyrazone) *Inhibits uric acid production (allopurinol) The adverse effects: 1. After oral administration include: nausea, vomiting, abdominal pain, and particularly diarrhea. 2. IV administration reduces the risk of GI disturbances, but increases the risk of sloughing and S/C tissue. 3. Higher doses may (rarely) result in liver damage and blood dyscrasias. Probenecid and sulfinpyrazone: Reduce urate levels by acting at the anionic transport site in the renal tubule to prevent reabsorption of uric acid. These agents are used for chronic gout, often in combination with colchicine. Drug interaction: these agents inhibit the excretion of other drug that are actively secreted by renal tubules, including penicillin, NSAIDs, cephalosporins, and methotrexate. Allopurinol: Mechanism of action: Allopurinol inhibits the synthesis of uric acid by inhibiting xanthine oxidase, an enzyme that converts hypoxanthine to xanthine and xanthine to uric acid. Allopurinol should be used with caution in patients with liver disease or bone marrow depression.