* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download J Glob Infect Dis
Survey
Document related concepts
Transcript
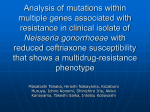
Antibiotics Resistance The appeal of the WHO: The Guardian: Antibiotic Resistance: Bacteria are winning the war http://www.guardian.co.uk/science/2011/apr/07/antibiotic-resistance-bacteria WHO Fact Sheet: Antimicrobial Resistance http://www.who.int/mediacentre/factsheets/fs194/en/ Albion Monitor http://www.albionmonitor.com/5-27-96/antibioticsfail.html Washington Post WHO Urges End fo Use of Antibiotics for Animal Growth http://www.mindfully.org/Farm/2003/WHO-Animal-Antibiotic13aug03.htm J Antimicrob Chemother. 2007 Sep;60(3):582-6. Epub 2007 Jun 29. Changing trends of antimicrobial susceptibility patterns of Neisseria gonorrhoeae in India and the emergence of ceftriaxone less susceptible N. gonorrhoeae strains. Bala M, Ray K, Gupta SM, Muralidhar S, Jain RK. Source Regional STD Teaching Training and Research Centre, Vardhman Mahavir Medical College and Safdarjang Hospital, New Delhi, India. [email protected] Abstract OBJECTIVES: To monitor the trend of antimicrobial susceptibility of Neisseria gonorrhoeae isolates from 2002 to 2006 in New Delhi, India under the Gonococcal Antimicrobial Susceptibility Programme and to document the emergence of any new antimicrobial resistance. METHODS: Antimicrobial susceptibility of 382 N. gonorrhoeae isolates from clinical cases in males and females to penicillin, tetracycline, ciprofloxacin, spectinomycin and ceftriaxone was determined by disc diffusion technique, using WHO reference strains as controls and WHO interpretative criteria. MICs were determined using Etests. RESULTS: A significant increasing trend of penicillin and ciprofloxacin resistance up to 2003 and 2004, respectively, and subsequent decrease in resistant strains with a concomitant increase in less susceptible strains, was observed. Tetracycline-resistant N. gonorrhoeae increased significantly from 6.7% in 2002 to 22.9% in 2005. Only one isolate was resistant to spectinomycin and nine isolates were less susceptible to ceftriaxone, during this 5 year period. A substantial proportion (23.3%) of strains were multiresistant. CONCLUSIONS: Emergence of ceftriaxone less susceptible N. gonorrhoeae isolates is a cause for concern, although treatment failure was not observed. An active, continuous and comprehensive programme for monitoring and surveillance of antimicrobial resistance needs to be established in many laboratories, and a search for new effective agents needs to be initiated to respond to the emergence of resistant isolates. Supplemental Content J Glob Infect Dis. 2010 Sep;2(3):284-90. Cephalosporin Resistance in Neisseria gonorrhoeae. Bala M, Sood S. Source Regional STD Teaching Training and Research Centre, Vardhman Mahavir Medical College and Safdarjang Hospital, New Delhi, India. Abstract Gonorrhea, a disease of public health importance, not only leads to high incidence of acute infections and complications but also plays a major role in facilitating human immunodeficiency virus (HIV) acquisition and transmission. One of the major public health needs for gonorrhea control is appropriate, effective treatment. However, treatment options for gonorrhea are diminishing as Neisseria gonorrhoeae have developed resistance to several antimicrobial drugs such as sulfonamides, penicillin, tetracyclines and quinolones. Antimicrobial resistance (AMR) surveillance of N. gonorrhoeae helps establish and maintain the efficacy of standard treatment regimens. AMR surveillance should be continuous to reveal the emergence of new resistant strains, monitor the changing patterns of resistance, and be able to update treatment recommendations so as to assist in disease control. Current treatment guidelines recommend the use of single dose injectable or oral cephalosporins. The emergence and spread of cephalosporin resistant and multi drug resistant N. gonorrhoeae strains, represents a worrying trend that requires monitoring and investigation. Routine clinical laboratories need to be vigilant for the detection of such strains such that strategies for control and prevention could be reviewed and revised from time to time. It will be important to elucidate the genetic mechanisms responsible for decreased susceptibility and future resistance. There is also an urgent need for research of safe, alternative anti-gonococcal compounds that can be administered orally and have effective potency, allowing high therapeutic efficacy (greater than 95.0% cure rate). Supplemental Content J Clin Microbiol. 2010 Jun;48(6):2016-21. Epub 2010 Mar 29. High prevalence of dihydropteroate synthase mutations in Pneumocystis jirovecii isolated from patients with Pneumocystis pneumonia in South Africa. Dini L, du Plessis M, Frean J, Fernandez V. Source Department of Parasitology, Mycology, and Environmental Microbiology, Swedish Institute for Infectious Disease Control, Solna, Sweden. [email protected] Abstract Pneumocystis jirovecii pneumonia (PCP) is an important cause of morbidity and mortality in immunocompromised patients. Sulfa-containing drugs are used for the treatment and prophylaxis of PCP. Mutations in the P. jirovecii fas gene, which encodes dihydropteroate synthase (DHPS), are associated with prior exposure to sulfa drugs, and their appearance suggests the emergence of variants with reduced sulfa susceptibility. The present study examined the prevalence of DHPS mutations in P. jirovecii strains isolated from South African patients with PCP. P. jirovecii infection was investigated by immunofluorescence microscopy and quantitative real-time PCR with respiratory specimens from 712 patients (93% of whom were >15 years of age) with suspected PCP consecutively received for the detection of P. jirovecii over 1 year. PCR amplification and sequencing of the DHPS fas gene was attempted with DNA from the P. jirovecii-positive samples. P. jirovecii infection was confirmed by immunofluorescence microscopy in 168/712 (24%) of the patients. Carriage of the fungus was revealed by real-time PCR in 17% of the patients with negative microscopy results. The P. jirovecii fas gene was successfully amplified from specimens from 151 patients and sequenced. Mutations resulting in the Thr55Ala and/or Pro57Ser amino acid substitution were detected in P. jirovecii strains from 85/151 (56%) patients. The high frequency of PCP episodes with P. jirovecii harboring DHPS mutations in South Africa indicates that populations of this fungus are evolving under the considerable selective pressure exerted by sulfa-containing antibiotics. These results, similar to previous observations of sulfa drug resistance in bacterial populations, underscore the importance of the rational use of sulfa medications either prophylactically against PCP or for the treatment of other infections. Supplemental Content Acta Derm Venereol. 2009;89(5):484-7. Neisseria gonorrhoeae antibiotic resistance in Paris, 2005 to 2007: implications for treatment guidelines. Farhi D, Hotz C, Poupet H, Gerhardt P, Morand P, Poyart C, Sednaoui P, Avril MF, Dupin N. Source Department of Dermatology, UPRES1833 Centre National de Référence de la Syphilis, Paris, France. [email protected] Abstract Quinolone-resistant Neisseria gonorrhoeae rates have increased worldwide since 1994. The objective of this study was to appraise: (i) the antimicrobial susceptibility of Neisseria gonorrhoeae in a venereology clinic in Paris, between 2005 and 2007; and (ii) the factors associated with quinolone-resistant N. gonorrhoeae. A prospective study of consecutive cases was performed for the period 2005 to 2007. Susceptibility of N. gonorrhoeae to five antibiotics (ciprofloxacin, ceftriaxone, spectinomycin, penicillin G and tetracycline) was tested systematically. Clinical and epidemiological data were collected using a standardized form. Male-to-female sex ratio was 22.0. Median age was 30.0 years. Of 115 cases, 84 occurred in men having sex with men (72.6%) and 22 involved the anorectal area (19.1%). The rate of quinolone-resistant N. gonorrhoeae was 37.4% (43/115), without significant association with gender, age, sexual behaviour, past history of sexually transmitted diseases and susceptibility to other antibiotics. All N. gonorrhoeae were susceptible to ceftriaxone and spectinomycin. The rate of quinolone-resistant N. gonorrhoeae in Paris has been increasing since 2004. Ceftriaxone remains the gold standard treatment. Supplemental Content Clin Infect Dis. 2009 Aug 15;49(4):515-21. Macrolide resistance and molecular types of Treponema pallidum causing primary syphilis in Shanghai, China. Martin IE, Gu W, Yang Y, Tsang RS. Source Division of Pathogenic Neisseria, Syphilis Diagnostics, Vaccine Preventable Bacterial Diseases, National Microbiology Laboratory, Public Health Agency of Canada, Winnipeg, Manitoba, Canada. Abstract BACKGROUND: The resurgence of syphilis in China requires laboratories to update their methods for molecular epidemiology investigation and surveillance. This study focuses on implementing polymerase chain reaction (PCR) diagnostic tests for syphilis and for detection of molecular subtypes and macrolide resistance among strains causing primary syphilis in the city of Shanghai, China. METHODS: Swabs were obtained from the genital lesions of 39 patients who presented with symptoms compatible with primary syphilis. Eight of the patients also provided whole blood samples. Swabs were also obtained from 10 patients without syphilis who presented with genital ulcers. PCR tests to amplify 3 common but unlinked treponemal genes were performed on DNA samples extracted from these specimens. Molecular subtyping was based on genetic characterization of 2 treponemal repeat genes, arp and tpr. Detection of macrolide resistance was accomplished by identification of the 23S ribosomal RNA gene mutation associated with the resistance pattern. RESULTS: Thirty-eight patients with primary syphilis were found to have Treponema pallidum DNA in their genital lesions by PCR assays using primers that target the bmp, tpp-47, and polA genes. None of the patients without syphilis had positive PCR results. Five molecular subtypes were identified, with 1 type (14f) causing 79% of the cases. All 38 patients were found to be infected with macrolide-resistant strains. CONCLUSIONS: Three common treponemal gene targets (bmp, tpp-47, and polA) were detectable by PCR in patients with primary syphilis. A single clone characterized as 14f and showing macrolide resistance appeared to have caused most of the primary syphilis cases in this study. Supplemental Content Clin Infect Dis. 2006 Feb 1;42(3):337-45. Epub 2005 Dec 28. Azithromycin-resistant syphilis infection: San Francisco, California, 2000-2004. Mitchell SJ, Engelman J, Kent CK, Lukehart SA, Godornes C, Klausner JD. Source STD Prevention and Control Services, San Francisco Department of Public Health, San Francisco, CA 94103, USA. Abstract BACKGROUND: The incidence of syphilis has been increasing in the United States since reaching a nadir in 2000. Several clinical trials have demonstrated that treatment with oral azithromycin may be useful for syphilis control. After reports of azithromycin treatment failures in San Francisco, we investigated the clinical and epidemiologic characteristics of patients with syphilis due to azithromycin-resistant Treponema pallidum infection. METHODS: We reviewed city-wide case reports and conducted molecular screening for patients seen at the San Francisco metropolitan STD clinic (San Francisco City Clinic) to identify patients who did not respond to azithromycin treatment for syphilis or who were infected with azithromycin-resistant T. pallidum. We conducted an epidemiologic investigation and retrospective case-control study to identify risk factors for acquiring syphilis due to azithromycin-resistant T. pallidum. RESULTS: From January 2000 through December 2004, molecular screening of 124 samples identified 46 azithromycin-resistant T. pallidum isolates and 72 wild-type T. pallidum isolates. Six instances of treatment failure were identified through record review. In total, we identified 52 case patients (one of whom had 2 episodes) and 72 control patients. All case patients were male and either gay or bisexual, and 31% (16 of 52) were infected with human immunodeficiency virus. Investigation of patient-partner links and a retrospective casecontrol study did not reveal a sexual network or demographic differences between cases and controls. However, 7 case patients had recently used azithromycin, compared with 1 control patient. Surveillance data demonstrated that azithromycin-resistant T. pallidum prevalence increased from 0% in 2000 to 56% in 2004 among syphilis cases observed at the San Francisco City Clinic. CONCLUSIONS: Azithromycin-resistant T. pallidum is widespread in San Francisco. We recommend against using azithromycin for the management of syphilis in communities where macrolide-resistant T. pallidum is present and recommend active surveillance for resistance in sites where azithromycin is used. Supplemental Content Indian J Med Microbiol. 2008 Jan-Mar;26(1):62-4. Antimicrobial susceptibility profile of Neisseria gonorrhoeae at STI clinic. Shilpee C, Ramachandran VG, Das S, Bhattacharya SN. Source Department of Microbiology, University College of Medical Sciences and Guru Teg Bahadur Hospital, Dilshad Garden, New Delhi - 110 095, India. [email protected] Abstract A total of 100 consecutive patients who attended a sexually transmitted infections clinic were studied. Thirteen had gonococcal urethritis, of which 10 showed growth of Neisseria gonorrhoeae on culture. All the isolates were tested for antimicrobial susceptibility by Australian Gonococcal Surveillance Programme (AGSP) method and beta lactamase production by chromogenic cephalosporin test. Four patients were co-infected with each of the following: HIV, HBV and Chlamydia trachomatis . Gonococcal urethritis (13%) was found more in male patients. Ten percent gonococcal isolates were penicillinase-producing N. gonorrhoeae , and another 10% were tetracycline-resistant N. gonorrhoeae . Supplemental Content Rev Esp Quimioter. 2011 Sep;24(3):136-42. [Which is the best empirical treatment in patients with urethritis?]. [Article in Spanish] Orellana MA, Gómez-Lus ML. Source Laboratorio Centro de Especialidades Periféricas, Madrid, Spain. [email protected] Abstract OBJECTIVE: To know the best empirical treatment of urethritis in patients at the City Center of Madrid. METHODS: 2.021 urethral exudates were analyzed in men between January 2003-December 2007. In addition to the traditional cultures, it was determined the presence of Chlamydia trachomatis, Ureaplasma urealyticum, Mycoplasma hominis, Trichomonas vaginalis and Herpes simplex. The susceptibility of N.gonorrhoeae and Haemophilus spp was performed by disk diffusion method and U. urealyticum by Mycoplasma IST. RESULTS: The percentage of positive samples was: 30.6%. The most frequently isolated microorganisms were: U. urealyticum 9.9%, N. gonorrhoeae 7.4%, C. trachomatis 5.1% and Haemophilus spp 3.8%. The resistance of N. gonorrhoeae in the first period was: penicillin 11.8%, tetracycline 5.9%, ciprofloxacin 8.8% and presence of betalactamase 11.8%. In the second period: penicillin 9.7%, amoxicillin/clavulanic acid 1.4%, tetracycline 8.3%, ciprofloxacin 23.6% and presence of betalactamase 10.5%. Resistance to ciprofloxacin in non-MSM (men having sex with men) was 20% and in MSM 56.2%. Resistance of Haemophilus spp in the first period was: 38.2% ampicillin, amoxicillin/clavulanic acid 8.8%, clarithromycin 35.3%, cotrimoxazole 64.7%, cefuroxime 5.9%, ciprofloxacin 8.8%, tetracycline 12.1% and presence of betalactamase 26.5%. In the second period:presence of betalactamase 41.9%, ampicillin 53.1%, amoxicillin/clavulanic acid 9.4%, cefuroxime 9.4%, clarithromycin 18.7%, tetracycline 34.4%, ciprofloxacin 15.6%, and cotrimoxazole 68.7%. Resistance of U. urealyticum was: ciprofloxacin 80.7%, ofloxacin 32.4%, erythromycin 17.5%, azithromycin 9.6%, tetracycline 3.5% and doxycycline 0.8%. CONCLUSIONS: N. gonorrhoeae showed a level of resistance to tetracycline and ciprofloxacin higher in the second period, being significant for ciprofloxacin. Quinolone resistance was higher in MSM. Haemophilus spp showed a level of resistance to ampicillin, ciprofloxacin and tetracycline higher in the second period, being significant for tetracycline. U.urealyticum showed high level of resistance to ciprofloxacin (80.7%)and ofloxacin (32.4%) and low level of resistance to doxycycline (0.8%) and tetracycline (3.5%). Supplemental Content Orv Hetil. 2011 Oct 16;152(42):1698-702. [Frequency and antibiotic resistance of Ureaplasma urealyticum and Mycoplasma hominis in genital samples of sexually active individuals]. [Article in Hungarian] Farkas B, Ostorházi E, Pónyai K, Tóth B, Adlan E, Párducz L, Marschalkó M, Kárpáti S, Rozgonyi F. Source Semmelweis Egyetem, Általános Orvostudományi Kar Bőr-, Nemikórtani és Bőronkológiai Klinika Budapest Mária u. 41. 1085 Synlab Hungary Kft. Budapest. Abstract Ureaplasma urealyticum and Mycoplasma hominis have important role among the causative agents of sexually transmitted diseases. AIM: The aim of the study was to determine the frequency and antibiotic resistance of Ureaplasma urealyticum and Mycoplasma hominis in genital samples obtained from patients examined in the Sexually Transmitted Diseases Centre of the Department of Dermatology, Venerology and Dermatooncology, Semmelweis University, Budapest between May 1, 2008 and July 31, 2010. PATIENTS AND METHODS: Samples were taken from the urethra in men and from the cervix and urethra in women by universal swab (Biolab®) into Urea-Myco DUO kit (Bio-Rad®) and were incubated for 48 hours at 37 C°. Antibiotic sensitivity of positive samples was determined in U9 bouillon using SIR Mycoplasma kit (Bio-Rad®). RESULTS: Samples for 4154 patients aged 16-60 years were examined. In 247/4154 samples (6%) U. urealyticum and in 26/4154 samples (0.63%) M. hominis was isolated from the genital tract. Most U. urealyticum and M. hominis strains (75% and 77%, respectively) were cultured from cervix, while the remaining 25%, and 23% from the male and female urethra, respectively. U. urealyticum and M. hominis were most commonly detected in patients aged between 21 and 40 years. The majority of U. urealyticum strains were sensitive to tetracycline (94%), doxycycline (95%), azithromycin (88%) and josamycin (90%), but were resistant to ofloxacin (21%), erythromycin (85%) and clindamycin (79%). Seventy-seven percent of the U. urealyticum strains were simultaneously resistant to erythromycin and clindamycin, suggesting that ex iuvantibus therapies may select cross-resistant strains to both antibiotics. The resistance of M. hominis to clindamycin, doxycycline, ofloxacin and tetracycline varied between 4% and 12 %. CONCLUSIONS: Because none of the strains was sensitive to all examined antibiotics, the antibiotic sensitivity of U. urealyticum and M. hominis strains should be determined. The high rate of ofloxacin, erythromycin and clindamycin resistance should be considered in the therapy of U. urealyticum infections in Hungary. This is the first such a clinical microbiological study in this topic in Hungary. Supplemental Content J Clin Microbiol. 2011 Apr;49(4):1695-6. Epub 2011 Feb 23. Induced macrolide resistance in Mycoplasma genitalium isolates from patients with recurrent nongonococcal urethritis. Supplemental Content Swiss Med Wkly. 2008 Apr 19;138(15-16):243-6. A new sexually transmitted infection (STI) in Geneva? Ciprofloxacin-resistant Neisseria gonorrhoeae, 2002-2005. Le Lin B, Pastore R, Liassine N, Aramburu C, Sudre P. Source General Directorate of Health, Geneva, Switzerland. Abstract PRINCIPLES: Neisseria gonorrhoeae (NG) resistant to ciprofloxacin (CR) was documented for the first time in Geneva in 2002 and increased from 7% that year to 47% in 2005. We describe NG cases during this period and compare characteristics of CR and ciprofloxacin susceptible (CS) cases. METHOD: Geneva microbiological laboratories identified NG cases. Antimicrobial susceptibility testing (AST) was performed on a sample of reported cases. The attending physicians completed questionnaires on demographic and epidemiological characteristics. Risk exposures were assessed by comparing CR and CS cases using logistic regression. RESULTS: 238 NG cases were reported. Of 91 on which AST was performed, 23 (25%) were CR; 91% of these were male vs 87% of CS patients. Men having sex with men (MSM) represented 38% of CR cases compared with 31% of CS cases (p>0.05). Among CR cases 65% were Swiss compared with 56% of CS cases. Median age was 35 years for both. Casual sexual contacts were reported for 88% of CR cases and 72% of CS cases (p>0.05). The difference between CR and CS cases in terms of sexual activity outside Switzerland (50% and 19% respectively) remained significant after adjusting for sexual preference and nationality (OR: 7.0, CI 95: 1.99-24.6). CONCLUSION: Although CR infection was more common among Swiss MSM, only sexual activity outside Switzerland was independently associated with CR. Physicians should request AST before treatment and reconsider first-line use of ciprofloxacin. Surveillance of gonococcal antimicrobial resistance is essential in monitoring epidemiologic trends and updating recommendations on first-line treatment. Supplemental Content Sex Transm Infect. 2008 Oct;84(5):352-5. Epub 2008 Jul 2. Escalation in the relative prevalence of ciprofloxacin-resistant gonorrhoea among men with urethral discharge in two South African cities: association with HIV seropositivity. Lewis DA, Scott L, Slabbert M, Mhlongo S, van Zijl A, Sello M, du Plessis N, Radebe F, Wasserman E. Source STI Reference Centre, National Institute for Communicable Diseases, Private Bag X4, Sandringham 2131, South Africa. [email protected] Abstract OBJECTIVES: The objectives of this study were to assess the prevalence of ciprofloxacin-resistant gonorrhoea in two South African cities and to investigate the association between the isolation of ciprofloxacin-resistant Neisseria gonorrhoeae and the HIV serostatus of patients. METHODS: Gonococci were cultured from endourethral swabs taken from consecutive men with urethritis attending clinics in Johannesburg and Cape Town. Minimum inhibitory concentrations (MIC) for ciprofloxacin and ceftriaxone were determined with E-tests. Isolates with a ciprofloxacin MIC of 1 mg/l or greater were defined as resistant and isolates with a ceftriaxone MIC of 0.25 mg/l or less were defined as susceptible. Rapid tests were used to screen and confirm the presence of HIV antibodies. Survey data from 2004 were used as a baseline to assess trends in gonococcal resistance to ciprofloxacin. RESULTS: In 2004, the prevalence of ciprofloxacin resistance was 7% in Cape Town and 11% in Johannesburg. In 2007, 37/139 (27%) Cape Town isolates and 47/149 (32%) Johannesburg isolates were resistant to ciprofloxacin; in comparison with 2004 data, this represents 2.9-fold and 1.9-fold increases, respectively. All isolates were fully susceptible to ceftriaxone. There was a significant association between HIV seropositivity and the presence of ciprofloxacinresistant gonorrhoea among patients (p = 0.034). CONCLUSIONS: Johannesburg and Cape Town have witnessed significant rises in the prevalence of ciprofloxacin-resistant gonorrhoea among men with urethritis. The resistant phenotype is linked to HIV seropositivity. There is now an urgent need to change national first-line therapy for presumptive gonococcal infections within South Africa. Supplemental Content Euro Surveill. 2009 Sep 17;14(37). pii: 19330. Multidrug-resistant Neisseria gonorrhoeae with reduced cefotaxime susceptibility is increasingly common in men who have sex with men, Amsterdam, the Netherlands. de Vries HJ, van der Helm JJ, Schim van der Loeff MF, van Dam AP. Source STI outpatient clinic, Cluster Infectious Diseases, Municipal Health Service Amsterdam, Amsterdam, The Netherlands. [email protected] Abstract Antimicrobial resistance is an increasing problem in Neisseria gonorrhoeae (NG) treatment. Presently, third-generation parenteral cephalosporins, like ceftriaxone and cefotaxime, are the first option. Resistance to oral, but not to parenteral, third-generation cephalosporins has been reported previously. We analysed the microbial susceptibility (as minimum inhibitory concentration - MIC) of NG cultures obtained from high-risk visitors of the largest Dutch outpatient clinic for sexually transmitted infections (STI) in Amsterdam, the Netherlands. Among 1,596 visitors, we identified 102 patients with at least one NG isolate with reduced susceptibility to cefotaxime (0.125 microg/ml < MIC < or = 0.5 microg/ml). The percentage of NG isolates with reduced susceptibility to cefotaxime rose from 4.8% in 2006 to 12.1% in 2008 (chi2 17.5, p<0.001). With multivariate logistic regression, being a man who has sex with men (MSM) was significantly associated with reduced susceptibility to cefotaxime (p<0.001). Compared to susceptible NG isolates, those with decreased susceptiblity to cefotaxime were more often resistant also to penicillin (16.5% vs. 43.3%), tetracycline (21.5% vs. 68.9%) and ciprofloxacin (44.4% vs. 90.0%, all p<0.001). The increased prevalence of NG strains with reduced susceptibility to cefotaxime among MSM may herald resistance to third-generation parenteral cephalosporins. A considerable proportion of these strains show resistance to multiple antibiotics which could limit future NG treatment options. Supplemental Content Antimicrob Agents Chemother. 2010 Nov;54(11):4893-5. Epub 2010 Aug 23. Characteristics and dissemination of mosaic penicillin-binding protein 2-harboring multidrug-resistant Neisseria gonorrhoeae isolates with reduced cephalosporin susceptibility in northern Taiwan. Huang CT, Yen MY, Wong WW, Li LH, Lin KY, Liao MH, Li SY. Source Research and Diagnostic Center, Centers for Disease Control, No. 161 Kun-Yang Street, Taipei, Taiwan. Abstract Among 254 Neisseria gonorrhoeae isolates from a sexually transmitted infection (STI) clinic in northern Taiwan, 69 isolates were found to contain the mosaic penA (MA) gene and were associated with elevated cefixime and ceftriaxone MICs. Most of these MA gene-harboring isolates were also resistant to penicillin (71.4%) and ciprofloxacin (100%) and were from men who have sex with men (MSM) or from bisexual men (81.2%). Three major sequence types (ST835, ST2180, and ST2253) constituted 55.7% of these isolates. The major sequence types harboring the mosaic penA gene may represent major sexual networks responsible for the emergence/introduction and the spread of the multidrug-resistant clones in Taiwan. Supplemental Content J Health Popul Nutr. 2010 Oct;28(5):443-9. Monitoring antimicrobial susceptibility of Neisseria gonorrhoeae isolated from Bangladesh during 1997-2006: emergence and pattern of drug-resistant isolates. Ahmed MU, Chawdhury FA, Hossain M, Sultan SZ, Alam M, Salahuddin G, Alam A, Nessa K, Nahar S, Shama-A-Waris, Alam A, Rahman M. Source Laboratory Sciences Division, ICDDR,B, GPO Box 128, Dhaka 1000, Bangladesh. Abstract Gonorrhoea is one of the most common sexually transmitted infections (STIs) in developing countries, and the emergence of resistance to antimicrobial agents in Neisseria gonorrhoeae is a major obstacle in the control of gonorrhoea. Periodical monitoring of antimicrobial susceptibility of N. gonorrhoeae is essential for the early detection of emergence of drug resistance. In total, 1,767 gonococcal strains isolated from males and females (general population and those with high-risk behaviour) from different parts of Bangladesh were studied during 1997-2006. Minimum inhibitory concentrations of penicillin, tetracycline, ciprofloxacin, ceftriaxone, spectinomycin, and azithromycin for the isolates were determined by the agar dilution method. Isolates resistant to three or more antimicrobial agents are considered multidrug-resistant. The prevalence of plasmid-mediated penicillinase-producing N. gonorrhoeae (PPNG) and plasmid-mediated tetracycline-resistant N. gonorrhoeae (TRNG) was determined. Nine percent of the isolates were resistant to ciprofloxacin in 1997 compared to 87% in 2006. Multidrug-resistant N. gonorrhoeae have emerged in 1997, and 44% of the strains (n = 66) isolated during 2006 were multidrug-resistant. Forty-two percent of the isolates in 2006 were both PPNG- and TRNG-positive compared to none in 1997. The rapidly-changing pattern of gonococcal antimicrobial susceptibility warrants the need for an antimicrobial susceptibility-monitoring programme, and periodical analysis and dissemination of susceptibility data are essential to guide clinicians and for successful STI/HIV intervention programmes. Supplemental Content