* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiac Cycle - Doctor Jade Main
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac surgery wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Myocardial infarction wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
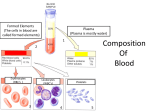
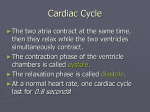
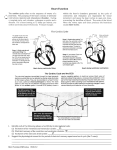
Cardiovascular System-The Heart Cardiovascular System The cardiovascular systesm consists of a series of tubes, the blood vessels filled with fluid, blood connected to a pump, the heart. Arteries carry blood away from the heart and veins carry blood to it. Pressure generated in the heart pumps blood through the system. The primary function is to transport materials to all parts of the body. O2 transport is especially important cells. It also transports hormones for cell to cell communication. It functions in defense in that WBCs and antibodies circulate. It also functions in temperature maintenance by circulating heat. Heart Anatomy The heart is a relatively small, hollow, cone-shaped muscle which sits a little left of the middle of the chest in the mediastinum. It is rest about the size of a fist weighing between 250-350 grams. It is enclosed in the pericardium. The outer layer is called the parietal layer and the inner one is the visceral layer-also called the epicedium. Between the two layers is the pericardial fluid which reduces the friction between layers of the pericardium. Heart Wall Layers The heart consists of three layers: epicardium, myocardium and endocardium. The epicardium is the superficial, visceral layer of the serous pericardium. The myocardium is the middle layer. It is mostly cardiac muscle. It is responsible for the pumping action of the heart. The endocardium is the innermost layer. It consist of a sheet of endothelium resting on a thin connective tissue layer. It is continuous with endothelial lining of blood vessels. Surface of Heart On the anterior surface of each atrium there is a wrinkled, pouchlike structure called an auricle. These slightly increase the capacity of each atrium to hold more blood. A series of grooves or sulci can be found of the surface of the heart; these contain coronary blood vessels. Each sulcus marks the external boundary between two chambers of the heart. A deep coronary sulcus encircles the heart and marks the external boundary between the atria and the ventricles. An anterior interventricular sulcus is a shallow groove on the anterior surface of the heart which marks the external boundary between the right and left ventricles. The posterior interventricular sulcus marks the external boundary between the ventricles on the posterior surface of the heart. Blood Flow & Chambers of the Heart The heart is divided into four chambers-2 atria and 2 ventricles. The two superior chambers are the receiving chambers each called an atrium. They receive blood returning from blood vessels. The two inferior or pumping chambers are the ventricles which return blood to circulation. Blood enters the right atrium via 3 veins:superior vena cava-from body areas superior to diaphragm, inferior vena cava-from areas below diaphragm and coronary sinus-from the myocardium The inside the anterior wall of the right atrium is rough due to the pectinate muscles. Between the right and left atria is a thin partition-the interatrial septum. This contains a small depression, fossa ovalis. This depression is the remainder of a hole in the heart-the foramen ovale found in a fetus. Blood passes from the right atrium to the right ventricle via the tricupspid (right atrioventricular) valve. The wall of the right ventricle consists of bundles of cardiac muscle fibers called the trabeculae carnae. Cusps of the tricuspid value are attached to think cords-the chordate tendineae which are connected to cone shaped papillary muscles. The right ventricles are separated internally from the left ventricles by a partition-the interventricular septum. Blood passes from the right ventricle through the pulmonary (pulmonary semi lunar) valve into the pulmonary trunk which divides into a right and a left pulmonary artery and carries blood to the lungs. The blood returns from the lung to the left atrium via four pulmonary veins. The walls of the left atrium are smooth; there are no pectinate muscles. Blood passes from the left atrium to the left ventricle via the mitral (left atrioventricular) valve. The walls of the left ventricle are the thickest. Since the right ventricle only has to pump to the lungs and the left to all areas of the body, the myocardium is thicker in the left ventricle. Blood passes from the left ventricle through the aortic (aortic semi lunar) valve to the ascending aorta. The first branch is the coronary artery which supplies the heart. In the fetus a ductus arteriosus shunts blood from the pulmonary trunk to the aorta. This closes shortly after birth and becomes the ligamentum arteriosum. Blood Circulation Movement of blood through the heart and around the body is circulation. One way circulation depends upon the valves. There are two types: atrioventricular and semilunar . These open and close in response to blood pressure differences. AV or atrioventricular valves between the atria and the ventricles prevent backflow into the atria when the ventricles contract. When the heart it relaxed, the AV valve flaps hang limply in the ventricular chamber. When the ventricles contract, the blood pressure increases which forces blood superiorly against the flaps; this causes the flap edges to meet and closes the valve. At the same time the papillary muscles contract which pulls on the chordae tendineae which anchors the flaps in the closed position. If not anchored they would go inward like an umbrella in the wind, which is called prolapse. The valves between the ventricles and the vessels leading from it are the semilunar valves, the aortic and the pulmonary. These control flow as blood leaves the heart and prevents back flow into the ventricles. Each valve is made of 3 pocket like flaps, shaped like crescent moons. When the ventricles contract, the intraventricular pressure rises above the blood pressure in the aorta and pulmonary truck. This forces the semilunar valves open, the cusps flatten against the arterial walls as blood rushes past. When the ventricles relax, blood is no longer propelled forward by ventricular contraction pressure and it begins to flows back toward the heart. The blood fills the cusps and closes the valve. Systemic & Pulmonary Circulation Right side or the pulmonary circuit transports blood to and from the lungs for gas exchange. O2 poor/CO2 rich blood from the bodysuperior & inferior venae cavae-systemic veins right atriumright ventriclepulmonary arteries lungsunloads CO2/ picks up O2 pulmonary veinsleft side. The left side or the systemic circuit delivers newly oxygenated blood from the lungs to the left atriumleft ventricleaortasystemic arteriesbranches into smaller and smaller arteriescapillariesgases and nutrients exchange through capillary walls-thin walledloads CO2-depletes O2systemic veinsright side. Cycle repeats continuously. Arteries always carry blood away from the heart and veins always carry blood toward. Most of the time, arteries carry blood that is oxygenated and veins carry blood that is deoxygenated. There are a couple exceptions. Pulmonary arteries leaving the right ventricle carry deoxygenated blood and pulmonary veins carry oxygenated blood. Coronary or Cardiac Circulation One might think that the heart has no problem getting O2 since blood is always in the heart. This blood does not provide nourishment because the myocardium is too thick to allow diffusion to supply nutrients. The heart must have its own source of oxygenated blood which is supplied by the coronary arteries. Right and left coronary arteries arise from the base of the aorta and divide into 2 branches and supplies the myocardium. The left passes inferiorly and divides into the anterior interventricular and circumflex branches. The anterior interventricular branch is in the anterior interventricular sulcus and supplies oxygen to the walls of both ventricles. The circumflex branch lies in the coronary sulcus and distributes blood to the left ventricle wall and the left atrium. The right coronary artery supplies the right atrium; it continues inferiorly to the right auricle to divide into the posterior interventricular and marginal branches. The posterior interventricular branch follows the posterior interventricular sulcus and supplies the walls of the ventricles. The marginal branch transports oxygen to the myocardium of the right ventricle. After passing through capillary beds in the myocardium, venous blood is collected by the coronary veins. These drain into the coronary sinus to bring blood to the right atrium. The principle tributaries carrying blood into the coronary sinus are the: great cardiac vein, middle cardiac vein and the small cardiac vein. Properties of Cardiac Muscle Fibers The heart is comprised of cardiac muscle. Cardiac muscles is called involuntary muscle. Anatomically, it resembles skeletal muscle in that both are striated. Under magnification one can see small stripes running crosswise-myofibrils-A and I band arrangement of actin and myosin. There are large mitochondria which make up2533% of the volume; this reflects the high energy needs. The t tubules are larger and the sarcoplasmic reticulum is smaller. Intercellular spaces are filled with loose connective tissue matrix called the endomysium. The plasma membranes or sarcolemmas of each muscle cells are connected by intercalated discs. These contain desmosomes which prevent cells from separating during contraction and gap junctions which allow ions to pass freely from cell to cell transmitting depolarizing current across entire heart-multiple muscle cells contract rapidly as unit. Cardiac Conduction System The heart has an inherent, rhythmical electrical activity. Due to the presence of specialized cardiac muscle fibers called autorhythmic fibers. These fibers are self excitatory. They initiate contraction without receiving signals from the brain; they initiate their own depolarization. The signal for contraction is myogenic or in the heart itself. These fibers generate action potentials that trigger heart contractions. They have leaky membrane which results in unstable resting potentials. There is an exchange of Na, K and Ca ions which causes a change in polarization and the cells continuously depolarize as the membrane potential drifts slowly toward threshold for firing. Only about 1% of cardiac fibers are autorhythmic. These are called pacemakers because they set the rhythm of electrical excitation that causes contraction of the heart. These fibers form the cardiac conduction system, a network of specialized cardiac muscle fibers that provide a path for cardiac excitability. Cardiac excitation begins in the SA-sinoatrial node, a crescent shaped area located in the wall of the right atrium. Cells here depolarize spontaneously. They contract about 75X per minute which sets the pace for the heart; no other area has a faster depolarization rate making the SA node the main pacemaker. The cells in the SA node would initiate an action potential every 0.6 seconds or 100X per minute if allowed to contract as they wanted; however hormones and parasympathetic fibers of the autonomic nervous system slow the SA node pace to every 0.8 or 75X per minute. The pacemaker triggers an action potential which causes the two atria to contract at the same time. The action potential is then conducted along the atrial muscle fiber to the AV-atrioventricular node located in the interatrial septum near the center of the heart. Here the impulse is delayed about 0.1 sec. This allows the atria to respond and empty blood into the ventricles. From the AV node the impulse travels to the Bundle of His or the atrioventricular bundle. After propagating along the AV bundle the action potential enters the right and left bundle branches. These extend along the interventricular septum toward the apex where they divide into the purkinje fibers which rapidly conduct the action potential to the apex of the heart and upward to the remainder of the ventricular myocardium. This causes the ventricles to contract pushing blood upward toward the semi-lunar valves. Action Potential of the Heart The action potential of the heart is similar to that seen in neurons and skeletal muscles. Rapid depolarization is due to Na entry. Na permeablity returning to resting level begins repolarization. One difference is that the action potential in the heart is lengthened due to Ca entry. The resting potential of heart muscles is -90mV. As the action potential depolarizes the membrane voltage gated Na channels open Na entersrapid depolariztion. Within a few milliseconds the fast Na channels are inactivated and Na inflow decreases and the cell begins to repolarize. At this time the action potential flattens into a plateau, a period of maintained depolarization due in part to opening of voltage-gated slow calcium channels. Calcium ions move from the interstitial fluid into the cytosol which caused more inflow of Ca from the sarcoplasmic reticulum. The increased calcium triggers contraction. Voltage-gated K channwels also begin to open and K begins to leave the muscle cells. Both of these maintain depolarization which lasts abouat 0.25 seconds. Recovery of the resting membrane potential is repolarization due to opening of more voltage-gated K channels. Outflow of K restores the resting membrane potential. Muscle tension develops during the plateau stage and peaks just after the plateau ends. Longer action potentials help prevent sustained contraction or tetanus. This is important; the cells must relax between contractions so the ventricles can fill with blood. In skeletal muscle one action potential is ending as contraction begins, a second action potential immediately after refractory period will cause summation of contractions. If there is series of action potentials in rapid successiontetanus. This cannot occur in cardiac muscle. The period of time when a second contraction cannot be triggered is called the refractory period. In the heart this period lasts longer than the contraction. Another contraction cannot be elicited until relaxation has begun. This means tetanus cannot occur. Heart Contraction Contraction of the heart is due to calcium. The mechanism is similar to that of skeletal muscle cells. The action potential is triggered in contractile cells by a sequence of electrical events similar to skeletal muscles. There is an influx of Na+ from extracellular fluidregulated fast Na channels openincreases Na permeability rising phase of action potentialreversal of membrane potential from 90mv to +30mv. Depolarization is transmitted down the t tubules sarcoplasmic reticulum releases Ca++ into sarcoplasm. Influx of Catriggers release of Ca from the SR which provides 90% of the Ca needed for contraction. Ca diffuses thorugh the cytosol to bind to troponin which starts cross bridge formation. During relaxation Ca unbinds from troponin, Ca-ATPase aids transport of Ca back in the SR. ECG-EKG-Electrocardiography As action potentials propagate through the heart they generate an electrical current that can be detected on the surface of the body. An EKG is a recording of these electrical signals. It is recorded by an electrocardiograph which amplifies the heart’s electrical activity made by placing electrodes on the skin’s surface. An EKG shows the sum of electrical potentials generated by all cells of heart at any moment-each component reflects depolarization and repolarization of a part of the heart. An EKG consists of 3 deflection waves. The P-Wave is a small upward deflection that represents depolarization of the atria. The QRS complex depicts ventricular depolarization. It begins as a downward deflection and continues as long as a large upright wave and ends in a downward deflection. The T-Wave shows ventricular repolarization. Atrial repolarization occurs during ventricular excitation but is obscured by the QRS complex. The EKG trace can tell a great deal about the heart. An enlarged R indicates an enlarged ventricle, a flattened T reflects cardiac ischemia, a prolonged Q-T indicates a repolarization problem. Cardiac Cycle All of the events associated with blood flow through the heart during one complete heartbeat includes one contraction and one relaxation which is called the cardiac cycle. Each cycle includes 2 phases, a contraction or systole and a relaxation or diastole of both the atria and the ventricles. The EKG give the electrical events which are key to the mechanical events; the electrical events precede the mechanical ones. Pressure and volume changes during the cardiac cycle are responsible for the movement of blood through the system. In each cardiac cycle the atria and the ventricles alternately contract and relax forcing blood from areas of higher to areas of lower pressure. As a chamber of the heart contracts the blood pressure increases within it. When the heart rate is 75 beats/minute a cardiac cycle lasts 0.8 seconds. A cardiac action potential begins at the SA node and propagates through the atrial muscle and down to the AV node; as the atrial contractile factors depolarize the P wave is seen. After the P wave begins atrial systole begins. Atrial systole lasts 0.1 seconds; the atria are contracting at this time. As the atria contract they exert pressure on the blood within them which forces blood through the open AV valve into the ventricles. Atrial systole contributes the final 25mls of blood to the volume of blood already in each ventricle (105ml) which flowed into them during the passive filling part of ventricular diastole. This is called completion of ventricular filing. The end of atrial systole also is the end of ventricular diastole. Ventricular volume is at its greatest at this point. This volume is labeled the End-diastolic volume (EDV) and is the volume of blood in each ventricle at the end of diastole. It is the maximum amount blood they can hold. The ORS wave of the EKG marks the onset of ventricular depolarization and ventricular systole begins. It lasts about 0.3 seconds. The ventricles are contracting at the same time the atria are relaxing (atrial diastole). Ventricular depolarization causes ventricular systole. As systole begins the pressure rises inside the ventricles and pushes blood up against the AV valves forcing them shut. The vibration from closure is the first heart sound-lubb. Since there is no change in ventricular volume (both AV and semilunar values are closed), this is called isovolumetric contraction. Continued contraction of the ventricles causes pressure inside the chambers to rise sharply and when the left ventricular pressure surpasses the aortic pressure and the right ventricular pressure rises above the pressure in the pulmonary trunk, both semilunar valves open. At this point ejection of blood begins-ventricular ejection. This phase lasts 0.25 seconds. Pressure in the right and left ventricles continues to rise. Both ventricles eject the same volume of blood; about 70mls. This volumes is labeled the stroke volume, the volume of blood ejected from each ventricle in a single beat. The amount of blood remaining in each ventricle at the end of systole is called the ESV-end systolic volume. SV = EDV –ESV. The T wave marks the beginning of ventricular repolarization. Relaxation lasts 0.4 seconds. As heart rate increases the relaxation phase gets shorter. The atria and the ventricles are both relaxed. Ventricular repolarizaton causes ventricular diastole. As the ventricles relax, the pressure falls causing blood in the aorta and pulmonary truck to fall back. The blood is caught in the cusps of the semilunar vales causing them to close. The vibrations produce the second heart sound-dupp. Closure of the aortic semilunar valve causes a brief rise in aortic pressure which appears on a trace of the heart beat as the dicrotic notch. After the semilunar values close this is called isovolumetric relaxation. As the ventricles continue to relax, pressure falls quickly. When ventricular pressure falls below atrial pressure the AV valves open and ventricular filling begins. This is called passive filling which accounts for 70-80% of ventricular filling. Heart Sounds There are four heart sounds: S1, S2, S3 and S4. Normally only S1 and S2 are loud enough to be heard. This is typically done with a stethoscope and is called auscultation. Heart sounds S1 and S2 are the result of valves closing as discussed above. Heart sounds S3 and S4 are only heard if there is a problem. S3 is the due to rapid ventricular filling and S4 is the result of atrial systole. Cardiac Output Body cells must receive a certain amount of oxygen from the blood each minute to maintain health and life. This is different for when the body is at rest and when it is exercising. The amount of blood pumped by one ventricle during contraction measured-mL/beat, at rest is 70mL. This is not constant; it can increase to 100mL during exercise. Cardiac output is the amount of blood pumped/ventricle/unit time. The volume of blood ejected from each ventricle each minute. It indicates total blood flow through the body. CO=heart rate X SV. CO=75bpm X 70mL/beat. CO = 5/25L. This is close to the average total blood volume in males of 5L. This means that one’s entire blood volume flows through the pulmonary and systemic circuits each minute. The CO can rise to 30-35L/minute when one is exercising. Stroke volume and heart rate can both increase (or decrease) cardiac output. Regulation of Stroke Volume There are three factors that regulate stroke volume: preload, contractility and afterload. Preload is the degree of stretch on the heart before contraction. Contractility is the forcefulness of contraction and afterload is the pressure that must be exceeded before ejection of blood can occur. Preload is the effect of stretching. A greater preload (stretch) on cardiac muscle fibers prior to contraction increases their force of contraction. The more the heart fills with blood during diastolethe greater the force of contraction during systole. This relationship is called the Frank-Starling Law of the Heart. Preload is proportional to the EDV. According to this law, the more blood in the ventricle at the start of the contraction, meaning there is an increased EDVthe greater the SV. Two key factors determine EDV: 1) duration of ventricular diastole and 2) venous return, the volume of blood returning to the right atrium. When heart rate increasesthe duration of diastole is shorterless filling timesmaller EDV. The ventricles may contract before being adequately filled. When venous return increasesa greater volume of blood flows into the ventricles and the EDV is increased. When the heart rate exceeds 160 beats/minutes, the stroke volume usually declines due to the short filling time. EDV is less and preload is lower. Contractility is the strength of contraction at any given preload. Substances that increase contractility are called positive inotropic agents. Thos that decrease contractility are called negative inotropic agents. For a constant preload, the SV increases when a positive inotropic agent is present. These agents often promote calcium inflow which strengthens the force of the next contraction. Stimulation of the sympathetic division of the AND, hormones (norepinephrine and epinephrinecatecholamines), increases calcium all have positive inotropic effects. Inhibition of the sympathetic nervous system, anoxia, increased postassium, acidosis are negative inotropic agents. Afterload is the pressure that must be overcome before a semilunar valve can open. An increase in afterload causes the SV to decrease so more blood remains in the ventricles at the end of systole. Hypertension, narrowing of arteries both increase afterload. Regulation of Heart Rate Adjustments in heart rate are important in the short term control of CO and blood pressure. The most important regulators are the ANS and hormones of the adrenal medulla-epinephrine and norephrine (catecholamines). Sympathetic and parasympathetic neurons of the ANS influence through antagonistic control. Parasympathetic fibers slow and sympathetic fibers increase heart rate. Parasympathetic fibers are involved in tonic control. In order to get a heart rate of 75bpm, tonic parasympathetic activity slows the intrinsic rate of 100bpm. Nervous system regulation of the heart begins in the cardiovascular center in the medulla. As physical activity begins proprioceptors monitoring the position of limbs and muscles send impulses at an increased frequency to the cardiovascular center. Other sensory receptors sending messages to the cardiovascular center are chemoreceptors and baroreceptors. Chemoreceptors monitor chemicals in the blood such as oxygen and hydrogen ions. Baroreceptors monitor blood pressure. These will be discussed when we discuss blood vessels. Sympathetic neurons extend form the medulla into the spinal cord. From the spinal cord sympathetic cardiac accelerator neurons extend to the SA and AV nodes and to most of the myocardium of the heart. These neurons release norepinephrine which binds to Beta-1 receptors on cardiac muscle cells. This has two effects. First at the SA and AV nodes it speeds the rate of spontaneous depolarization which causes the pacemaker to fiber more quickly and increases the heart rate. Second, in the atria and ventricles, norepinephrine enhances the entrance of calcium. This increases the contractility and more blood is ejected during systole. With a moderate increase in heart rate, the stroke volume does not decline because the increased contractility offsets the decreased preload. With maximum sympathetic activity, heart rate can increase to 200beats/minute. At this rate stroke volume is lower due to a short filling time. Parasympathetic neurons reach the heart via the right and left vagus nerve. They terminate in the SA and AV nodes and in the atrial myocardium and slow the rate of spontaneous depolarization. Chemical regulation of the heart rate is in response to hormones and other cations in the blood such as oxygen and hydrogen ions. Hormones form the adrenal medulla enhance the heart’s pumping effectiveness. These affect heart muscle fibers in the same way as norepinephrine released by neurons; they increase heart rate and contractility. Exercise, stress, and excitement cause the release of these hormones. Sodium and potassium are crucial to action potential production and calcium is needed for muscle contraction. Therefore the concentrations of these hormones have a huge effect on cardiac function. Increased potassium and sodium decrease heart rate and contractility. Excess sodium blocks the influx of calcium during an action potential and decreases contractility. Potassium blocks action potential generation and calcium increases speed and strengthen the heart rate.