* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download File
Sexually transmitted infection wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Chagas disease wikipedia , lookup
Sarcocystis wikipedia , lookup
Trichinosis wikipedia , lookup
Herpes simplex wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Anaerobic infection wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Hepatitis C wikipedia , lookup
Onchocerciasis wikipedia , lookup
Gastroenteritis wikipedia , lookup
Hepatitis B wikipedia , lookup
Schistosomiasis wikipedia , lookup
Neonatal infection wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
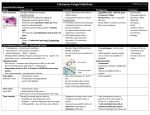
Athlete's foot wikipedia , lookup
Fungal infections Dermatophytic infections (ringworm) CAUSE Three genera of dermatophyte fungi cause tinea infections (ringworm). Trichophyton – skin, hair and nail infections. Microsporum – skin and hair. Epidermophyton – skin and nails.. Dermatophytes invade only into the stratum corneum The inflammation they cause is a result of metabolic products of the fungus OR Delayed hypersensitivity PRESENTATION AND COURSE The site and on the strain of fungus involved Tinea of the scalp (tinea capitis) Tinea of the trunk and limbs (tinea corporis) Tinea of beard (Barbae) Tinea of the nails (unquium) Tinea pedis (athlete’s foot) Tinea of the groin (T. cruris) TINEA PEDIS (ATHLETE’S FOOT) Most common type of fungal infection in humans. Trichophyton rubrum (the most common) The sharing of wash places (e.g. in showers) and of swimming pools predisposes to infection Spores in occlusive footwear encourage relapses Hyperhidrosis of sole Tinea unguium 1. 2. 3. There are three common clinical patterns. Soggy interdigital scaling, particularly in the fourth and fifth interspace,when complicated by bacterial superinfection labeled athlete’s foot. A diffuse dry scaling of the soles (usually T. rubrum) Recurrent episodes of vesication (usually T.mentagrophytes) TINEA OF THE NAILS /ONYCHOMYCOSIS) Tinea unquium Toe nail infection is usually associated with tinea pedis. The initial changes occur at the free edge of the nail, which becomes yellow and crumbly Followed by hyperkeratosis, separation of the nail from its bed and thickening(onycholysis) Usually, only a few nails are infected & rarely all Finger nail lesions are similar, but less common TINEA OF THE HANDS/TINEA MANUUM Usually asymmetrical Associated with tinea pedis and unilateral onychomycosis. Unilateral well defined plapues or as diffuse erythema of palm with a characteristic powdery scale in the creases. TINEA OF THE GROIN/TINEA CRURIS This is common and affects men more often than women. Predisposing factors:summers or winter or occlusion by use of synthetic clothes The eruption is sometimes unilateral or asymmetrical. The upper inner thigh is involved Lesions expand slowly to form sharply demarcated plaques with peripheral scaling. Scrotum is usually spared. A few vesicles or pustules may be seen within the lesions. TINEA OF THE TRUNK AND LIMBS/TINEA CORPORIS Characterized by annular or arcuate plaques with scaling and erythema most pronounced at the periphery, relative clearing in the center and active periphery. Few small vesicles and pustules may be seen within them. Lesions expand slowly and healing in the centre leaves a typical ringlike pattern. TINEA OF THE SCALP (TINEA CAPITIS) Usually a disease of children Discoid patch of partial alopecia from which the hair can easily and painlessly be plucked. Causative organism varies Fungi coming from human sources (anthropophilic organisms)cause bald and scaly areas With minimal inflammation Fungi coming from animal sources (zoophilic fungi) induce a more intense inflammation In ringworm acquired from cattle -swelling, with inflammation, pustulation and lymphadenopathy-bacterial infection is suspected Lesion is called a kerion The hair loss associated with it may be permanent. Favus : caused by T.schoenleinii Characterized by presence of foul smelling yellowish cup shaped crusts entangling many scalp hair. Often results in cicatricial alopecia COMPLICATIONS Fierce animal ringworm of the scalp can lead to a permanent scarring alopecia. A florid fungal infection can induce vesication on the sides of the fingers and palms Epidemics of ringworm occur in schools. The usual appearance of a fungal infection can be masked by mistreatment with topical steroids(tinea incognito) ‘Tinea incognito’. Topical steroid applications have thinned the skin and altered much of the morphology. A recognizable active spreading edge is still visible. DIFFERENTIAL DIAGNOSIS Area Differential diagnosis Scalp Alopecia areata, psoriasis, seborrhoeic eczema, carbuncle, abscess Feet Erythrasma, eczema Trunk Discoid eczema, psoriasis, candidiasis, pityriasis rosea Groin Candidiasis, erythrasma, irritant and allergic contact dermatitis, psoriasis, neurodermatitis Nails Psoriasis, paronychia, trauma, ageing changes Hand Chronic eczema, xerosis, INVESTIGATIONS Microscopic examination of a skin scraping nail clipping or plucked hair in KOH mount Cultures Wood’s light (ultraviolet light) examination of the scalp usually reveals a green fluorescence of the hairs. TREATMENT Local Imidazole preparations (e.g. Miconazole & and Clotrimazole and ketoconazole) Terbinafine Applied twice daily Amorolfine and Tioconazole nail solutions Systemic For tinea of the scalp or of the nails For widespread or chronic infections of the skin that have not responded to local measures. Terbinafine Itraconazole Griseofulvin (drug of choice for chronic dermatophyte infections) CANDIDIASIS CAUSE Opportunistic pathogen Candida albicans, a dimorphous fungus existing as commensal in oral mucosa (50% of normal humans )and vaginal (25%of normal women) Commensal becomes pathogenic in presence of following predisposing factors: Diabetes Other endocri. Antibiotics Obesity (friction) Poor hygiene candidiasis Cold hands Immersion in water Pregnancy Oral contraceptive High humidity, Occlusive clothes Immunosuppression Systemic candidiasis (rare) Leucopenia Thymic tumours Inherited defects of immunity Chronic Mucocutaneous candidiasis (rare) Endocrinopathy TYPES Systemic Chronic mucocutaneous Acute mucocutaneous ACUTE MUCOCUTANEOUS: CANDIDA INTERTRIGO /FLEXURAL A moist glazed area of erythema and maceration in body fold The edge shows soggy scaling and outlying satellite papulopustules. Most common under the breasts and in the armpits and groin Can also occur between the fingers Typical lesion: • Central denudation leaving a fiery red, raw surface • Thick, white plaques at periphery ORAL CANDIDIASIS Acute pseudomembranous candidiasis(thrush): most common form Seen in infants or elderly with antibiotics or steroids therapy Presents with white adhernt plaques which are difficult to remove On removal erythematous base is revealed. Seen over buccal mucosa, tongue, palate and gingiva. Acute atrophic candidiasis: patchy depapillated area over the dorsum of tongue Angular stomatitis Oral Candidiasis GENITAL CANDIDIASIS Presents as a sore itchy vulvovaginitis White curdy plaques adherent to the inflamed mucous membranes Whitish discharge In males- similar changes occur under the foreskin and in the groin Diabetes, pregnancy and antibiotic therapy are common predisposing factors. PARONYCHIA Acute paronychia is usually bacterial In chronic paronychia Candida may be the sole pathogen OR It may be found with other opportunists such as Proteus or Pseudomonas sp. Proximal and sometimes the lateral nail folds of one or more fingers become rolled and red The cuticles are lost and small amounts of pus can be expressed. The adjacent nail plate becomes ridged and discolored. Predisposing factors include wet work, diabetes and vulval candidiasis. CHRONIC MUCOCUTANEOUS CANDIDIASIS Persistent candidiasis Can start in infancy Autosomal recessive and dominant inheritance forms In the Candida endocrinopathy syndrome, chronic candidiasis occurs with one or more endocrine defects Hypoparathyroidism Addison’s disease. Late-onset cases have underlying thymic tumours. Manifest over oral mucosa or skin or nails. SYSTEMIC CANDIDIASIS Usually seen with Severe illness Leucopenia Immunosuppression Lethal within days, without treatment Cutaneous or visceral inf. Skin lesions are firm red nodules, which can be shown by biopsy Contain yeasts Pseudohyphae. INVESTIGATIONS KOH mount shows budding yeast and pseudohyphae Swabs from suspected areas for culture Urine for sugar In chronic mucocutaneous candidiasis Detailed immunological work-up TREATMENT Predisposing factors should be sought and eliminated Infected skin folds should be separated and kept dry Chronic paronychia -keep their hands warm and dry Topical nystatin and the azole group of compounds are effective and topical or oral antibiotic if associated infection Oral suspensions and oral gels for oral lesions. Imidazole pessaries or topical azoles for genital lesion False teeth should be removed at night, washed and steeped in antiseptic or a nystatin solution. Systemic therapy: Vulvovaginitis;single dose fluconazole 150mg or itraconazole400mg.weekly dose of fluconazole 150mg for recurrent problem. For reccurent oral lesion; fluconazole 150mg weekly dose. In chronic paronychia, the nail folds can be packed with an imidazole cream or drenched in an imidazole solution several times a day. Genital candidiasis responds well to a single day’s treatment with either Itraconazole and Fluconazole. PITYRIASIS VERSICOLAR Chronic often asymptomatic Fungal infection characterised by pigmentary changes. Commonly involves the trunk. PRESENTATION • • • • • Caused by overgrowth of mycelial form of commensal yeast pityrosporum ovale/malassezia furfur Common in humid region Common in young adults In white people ,brown or pinkish oval or round superficial scaly patch is seen In racially pigmented or tanned skin hypopigmented patch is seen as organism releases carboxylic acid that inhibit melanogenesis. DIFFERENTIAL DIAGNOSIS Vitiligo:differentiation is done by microscropic examination of the skin scraping:p.versicolar shows short hyphae and spores has grapes and banana appearance. Tinea corporis Pityriasis rosea. MANAGEMENT Topical antifungals:ketoconazole Shampoo(2.5%slenium sulphide) applied at night and washed off the following morning .Repeated twice at weekly interval. Systemic: Iatraconazole Ketoconazole Fluconazole