* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Fungal skin infections
Survey
Document related concepts
Transcript
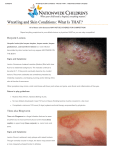
Fungal skin infections Tinea / ringworm Recommend Prevent transmission of ringworm/s. Always treat secondary infection Perform a skin scraping from the edge of an affected area for microscopy/mycology if there is any doubt about the diagnosis Background Tinea or ringworm can infect any part of the person’s skin, hair and nails [6]. It is caused by dermatophytes – a fungus parasite and has a typical appearance which is described as annular (forming a ring) or arcuate (bow shape). It is usually scaly and itchy with a definite edge and central clearing as it expands [6] Transmission is fostered by overcrowding, shared bathroom facilities, poor hygiene, humid conditions and malnourished state Can be transmitted by direct contact with others or by infected animals or by objects such as combs, caps, clothing, footwear, linen and wet floors Related topics: Bacterial skin infections, page 279 1. May present with: Tinea corporis may be diverse in its presentation but most commonly presents as an itchy lesion or rash with an advancing irregularly shaped raised red scaly border with central clearing. Excoriation from scratching and secondary infection is common Tinea capitus also has a variable appearance ranging from small lumps about the hair shafts to a kerion, which is an inflammatory boggy mass studded with broken hairs and oozing purulent material. It is usually itchy or painful. Occurs almost exclusively in children [6] Tinea cruris predominantly occurs in males. Unlike candidiasis, satellite lesions are unusual. Often the inner thigh is affected Tinea pedis usually occurs between the toes and is characterised by itching, scaling and fissuring. Secondary infection is common and this may be a site of entry of streptococcal infection 2. Immediate management: not applicable 3. Clinical assessment: Obtain a complete patient history including environmental history past episodes is the skin itchy / painful? length of time condition has been present do any other members of their family / close contacts have the same skin lesions? ask if any measures have been used to treat, topical creams / ointments? medication history Perform standard clinical observations, + BGL Review nutritional status Perform physical examination (wear gloves) inspect all skin surfaces, nails and hair is there evidence of scaly lesions? with central clearing? are there scratches on the skin? broken skin from scratching? describe the shape are the lesions? describe the part of the body where they are present? is there signs of secondary infection? o redness, pustules, heat, swelling? 4. Management: Consult MO if there is widespread skin involvement or tinea capitus present Perform a skin scraping from the edge of an affected area for microscopy/mycology if there is any doubt about the diagnosis Treat any secondary bacterial infection first (see Impetigo) Efforts to decrease occlusion and moisture are helpful. This can be done by avoiding synthetics, and wearing lighter and better ventilated clothing and footwear, and by the judicious use of an absorbent powder For isolated lesions treat with a topical agent such as Miconazole 2% or Clotrimazole 1% Schedule 2 Miconazole DTP IHW / IPAP / NP Authorised Indigenous Health Workers and Isolated Practice Area Paramedics may proceed Nurse Practitioners may proceed Route of Form Strength Recommended Dosage Duration Administration Cream 2% Topically Apply topically 2-3 times daily Apply until lesion clears plus a few days Management of Associated Emergency: Consult MO Or: Schedule 2 Clotrimazole DTP IHW / IPAP / NP Authorised Indigenous Health Workers and Isolated Practice Area Paramedics may proceed Nurse Practitioners may proceed Route of Form Strength Recommended Dosage Duration Administration Lotion 1% Topically Apply topically 2-3 times daily Apply until lesion clears plus a few days Management of Associated Emergency: Consult MO 5. Follow up: Review the patient in 2 weeks See next MO clinic if: widespread skin involvement tinea capitis fingernails or toenails involved (these patients usually require oral antifungal treatment (eg. Griseofulvin) 6. Referral / Consultation: Consult MO as above