* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Best Practice - The Heart Foundation
Cardiac contractility modulation wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Heart failure wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Electrocardiography wikipedia , lookup
Rheumatic fever wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Jatene procedure wikipedia , lookup
Saturated fat and cardiovascular disease wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
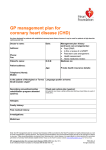
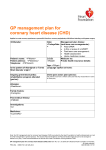
GP management plan for coronary heart disease (CHD) Has been designed for patients with established coronary heart disease however it may be used for patients at high absolute cardiovascular risk. Doctor’s name: <DrName> Patient’s name: <PtName> Management plan history (and team care arrangements): Past GPMP: <Past GPMP> Is this a review of a GPMP? <Is this a review of a GPMP?> Past team care arrangement: <Past team care arrangement> Health assessment: <Health assessment> Home medicines review: <Home medicines review> D.O.B: <PtDoB> Medicare no: <PtMCNo> Patient address: <PtAddress> Age: <PtAge> Address: <DrAddress> Phone: <DrPhone> Fax: <DrFax> Date: <TodaysDate> Private health insurance details: <PtHealthIns> Telephone Home: <PtPhoneH> Mobile: <PtPhoneMob> Is the patient of Aboriginal or Torres Language spoken at home: <What language is spoken Strait Islander origin? <Aborginal or at home?> Torres Strait Islander origin?> Secondary prevention/cardiac Chest pain action plan (yes/no): (All patients must have a written action plan that they should follow in event of rehabilitation program attended chest pain.) <Chest pain action plan> (yes/no): <Cardiac rehabilitation program attended> Allergies: <Reactions> Family history: <FamilyHx> Past medical history: <PMHAll> Investigations: <Ix> Medicines: <CurrentRx> Note: the GP management plan for coronary heart disease (CHD) is provided by the Heart Foundation to health professionals as a tool for CHD management in general practice. The sections recommendations and recommended targets should not be changed or altered in any way. These recommendations are derived from Reducing risk in heart disease. An expert guide to clinical practice for secondary prevention of coronary heart disease (Update 2012). Please see the Heart Foundation website at www.heartfoundation.org.au for Terms of Use. GP management plan for coronary heart disease (CHD) (MBS Item No. 721) © 2013 National Heart Foundation of Australia ABN 98 008 419 761 1 PRO-084-v2-BP All rights reserved. Medicine Commenced/ Continued. If no, what reason Yes No Medicines Discussed benefits and side effects? Yes Recommendation Unless otherwise indicated, all recommendations derived from National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand Reducing risk in heart disease. An expert guide to clinical practice for secondary prevention of coronary heart disease (Update 2012). No Antiplatelet agents Use aspirin 75–150 mg/day for all patients unless contraindicated. Clopidogrel can be used where aspirin is contraindicated, or with aspirin in patients who have recurrent events or following treatment for ACS (either fibrinolysis or stenting). ACE inhibitors (ACEI)/Angiotensin II receptor antagonists (ARA) Recommended for all patients, especially those at high risk of recurrent events, unless contraindicated. Start early post myocardial infarction (MI). Consider ARA for patients who develop unacceptable side effects on ACEI. Beta-blockers Recommended for all patients post MI, unless contraindicated, and continued indefinitely, especially in high-risk patients. (High-risk patients are defined as those with either significant myocardial necrosis, left ventricular systolic dysfunction, persistent evidence of ischaemia or ventricular arrhythmia.) Statins Recommended for all patients, unless contraindicated. Anticoagulants Use warfarin in patients at high risk of thromboembolism due to AF post MI. Aldosterone antagonists Epleronone may be used early (3-14days) post MI in patients with left ventricular systolic dysfunction and symptoms of heart failure. Medicine adherence If poor adherence suspected, consider a Home Medicine Review. Short-acting nitrates Recommended for all patients, unless contraindicated, plus a written action plan for chest pain. Other Note: the GP management plan for coronary heart disease (CHD) is provided by the Heart Foundation to health professionals as a tool for CHD management in general practice. The sections recommendations and recommended targets should not be changed or altered in any way. These recommendations are derived from Reducing risk in heart disease. An expert guide to clinical practice for secondary prevention of coronary heart disease (Update 2012). Please see the Heart Foundation website at www.heartfoundation.org.au for Terms of Use. GP management plan for coronary heart disease (CHD) (MBS Item No. 721) © 2013 National Heart Foundation of Australia ABN 98 008 419 761 2 PRO-084-v2-BP All rights reserved. Risk factor Smoking Lifestyle/Psychosocial risk factors Patient agreed Current goals and actions Recommended targets status (how, who and by when) <SmkStat Complete cessation us> and avoidance of second-hand smoke. Physical inactivity Progress, over time, to at least 30 minutes of moderate-intensity physical activity on most, if not all, days of the week (150 minutes per week minimum). Nutrition Establishment/ maintenance of healthy eating patterns, with saturated fatty acid intake <7% and trans fatty acid intake <1% of total energy intake. Include 1g of eicosapentaenoic acid (EPA) + docosahexaenoic acid (DHA) and >2g of alpha linolenic acid (ALA) daily. Limit salt intake to ≤4g/day (1550mg sodium). Healthy weight Waist measurement ≤ 94 cm (males) or ≤ 80 cm (females); BMI = 18.5-24.9 m2. (Weight management goals based on studies of European populations and may not be appropriate for all ages and ethnic groups.) Alcohol Low risk alcohol consumption in people who drink. ≤ 2 standard drinks per day or ≤ 1 standard drink per day for women with high blood pressure or who are taking antihypertensive medicine. Depression Assess all patients for co-morbid depression. Initiate psychosocial and medical management if appropriate. Social support Assess all patients for level of social support and provide follow-up for people considered at risk by referral to cardiac rehabilitation and/or social worker or psychologist. Warning signs of heart attack: action plan Provide written information and an action plan for patients to follow in the event they have warning signs of heart attack. Other Note: the GP management plan for coronary heart disease (CHD) is provided by the Heart Foundation to health professionals as a tool for CHD management in general practice. The sections recommendations and recommended targets should not be changed or altered in any way. These recommendations are derived from Reducing risk in heart disease. An expert guide to clinical practice for secondary prevention of coronary heart disease (Update 2012). Please see the Heart Foundation website at www.heartfoundation.org.au for Terms of Use. GP management plan for coronary heart disease (CHD) (MBS Item No. 721) © 2013 National Heart Foundation of Australia ABN 98 008 419 761 3 PRO-084-v2-BP All rights reserved. Risk factor Lipids Blood pressure Current status Biomedical risk factors Patient agreed goals and actions Recommended targets (how, who and by when) LDL-C < 1.8 mmol/L; HDL-C > 1.0 mmol/L; Triglycerides (TG) < 2.0 mmol/L; non-HDL-C < 2.5 mmol/L. BP < 130/80 mmHg including patients with or without diabetes and/or stroke/TIA and/or microalbuminuria.. Ambulatory BP measurements: < 135/85 mmHg for daytime, < 120/75 mmHg for night time, and < 130/80 mmHg for 24 hours. (Microalbuminuria – men > 2.5 mg/mmol; women > 3.5 mg/mmol) Diabetes Identify undiagnosed type 2 diabetes; maintain optimal BSL in those with diabetes (HbA1c ≤ 7%). Other conditions Other considerations Implement a patient-centred approach, setting realistic goals and time frames in consultation with the patient. Consider strategies to support self-management, assess readiness for change and explore barriers. Provide written information and self-management resources, such as My heart for life and My heart my life, that are available from the Heart Foundation. Consider referral if appropriate. For heart health information call 1300 36 27 87 or visit www.heartfoundation.org.au Note: the GP management plan for coronary heart disease (CHD) is provided by the Heart Foundation to health professionals as a tool for CHD management in general practice. The sections recommendations and recommended targets should not be changed or altered in any way. These recommendations are derived from Reducing risk in heart disease. An expert guide to clinical practice for secondary prevention of coronary heart disease (Update 2012). Please see the Heart Foundation website at www.heartfoundation.org.au for Terms of Use. GP management plan for coronary heart disease (CHD) (MBS Item No. 721) © 2013 National Heart Foundation of Australia ABN 98 008 419 761 4 PRO-084-v2-BP All rights reserved. Administration details Date plan/service completed: <Date Plan/Service Completed> Proposed review date(s): <Proposed Review Date> Copy of CHD management plan offered to Copy of CHD management plan added to patient? <Copy of CHD management plan patient’s records? <Copy of CHD management offered?> plan added to record?> Other notes or comments: Patient’s agreement I agree with the goals of this plan and I understand the recommendations, including the costs involved. Patient’s signature: _______________________________________ Date: ______________ Patient’s name (in print): __________________________________________________________ I have explained the steps and any costs involved, and the patient has agreed to proceed with this plan. GP’s signature: __________________________________________ Date: _______________ Note: the GP management plan for coronary heart disease (CHD) is provided by the Heart Foundation to health professionals as a tool for CHD management in general practice. The sections recommendations and recommended targets should not be changed or altered in any way. These recommendations are derived from Reducing risk in heart disease. An expert guide to clinical practice for secondary prevention of coronary heart disease (Update 2012). Please see the Heart Foundation website at www.heartfoundation.org.au for Terms of Use. GP management plan for coronary heart disease (CHD) (MBS Item No. 721) © 2013 National Heart Foundation of Australia ABN 98 008 419 761 5 PRO-084-v2-BP All rights reserved.