* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Dear Notetaker:
Stimulus (physiology) wikipedia , lookup
Cardiac output wikipedia , lookup
High-altitude adaptation in humans wikipedia , lookup
Intracranial pressure wikipedia , lookup
Hemodynamics wikipedia , lookup
Biofluid dynamics wikipedia , lookup
Homeostasis wikipedia , lookup
Circulatory system wikipedia , lookup
Common raven physiology wikipedia , lookup
Haemodynamic response wikipedia , lookup
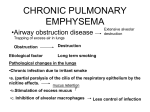
BHS 116 – Physiology Notetaker: Vivien Yip Date: 10/19/2012, 1st hour Page1 Final Exam Review 65-70Qs Lect 26-34 will be bulk of exam (60%) Not tested on reading assignments Remaining will be old Eliminate Lectures 1,2,3, 12 Dr. Donati will be around all week except Monday, all of next week and the Monday and Tuesday before final to answer any questions Pressure changes during ventilation Alveolar surface tension - Surfactant, breaks up surface tension - Normalizes collapsing pressure of larger and smaller alveoli - Smaller alveoli would collapse otherwise Alveolar ventilation - Pulmonary ventilation - All the air that goes into respiratory system - Alveolar ventilation - Only air that gets into alveoli, can physically exchange w/ blood - Always less than pulmonary ventilation (dead space) Factors affecting the rate of gas diffusion through the respiratory membrane Ventilation perfusion ratio - Ventilation is air taken into alveoli - Perfusion is blood to alveoli - Can be altered - Top of lungs have greater ventilation than perfusion, air goes into upper portions more so than lower portion o Have a lot of dead space, not getting full exchange w/ blood - Bottom of lung has greater perfusion than ventilation o Lower ventilation perfusion ratio (shunt) o More blood flow but does not get fully oxygenated - Airway obstruction that blocks air way leads to shunt situation, decrease ratio - Vascular obstruction leads to increase ratio, leads to dead space situation Local controls of ventilation perfusion ratio - Mechanisms to compensate for dead space/shunt situations - Vascular or broncho dilation/constriction to normalize ratio Gas transport in blood - Oxygen is much less soluble than CO2 - Only going to be 1.5% of O2 that is physically dissolved in blood, vast majority is carried by hemoglobin - CO2 is more soluble, 10% is physically dissolved, majority is in the form of bicarbonate in blood - PO2 or PCO2, refer to amounts that are physically dissolved and contributes to partial pressure - Amount bound to hemoglobin does not contribute to partial pressure Oxygen hemoglobin dissociation curve - Arterial blood 98% saturated - Venous blood 75% saturated - Tissues have higher CO2 levels - Under normal circumstance, we only give up 23% of oxygen - PO2 below 40, highly metabolic, exercise, really using up O2, see a very steep drop in dissociation curve BHS 116 – Physiology Notetaker: Vivien Yip Date: 10/19/2012, 1st hour Page2 - Hb gives up O2 more freely if below 40mmHg O2 and Hb dissociation curve shifts - Bohr Effect - Inc PCO2 and/or dec pH, dec O2 binding to Hb Right shift - Dec PCO2 and/or inc pH, inc O2 binding to Hb Left shift Haldane Effect - Dec O2 binding to Hb - Inc CO2 and H+ binding to Hb (@ tissue capillaries) Temperature and 123 Bisphosphoglycerate also contributes to Hb and O2 binding o Inc temperature and/or bisphosphoglycerate causes inc release of O2 and Hb Know how O2 and CO2 are transported in the blood Dorsal respiratory group of neurons - Primary regulator of ventilation - During normal breathing, consists primarily of inspiratory neurons which are either on/off, stimulating phrenic nerve, stimulates diaphragm, contraction (inspiration), relaxation (expiration) Ventral group comes in only during active expiration, during exercise or when we need to forcefully expire, has both expiratory and inspiratory neurons - Pneumotaxic center switches off inspiratory neurons from dorsal route, help regulate duration of inspiration - Apneustic center acts to inhibit the pneumotaxic neurons, maintain a constant inspiration, continue or exaggerate inspiration o Both act in concert, apneustic center mostly take over - Pacemaker maintains ventilation rate Peripheral chemoreceptor System - Carotid bodies and aortic bodies - Important for detection of changes in arterial blood PO2 - Also respond weakly to increased PCO2 + H+ O2 peripheral chemoreceptor effect - Highly sensitive group of receptors, only when O2 levels go below 60, do the chemoreceptors kick in - Stimulate medullary respiratory center, inc ventilation, bring in more O2 - Don’t respond to decreased HBO2 levels like anemia + CO - PO2 is only the amount physically dissolved in blood Central chemoreceptors - Found directly in brain, medulla - Inc in PCO2 leads to increased ventilation, decrease in PCO2 leads to opposite effect - More sensitive to PCO2 than PO2 (more potent regulator of ventilation) - Signal to medullary respiratory center to either increase or decrease ventilation and bring arterial PCO2 levels back to normal Bicarbonate Buffering System - 1st line of defense against changes in blood pH - Decreased blood pH drives reaction to the left - Excess co2 is expired by lungs - Increased blood pH drives the reaction to the right - Excess HCO3- is excreted in urine - Know the equation - CO2 + H20 <--> H2CO3 <-> H+ + HCO3Alveolar ventilation effects on pH - Increased ventilation, lower PCO2, lower H2CO3 levels, lower H+ levels, higher pH - Decreased ventilation, higher PCO2, higher H2CO3, higher H+ levels, lower pH pH effects on alveolar ventilation BHS 116 – Physiology Notetaker: Vivien Yip Date: 10/19/2012, 1st hour Page3 - Inc pH leads to dec ventilation - Dec pH leads to inc ventilation Effects of hydrostatic pressure gradients on pulmonary circulation - Zone 1: pulmonary capillaries are never open o Pathological conditions - Upper lung o Zone 2: systolic pressure, alveoli are open, diastolic pressure, alveolar pressure is greater, collapse o No blood flow through lungs during diastole, only seen in upper portions of lung - Most of lung o Zone 3: most common regions of lung o Open during diastole and systole o Capillary pressure is greater than alveolar pressure, vessels are open all the time Pulmonary pathologies COPD - Chronic bronchitis (disease of bronchi), asthma (disease of bronchi), emphysema (disease of alveoli) - More difficulty w/ expiration than w/ inspiration - Inc RV, Emphysema - Centriacinar, due to heavy smoking, quite common, Respiratory bronchioles, only area affected - Panacinar, affect entire alveolar tree, respiratory bronchioles and distal alveoli are affected, due to genetic deficiency, associated with alpha 1 antitrypsin, protease takes over and walls of alveoli are broken down Forced expiratory vital - FEV1/FVC - Normal is 80% - Forceful expiration test Pathogenesis - Imbalance with protease and anti protease - Cigarettes draws in macrophages, release proteases - ROS break down normal anti proteases - Proteases are more prominent than anti proteases - Break down of elastic tissue in alveoli, drastically reduce recoil of alveoli, which contributes to dec in expiration, not pushing as much air out Asthama - Extrinsic o Allergic response, increase IgE o Opening of mucosal tight junctions, edema and increased mucus secretion o Bronchoconstriction, due to chemical released from mast cells, stimulate vagal receptor - Intrinsic o Not allergic response o Virus provoked o Still end up with same primary affects: bronchoconstriction, edema, increase mucous production o No IgE - Global changes in bronchi: o See same things in both forms o Inc in thickness of basement membrane o Lamina propria thickens o Edema helps with thickening BHS 116 – Physiology Notetaker: Vivien Yip Date: 10/19/2012, 1st hour Page4 o Inc smooth muscle cells o Inc mucous gland production o Inc lymphocytes that are drawn to the area o Eosinophils in mucus Chronic bronchitis - No eosinophils - Earliest feature of bronchitis is hypersecretion of mucous in large airways (trachea and bronchi) due to hypertrophy of mucous glands - Irritant eventually leads to inflammation and narrowing of bronchioles causing fibrosis (irreversible damage) Chronic restrive lung diseases - Reduced compliance leading to problems with inspiration - Different types: idiopathic pulmonary fibrosis, hypersensitivity pneumonitis, diffuse alveolar hemorrhage syndromes - Decrease TLC, normal RV, decrease VC - FEV1/FVC is normal, everything is reduced proportionally, ratio is normal IPF idiopathic pulmonary fibrosis - Initial injury to alveolar wall that results in interstitial edema and accumulation of inflammatory cells (alveolitis) - Persistent injury results in the proliferation of macrophages, neutrophils, and alveolar…. - Main trigger: activation of macrophages - Recruit neutrophils and fibroblasts - Neutrophils release proteases and oxidants, injure type I pneumocytes epithelium - Activate hypertrophy in type II pneumocytes, also release fibrogenic compounds that draw in fibroblasts - Lay down extra ECM and fibrin Hypersensitivity pneumonitis - Immune response - Aka allergic alveolitis - Unlike bronchial asthma, the damage occurs primarily at the level of the alveoli Diffuse alveolar hemorrhage syndromes - Attack pulmonary basement membrane caused by type II hypersensitivity reaction - RBCs enter alveoli - Cough up blood, can become anemic - Hemoptysis, and diffuse pulmonary infiltrates are other symptoms - Reduce ability of lungs to fully expand, limit stretchability due to fibrotic deposits, restricting inspiration Thromboembolism, hemorrhage, and infarction - 2 important consequences of embolic arterial occlusion o Inc in pulmonary arterial pressure, pulmonary hypertension due to blockage of flow, can get necrosis of lung tissue o Ischemia of the downstream lung tissue, occlusion of larger vessels has a greater chance of resulting in death Pulmonary hypertension – Secondary, more common - Result of COPD - Recurrent pulmonary thromboemboli - Heart disease with a left to right shunt - L side of heart has higher pressure, blood shifts left to right side, increased volume in right side, makes r ventricle work harder Primary pulmonary hypertension - Genetic defect in BMPR2 BHS 116 – Physiology Notetaker: Vivien Yip Date: 10/19/2012, 1st hour Page5 - Normal protein: act to inhibit proliferation of vascular smooth muscle - Results in thickening of smooth muscle layer and constricts the vessel lumen Primary TB - Caused by mycobacterium TB - Initial phase, primary TB, bacteria is inhaled and taken up by alveolar macrophage o Proliferates in macrophage o Macrophage burst and release more bacteria o T cells are activated by macrophages o T cells recruit other cells to region (certain monocytes and epitheloid cells) to surround infected cells in the region, forming a granuloma o Prevent spread of bacteria o T cells are activated, hypersensitive phase, asymptomatic at this point because infection is walled off o Only when we get reinfected w/ the bacteria or something causes breaching of granuloma do we get secondary TB o Can also get latent lesions that lasts for decades o Major assault by immune system attacking bacteria and macrophages, a lot of collateral damage o Large regions of lung tissue are destroyed o Blood borne bacteria (military TB gets to blood stream and targets liver and spleen) o Primary (direct) and secondary (via military) ocular TB Pneumonia - Any type of infection to lung - Bronchopneumonia, parts of alveoli are affected - Lobar pneumonia, entire lobe is infected - Alveoli fill w/ fluid, RBCs, and leukocytes (mostly neutrophils) - Results in decrease in respiratory membrane arerea - Decrease in ventilation of alveolar space 4 stages of pneumonia - Healthy person can get through all 4 stages - Immune deficient individuals cannot o Congestion o Red hepatization o Gray hepatization o Resolution - Usually no permanent damage from pneumonia Genetic Diseases - Hereditary = familial - Congenital = present at birth - Autosomal dominant disorders o Only need 1 mutant copy to express disease, symptomatic o Know how those are passed on o Heterozygous Marfan’s syndrome - Fibrillin 1 is missing - Manifests in Skeleton, cardiovascular system, and the eyes - Fibrillin plays role in Ct of large arteries, get disruption - Aneurysmal dilations of aorta and other large arteries Familial hypercholesterolemia BHS 116 – Physiology Notetaker: Vivien Yip - Date: 10/19/2012, 1st hour Page6 LDL receptor mutations, loss of feedback and control, elevated levels of plasma cholesterol, premature atherosclerosis, inc risk of MI Autosomal recessive disorders - Need 2 copies of mutant gene to have disorder - 1 copy, asymptomatic carrier - Frequently involved w/ enzyme gene expression Glycogen storage diseases (glycogenoses) - Deficiency in any one of the enzymes involved in glycogen synthesis - Hepatic form: type I o Glycogen builds up, enlargement of liver, fail to make glucose, hypoglycemia - Myopathic forms: type V o Muscle weakness o V little lactic acid produced during exercise Cystic fibrosis - Affect epithelial cells in exocrine gland - Affects respiratory GI and reproductive system - Sweat test v important in diagnosis, higher NaCl content, the more severe the cystic fibrosis - Mutation in CFTR gene - Function of CFTR are tissue specific, impact will also be tissue specific X linked recessive disorders - Males only have 1 X chromosome, they will have the disease o Will not pass onto their sons - Females will be asymptomatic carriers with the affected X chromosome - Sons of heterozygous mothers have a 50/50 chance of getting the disease Hemophelia A - Mutation in factor VIII, coagulation factor - Higher susceptibility to bleeding - Need to knock out more than 99% of factor VIII to get effect Fragile X syndrome - Mutation in familial mental retardation FMR1 gene - Trinucleotide repeat - Loss of FMR P protein, get defective neuronal development - Not true mendelian disorder - Carrier males can be asymptomatic, premutation - Can pass onto their daughters - Daughters will then during oogenesis will add more trinucleotides where it becomes a full blown mutation to their sons (50% chance) Normal karyotype - Polyploidy o Incompatible with life - Aneuploidy o Can be compatible with life, trisomy 21, error in meiosis called nondisjunction Mutations - Point mutations - Misssense and nonsense - Frameshift - Trinucleotide repeat - Chromosome structural abnormalities - Translocations…