* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download HIV Infection in Children and Adolescents
Rocky Mountain spotted fever wikipedia , lookup
Cryptosporidiosis wikipedia , lookup
Tuberculosis wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Meningococcal disease wikipedia , lookup
Trichinosis wikipedia , lookup
Hepatitis C wikipedia , lookup
Sarcocystis wikipedia , lookup
West Nile fever wikipedia , lookup
Chagas disease wikipedia , lookup
Onchocerciasis wikipedia , lookup
Epidemiology of HIV/AIDS wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Microbicides for sexually transmitted diseases wikipedia , lookup
Marburg virus disease wikipedia , lookup
Neonatal infection wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Leptospirosis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Hepatitis B wikipedia , lookup
Diagnosis of HIV/AIDS wikipedia , lookup
Schistosomiasis wikipedia , lookup
Infectious mononucleosis wikipedia , lookup
Lymphocytic choriomeningitis wikipedia , lookup
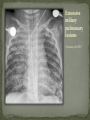
Infectious Disease Part 1 I’m going to Jazz Fest this weekend! A. True B. False Epidemiology, diagnosis, prevention and treatment of HIV/AIDS has changed dramatically over the past 25 years Rates of new infections in infants has plummeted Effective screening and prevention strategies Children born with HIV are surviving into young adulthood Adolescents acquiring HIV at an alarming rate Worldwide: 33.2 million people living with HIV 2.5 million are children younger than 15 In 2007, 2.1 million AIDS deaths occurred 330,000 were children In the US: In 2006, 2181 cases of AIDS were reported among children and adolescents through age 24 Only 38 cases were in children <13yo Pediatric burden of infection now rests in the adolescent population! Lentivirus in the retrovirus Family Infection occurs when the virus enters the body and binds to the CD4 receptors on host T lymphocytes Binding fusion of HIV envelope with lymphocyte cell membrane viral RNA and enzymes (RT) enter host cell viral RNA reverse transcribed into DNA viral DNA enters host cell nucleus integration into host cell genome activation of host cell virion production and release spread to other cells This viremic phase preceeds antibody response and is the period of HIGHESET INFECTIVITY!! A 17 yo honor student comes to your office with a maculopapular rash on his face, trunk, palms, and soles. He also c/o a sore throat and fever. He states that he has been sexually active with women for 2 years and men for 6 months. He does not use condoms with either. He denies any sick contacts or substance abuse, including injection drug use. You are strongly considering early HIV infection in this patient. The most accurate test to confirm the diagnosis at this time would be: A. Western Blot B. EIA C. HIV RNA PCR D. Rapid test- blood E. Rapid test- saliva Viremic phase corresponds with the acute retroviral syndrome: Fever, LAD, rash, myalgias/ arthralgias, HA, diarrhea, oral ulcers, leukopenia/ thrombocytopenia, transaminitis During this “window period” between host cell infection and antibody response: HIV antibody test negative HIV RNA positive Seroconversion occurs b/t 10-14 days and 6 months after infection All of the following are effective ways to decrease the risk of transmission of the HIV virus from mother to child EXCEPT: A. C/S before the onset of labor in persistently viremic women B. ART during pregnancy C. Neonatal AZT D. Intrapartum AZT E. Breastfeeding the infant *Transmission by two principal modes *Mother-to-child Antepartum: transplacental transfer Intrapartum: exposure to maternal blood, amniotic fluid or cervicovaginal secretions during delivery Postpartum: Breastfeeding Behavioral Unprotected sex Traumatic sex Active genital ulcer disease Douching before sex Injection drug use So what do we do?! *Mother-to-child ART Intrapartum zidovudine Neonatal zidovudine Safe replacement feeding Elective C/S before the onset of labor in women with persistent viremia Behavioral *COUNSEL, COUNSEL, COUNSEL!! Abstinence Consistent and correct use of condoms A 20 mo F presents to your clinic, because her mother was recently diagnosed with HIV. Mom did not receive PNC during her pregnancy and is unsure if any HIV testing was performed at delivery. She is very concerned and would like the child tested. Of the following, the most appropriate test to order (on the child) would be: A. HIV DNA PCR B. HIV RNA PCR C. HIV antibody titer D. No testing is required in this patient *Remember that all infants Born to HIV-positive mothers Will test positive for the HIV Antibody due to maternal Transfer of Ig A 4 mo M presents to your office for a WCC. Past medical history includes HIV exposure in utero. Mom was treated with ART through the pregnancy and AZT at delivery. The child also received AZT and is formula fed. At his 2 week visit and 2 month visits, HIV DNA PCRs obtained were negative. Of the following, you are most likely to counsel Mom that: A. HIV is definitively excluded in her son B. An HIV antibody titer should be performed at this visit and if negative, HIV is definitively excluded C. An HIV DNA PCR should be performed at this visit and if negative, HIV is definitively excluded D. An HIV antibody titer should be performed at 18 mos to definitively exclude HIV E. Even though the past 2 tests have been negative, there is still a high likelihood her son is infected with HIV HIV-exposed infants HIV DNA/RNA PCR at 2 weeks, 2 months, and 4 months Definitive exclusion of infection Negative results for two virologic tests First at age 1 month or older Second at 4 months of age or older Confirmatory antibody test at 12-18 mos optional HIV-positive mothers and BF Testing should continue throughout period of BF and 6 months after Children and adolescents All children of HIV-positive mothers should be screened Adolescents should be screened as a part of routine health care Age 13 and older High-risk adolescents should be screened yearly! First step: referral to an HIV specialist! Antiretroviral therapy Goals: (maximize quality and longevity of life) Complete suppression of viral replication Preservation or restoration of immunologic function Prevention of or improvement in clinical disease Antiretrovirals What to start? ART should be planned and monitored in collaboration with an HIV specialist Triple-drug combination ART 3 drugs from 2 categories: one non-nucleoside reverse transcriptase inhibitor (NNRTI) OR protease inhibitor PLUS two nucleoside or nucleotide reverse transcriptase inhibitors Viral load to monitor adherence Non-detectable viral load within 3-6 months Failure to achieve this goal strongly suggests suboptimal adherence rather than resistance Prevention of Opportunistic Infections Pneumocystis jiroveci pneumonia (PCP) Most common OI Bactrim prophylaxis for: All HIV-exposed infants until infection is reasonably excluded All HIV-infected infants <12mos All HIV-infected children and adolescents with severe immune suppression CD4 percentage< 15% or CD4 count< 200 cells/mm3 Mycobacterium avium complex Azithromycin prophylaxis for: Age≥ 6yo with CD4 count <50 cells/mm3 Ages 2-5yo with CD4 count <75 cells/mm3 Ages 1-2 yo with CD4 count <500 cells/mm3 Age< 1yo with CD4 count <750 cells/mm3 Prevention of opportunistic infections Toxoplasmosis Less common in children Bactrim prophylaxis in: Toxoplasma IgG positive individuals with severe immunosuppression (CD4%< 15% or CD4 count < 100 cells/mm3) Immunization schedule same as for healthy children with a few small exceptions: CD4 percentage< 15% or CD4 count< 200 cells/mm3= NO VARICELLA OR MMR Only killed, injectible formulations of the influenza vaccine Coping with the diagnosis and prognosis Offer hope and reassurance about the availability of effective treatment *Disclosure of HIV Infection status Planned disclosure to family and friends can increase support for the HIV-positive person Sexual partners can make informed decisions about how to protect themselves Adherence to Care and Treatment Requires 90-100% adherence to drug regimens to avoid the development of resistance School and sports participation HIV-infected children and adolescents can participate fully in the educational and extracurricular activities at school *No obligation to notify school personnel of student’s HIV infection status Some experts advise athletes with a detectable viral load to avoid high-contact sports (boxing, wrestling) Transition to adult health care Complete and coherent medical record Advance care planning and palliative care Which of the following statements regarding EBV epidemiology is TRUE? A. Immunocompetent persons who have been infected shed more virus than immunosuppressed persons B. Infectious mononucleosis caused by EBV occurs most commonly in infants and toddlers C. Most people who become infected with EBV are symptomatic for life D. The risk of transmission is highest from persons who have had recent infections E. The virus is only transmitted through oral secretions EBV results in spectrum of diseases Infectious Mononucleosis Aggressive non-malignant proliferations Hemophagocytic syndrome Post-transplant lymphoproliferative syndrome (PTLS) Lymphoid interstitial pneumonitis Oral hairy leukoplakia Human malignancies Nasopharyngeal carcinoma Burkitt lymphoma Hodgkin disease Leiomyosarcoma *Host immune response plays a key role in determining clinical manifestations *Know the epidemiology of EBV *Mode of transmission: oral contact with saliva Handling of toys Kissing among adolescents Also found in genital secretions *Incubation period: 30 to 50 days Onset of illness is insidious over 1 to 2 weeks *Period of communicability Shed at high concentration for 6 months following acute infection, and then low concentration for life Herpesvirus Type 1 and Type 2 Infection of B cells in the lymphoid-rich areas of the oropharynx Dissemination throughout the lymphoreticular system including the liver and spleen Like all herpesviruses, EBV establishes persistent latent infection for the life of the host Memory B-cells Reactivation is asymptomatic (second attacks have not been documented) *Classic infectious mononucleosis Fever Pharyngitis Adenopathy (90%) Peaks in 1st week Fatigue Headache Nausea, vomiting, and anorexia are frequent Reflect hepatitis A 15-year-old male comes to the ER because he has had a sore throat and fever for the past week. On physical exam he has cervical lymphadenopathy, his spleen edge is palable 3cm below the costal margin, and he has a generalized maculopapular rash with several scratch marks. Upon further questioning, he tells you that his PCP gave him some antibiotics a few days ago but he can’t remember the name. The MOST likely medication to cause the patient’s new symptom is: A. Amoxicillin B. Cefdinir C. Ampicillin D. Bactrim E. Ciprofloxacin Splenomegaly in 50 to 60% Can cause upper quadrant discomfort 2 to 3 cm below the costal margin *Know the significance of rash following ampicillin in patients with mono 3 to 15% of all patients Maculopapular Following administration of ampicillin or amoxicillin in 70 to 90% Immune mediated Discontinue antibiotic Gianotti-Crosti syndrome Papular acrodermatitis on cheeks, extremities, and buttocks Can last for 15 to 50 days *Know the range of clinical manifestations of EBV infection in children of various ages Infection in young children is usually asymptomatic Or produces symptoms indistinguishable from other febrile infections Infectious mononucleosis is rarely recognizable in children under 4 Among adolescents the clinical syndrome is classic Infectious mononucleosis is rare in adults older than 30 to 40, when most people are already infected with EBV Heme Total WBC 12,000 to 18,000 Lymphocytosis (>60%) Atypical lymphocytes (20-40%) Thrombocytopenia (usually self-limited) Liver function tests Elevated aminotransferases in 50% of patients Asymptomatic without jaundice You are evaluating a 3-year-old girl who has fever for 10 days, pharyngitis, and cervical lymphadenopathy. You suspect she has an infection caused by EBV. Which of the following tests is MOST likely to confirm your diagnosis? A. CBC B. Heterophile antibody C. IgM early antigen test D. IgM viral capsid antigen test E. Viral culture Heterophile antibodies Monospot is a latex agglutination assay using horse erythrocytes Stays positive for 2 years after infection Detects antibody in 90% of cases Does not have same specificity and sensitivity in young children They do not produce antibodies 80% by age 4 Diagnostic choice If + monospot and compatible syndrome, no further testing If EBV infection still suspected, test for specific antibodies *Distinguish (by serologic tests) between acute and past EBV infections EBV-specific antibodies Viral capsid antigen (VCA) IgM and IgG are present at onset IgM wanes over 3 months Confirms the diagnosis of acute EBV infection IgG persists for life Nuclear antigen (EBNA) IgG to EBNA begins to appear 6 to 12 weeks after onset of symptoms Early antigen IgG to EA present at onset of illness You are seeing a long-time patient of yours who is a 16 year- old male with sore throat, fever, and fatigue for the past week. He is a varsity football player, but has felt too tired to practice this week. On physical exam he has mild hepatosplenomegaly. You do a Monospot in the office and it is positive. Of the following, the BEST way to manage this patient is: A. Start a course of corticosteroids B. Supportive care and advise him to avoid contact sports for 3 to 4 weeks and until his splenomegaly has resolved C. Supportive care and advise him to avoid contact sports for 6 months D. Supportive care and he can return to practice immediately E. A 7 day course of Acycolvir *Plan the management of a patient with uncomplicated infectious mononucleosis Observation and symptomatic treatment Acetaminophen, NSAIDS, bed rest Return to sports Want to avoid splenic rupture Most likely to occur within 2 to 21 days after onset of symptoms Avoid sports in initial 2 to 3 weeks or while splenomegaly is present All of the following are indications for corticosteroid use in the treatment of EBV infection EXCEPT: A. Seizures B. Worsening fatigue C. Upper airway obstruction D. Hemolytic anemia E. Thrombocytopenia with bleeding *Know the indications for the use of corticosteroids in treatment of infectious mononucleosis Upper airway obstruction Thrombocytopenia complicated by bleeding Autoimmune hemolytic anemia Seizures Meningitis Prednisone 1 mg/kg/day x 7 days then taper x 7 days Should not be used on routine basis due to unknown hazards of immunosuppression for a virus that has oncogenic complications Uncommon in healthy persons Splenic rupture (<0.5% in adults) Tonsillar swelling that causes airway obstruction Drooling, stridor, difficulty breathing Indication for hospitalization IV hydration, humidified air, steroids Headache (50%) Seizures and ataxia (1 to 5%) Meningitis, facial nerve palsy, transverse myelitis, GBS “Alice-in-Wonderland synrome” (metamorphopsia) Hemolytic anemia Aplastic anemia Myocarditis Interstitial pneumonia Pancreatitis Parotitis Orchitis HLH *Understand that host factors are important in the outcome of EBV infection Immune response is essential for controlling EBV replication during primary infection as well as latent infection Immunocompromised people are at increased risk for EBV-associated malignancies HIV, organ transplant anti-immune therapy, congenital immunodeficiencies Excellent with symptoms typically lasting 2 to 4 weeks Some have debilatating fatigue and malaise that can wax and wane for 6 months Second attacks are not documented One of your patients recently had a positive TST. He was subsequently sent for a CXR which was normal. He is otherwise well and has no known TB contacts or travel. By definition, this patient has: A. Active TB disease B. No TB disease C. Latent TB infection (LTBI) D. Had the BCG vaccine TB exposure: persons exposed to someone who has TB but whose status is not yet clear *Latent TB (LTBI): positive TST without symptoms, physical findings, or radiologic anomalies c/w TB *TB disease: positive TST with clinical or radiologic manifestations of TB disease Multidrug-resistant (MDR) TB: TB resistant to 2 first-line TB meds (INH and rifampin) One third of the global population has LTBI (!) Of all persons with untreated LTBI, 5-10% will ultimately develop TB disease 90% of the burden of TB disease is in the developing world In the US: 13,000 new cases of TB disease in 2007 820 children <15yo Control of TB in children has often been neglected b/c children are ineffective transmitters of the bacillus However, much of the morbidity and mortality occurs during childhood! *Specific groups with high LTBI and disease rates include: Immigrants International adoptees Travelers to countries with endemic infection Homeless Residents of corrections facilities Refugees from high prevalence regions Increased risk of progression to TB disease: HIV co-infection (and other immunocompromising conditions) Recent LTBI IV drug use Medical conditions DM Renal failure TB is transmitted by expulsion of nasal droplets from an infected human individual to an uninfected one. Nasal droplets, which contain tubercle bacilli and are no larger than 2 um in diameter, are able to penetrate to the alveoli of the respiratory tract of the uninfected individual. Includes intrathoracic LAD and parenchymal disease Most common site of TB infection Incubation period 4-12 mos Three time frames for pulmonary involvement with TB Primary parenchymal Progressive primary Reactivation disease One of the most common manifestations of disease Infants and adolescents more likely to be symptomatic than 5-10 yo children Become symptomatic when enlarging LN compress adjacent airways collapse consolidation pattern Radiographic features: hilar/mediastinal LAD Right –sided hilar LAD, narrowing of the right mainstem bronchus and collapse-consolidation of the RLL *Courtesy of UTD* Results from poor containment of the initial infection Young infant or immunocompromised host LN erosion into the airways aspiration of bacilli Development of adult-type cavitary disease in children >10yo Associated with lung tissue destruction and cavity formation Progressive Primary TB in a toddler Extensive hilar LAD with collapseconsolidation in the left lung and miliarylike presentation of the right lung *Courtesy of UTD* More common in adolescents, especially in areas that have high rates of co-infection with HIV Reactivation disease more common in the apices of lungs in adults (while primary disease occurs in the bases)- NOT SO FOR CHILDREN Radiographic findings in reactivation overlap considerably with the other two types of pulmonary disease Cavitary TB Infiltrate and cavity along R horizontal fissure. Absent hilar LAD c/w adult-type or reactivation TB in adolescents. *Courtesy of UTD* Symptom Infants Children Adolescents Fever Common Uncommon Common Night sweats Rare Rare Uncommon Cough Common Common Common Productive cough Rare Rare Common Hemoptysis Never Rare Rare Dyspnea Common Rare Rare Rales Common Uncommon Rare Wheezing Common Uncommon Uncommon Decreased BS Common Rare Uncommon Pulmonary Common Common Common Pulmonary+ Extrapulmonary Common Uncommon Uncommon Sign Location of disease Most common extrapulmonary form of TB Hematogenous spread Incubation period: 4-12 mos LN involvement: anterior cervical > posterior triangle > submandibular > supraclavicular Usually measure 2-4 cm and lack the classic inflammatory findings of a pyogenic node May be overlying violaceous skin discoloration Untreated lymph nodes: may caseate, spread to contiguous structures and lead to formation of a sinus tract Surgical node excision not curative but may be necessary to establish the diagnosis Rare Develops in fewer than 2% of all cases of TB 50% of all patients are younger than 2 years of age Incubation period: 2-6 mos (In parts of the developing world, TB is the primary cause of subacute meningitis and tuberculomas are common causes of mass occupying CNS lesions) Tuberculomas Conglomerate caseous foci within the brain that develop from deep seated tubercles acquired during recent or remote hematogenous bacillemia Single rim enhancing lesions ranging from 1-5cm. TB Meningitis When a subependymal tubercle progresses and ruptures into the subarachnoid space CSF : lymphocytes, low glucose, and high protein Highest morbidity and mortality rate Due to lymphohematogenous spread So, it can pretty much go ANYWHERE! Disease of the younger or immunocompromised child Clinical presentation highly variable Acute disease: may be fulminant including multiorgan system failure, septic shock, or ARDS Subacute or chronic disease: may present with FTT without fever, fever of unknown origin, or with dysfunction of one organ system Clinical manifestations Fever, constitutional symptoms HSM on exam CNS involvement in 20% A child with miliary TB should ALWAYS be evaluated for meningitis Extensive miliary pulmonary lesions *Courtesy of UTD* Skeletal disease Disease of the older child Spondylitis (Pott’s disease), arthritis, osteomyelitis Pleural disease Also a disease of the older child Can occur in isolation from or concomitantly with pulmonary disease Sx: CP, fever, dyspnea, cough, anorexia Congenital disease Occurs in infants born to mothers with endometrial or disseminated TB Abdominal disease Renal disease Cutaneous disease Who to screen? Screening tests TST IGRAs Confirmatory tests Sequential sputum sampling Early AM gastric aspirates Specimens from an extrapulmonary site CT scan TST Comprises antigens not all specific to M. tuberculosis Antigens trigger a delayed hypersensitivity reaction to persons who have come in contact with TB bacilli Becomes positive 3 weeks to 3 months after infection and should remain positive for life One of the nurses on the 5th floor asks you to read her TST that was placed ~60h ago. You appreciate an area of induration approximately 11 mm in diameter. What is the most appropriate next step for this nurse? A. INH for 9 mos B. CXR to screen for active TB disease C. Reassurance D. Repeat TST in 3 mos E. RIPE therapy for 6 mos You are doing a WCC on a 7 yo F who recently moved to the US from India. Since there were 2 positive responses on the TB risk factor-based questionnaire (+lived out of the US, +BCG vaccine), you place a TST. When the patient returns in 48h, the TST is positive with a 12 mm area of induration. The mother asks you what needs to be done next. You respond: A. Nothing, the TST was likely positive because she received the BCG vaccine B. Induced sputum for AFB gram stain and culture C. INH therapy D. CXR E. RIPE therapy False Positive Results False Negative Results Children exposed to Age<6mos nontuberculosis mycobacteria Recent administration of the BCG vaccine** Improper administration or interpretation of TST Disseminated forms of TB can induce anergy (miliary and meningitis) Recent measles infection High-dose corticosteroid treatment (or other forms of immunosuppression) Irradiation Measures patient’s ability to produce interferon gamma after their lymphocytes are stimulated by 2 or 3 antigens on M. tuberculosis Greater specificity than TST but similar sensitivity CXR Detailed contact and symptom history Physical Exam Latent or Active TB • 3 samples collected on different days before the child eats or ambulates • Induced vs. Expectorated vs. BAL • Pleural fluid, CSF, lymph node biopsy, etc… Sequential sputum sampling Gastric aspirates of early AM secretions Specimens from an extrapulmonary site CT scan • If CXR findings are equivocal *Healthcare worker: +TST (≥10mm) CXR CXR negative offer to treat for LTBI weighing risks and benefits CXR positive further evaluation and Rx Contact investigations *Child with an adult household contact with TB disease: TST and CXR for ALL children in the household Children <4yo (or immunocompromised) empiric INH The mother of a 2 mo breastfed infant comes to your clinic very concerned, because she recently had a positive TST. She reports that her doctor sent her for a CXR, which was normal, and then put her on a single medication. She asks you what needs to be done to keep her baby from contracting the illness? A. No intervention is required for the infant B. Cessation of breastfeeding C. Separation of mother and baby D. Empiric INH in the infant E. Multidrug therapy in Mom Infant whose mother has TB: Mom with +TST, -CXR (LTBI) no intervention for infant Mom with +TST, +CXR (TB disease) evaluation for congenital TB; separation from Mom until infant is receiving INH and Mom is on multidrug therapy Children who have TB should be seen monthly while receiving therapy Medication tolerance and adherence Weight gain Achieving appropriate milestones (esp with TB meningitis) Look for disease spread Pulmonary TB Repeat CXR after 1-2 months of therapy TB meningitis: Often require sequential CNS imaging by CT scan or MRI Appropriate chemoprophylaxis of children who have been exposed to TB or have LTBI BCG vaccination Should only be considered for children who are HIV negative, have a negative TST and who are continually exposed, and cannot be separated from, adults who: Are untreated or ineffectively treated for TB disease (if the child cannot be given long-term treatment for infection) Have TB caused by strains resistant to isoniazid and rifampin Infection control and contact investigation Hospital infection control Most younger children do not have a sufficiently forceful cough or high enough organism burden in the airways to be infectious EXCEPT FOR children with: Cavitary or extensive pulmonary involvement AFB smear-positive TB Laryngeal TB Procedures with high risk of aerosolization of bacteria (BAL, entubation) If any of the above criteria met personally fitted and sealed particulate respirators should be used by all patient contacts and patient should be placed in airborne infection isolation Infection control and contact investigation Hospital infection control (con’t) Major concern is household contacts that may be the source case Visitation should be limited to those who have had a CXR that excludes contagious TB Return to child care and school Children with TB disease can attend school or child care if: Effective therapy has been instituted Adherence to therapy has been documented Clinical Sx have diminshed substantially Children with LTBI can participate in all activities whether they are receiving treatment or not Children with a positive TST should be a “starting point for epidemiologic investigation by the local health department” Reporting of suspected and confirmed cases of TB is mandated by law in all states Physicians should assist local health department in the search for the source case and others infected by the source case New Orleans Health Department 504-658-2500 LTBI TB Disease TB meningitis • 100% effective in preventing TB disease • Adherence must be EXCELLENT! • 95-100% cure in drug-susceptible disease • Overall mortality low • Highest rates of mortality and long-term sequelae • 33% die and 50% have residual defecits Designed to prevent the spread of microorganisms among patients, health-care personnel, and visitors Standard precautions and “cough etiquette” should be used for all persons in and out of the health-care setting 3 components Source Patient, health-care worker, visitor Acutely ill with symptoms Colonized/infected but no symptoms Inanimate objects and toys Susceptible host Means of transmission Direct contact (infected person to host) Indirect contact (fomite) Droplet (large particles going < 3 feet) Airborne (small particles suspended in air and dispersed) *Know the recommendations for standard precautions All patients Hand hygiene before and after each patient contact Single most important practice to reduce transmission of microorganisms Alcohol-based preferred (superior activity and adherence) Soap and water if visible soil or with spore-forming organisms (C. diff) No artificial nails for workers in ICU, OR, or oncology) Assoc. with gram-neg bacillary and candidal infections Use of protective equipment when needed Respiratory Hygiene “Cough etiquette” For staff, patients, families (everyone!) Covering one’s mouth and nose during a cough or sneeze Dispose of tissues Follow with hand hygiene If no hand hygiene available → direct cough into antecubital fossa Those with respiratory illness who cannot be separated from others by 3 feet, should wear a mask You are on night float for Purple team and a 7 month old male comes in with rhinorrhea, cough, and increased work of breathing. The viral panel comes back positive for RSV. Which of the following will you include in your order set? A. Droplet precautions B. No precautions necessary C. Airborne precautions D. Standard precautions E. Contact precautions *Know the recommendations for contact precautions Gloves and gown when direct patient contact Patients in single rooms or cohorted *Identify when contact precautions are required Organisms C. diff Enteroviruses RSV Multidrug-resistant organisms Draining abscesses, cellulitis, decubitus ulcers Supplies should be available outside the patient rooms A few hours later, you are admitting a 4-year-old male for Silver team who is a know asthmatic with symptoms of cough, fatigue, and increased work of breathing. His viral panel comes back positive for influenza. Being the stellar resident that you are, you order droplet precautions prior to sending this patient to the floor. Which of the following BEST describes droplet precautions? A. Single room and surgical mask required B. Shared room and no personal protective equipment required C. Single room and gown and gloves required D. Cohort room and good hand hygeine E. Negative pressure room and surgical mask required *Know the recommendations for droplet precautions A surgical mask is required Single room or cohort (with 3 feet and curtain) for patients When patients leave the room → mask, cough etiquette *Identify when droplet precautions are required Influenza Rhinovirus Bordetella pertussis Neisseria meningitidis Strep pyogenes Keep precautions in place until pt. has been receiving antimicrobial therapy long enough to prevent transmission *Know the recommendations for airborne precautions Negative pressure airborne infection isolation room Before entering the room, clinicians should use a fit- tested N95 or similar sealing mask *Identify when airborne precautions are required TB Measles Varicella *Understand that office and hospital staff should receive an annual influenza immunization Have a great weekend!