* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download shigella -study material-2012
Triclocarban wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Marine microorganism wikipedia , lookup
Molecular mimicry wikipedia , lookup
Bacterial cell structure wikipedia , lookup
Gastroenteritis wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Human microbiota wikipedia , lookup
Schistosomiasis wikipedia , lookup
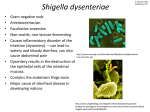
SHIGELLA 1 Shigella The organisms of genus Shigella differ from other. Enterobacteriaceae in that they are exclusively parasites of human intestine and other primates and cause bacillary dysentery in man characterized by the passage of loose motion mixed with blood and mucous. The dysentery bacilli belong to the genus Shigella, named after Shiga who isolated the first member of the group in 1896 from epidemic dysentery in Japan which was then called Shigelia shiga. Morphology The organisms are Gram-negative, aerobic, non- motile, non-flagellate and noncapsulated bacilli, measuring 1-3 x 0.5 μm. Culture The organisms grow in ordinary medium like nutrient agar, in which the colonies are about 2 mm in diameter, circular, convex, smooth and translucent. For their isolation from faeces, MacConkey’s agar or Deoxycholate citrate agar (DCA) media are used. In DCA and MacConkey’s agar the colonies are colorless except Shigella. sonnei which is a late lactose fermenter. In Shigella-Salmonella agar (S. S. agar) the colonies are colorless. Viability The thermal death point for Shigelia is 55°C for one hour. They are killed by 1% phenol in 30 minutes. They remain viable in water and ice for 1-6 months. Antigenic structure Shigellae are differentiated on the basis of their polysaccharide component of lipopolysaccharide complex of the somatic 0-antigens into four groups A, B, C and D. Some strains produce K antigens which are usually of B variety and cover the 0-antigen. The K-antigen may or may not be visible as capsule. Classification Antigenically, shigellae are divided into four groups (A, B, C & D) on the basis of serological specificity of polysaccharide component of the somatic 0-antigen. These main groups or species of Shigella are better differentiated by a combination of their biochemical reactions and antigenic structure. Mannitol fermentation reactions are important which distinguish Group A strains (mannitol-negative) from Groups B, C and D (mannitol-positive). SHIGELLA 2 Biochemical Reaction SHIGELLA 3 Antigenic structure Based on 0 antigens shigellae are differentiated into serotypes, identified by agglutination absorbed antisera. The antigenic structure of the shigellae is complex. Subgroup A (Sh. dysenteriae) Sh.. dysenteriae is subdivided into 12 serotypes, of which serotype 1 is known as Shiga’s bacillus and serotype 2 as Schmidtz’s bacillus. Subgroup B (S/i. flexneri) The members of the group have complex structures There are six main serotypes (1-6) of S/i. flexneri, each characterized by different specific antigen, each of which is further subdivided into sub serotypes (e.g. la and lb). Subgroup C (S/i. boydii) Eighteen serotypes of Sh. boydii are recognized. Except serotypes 10 and 11, all are antigenically distinct. Subgroup D (Sh. sonnei) Sh. sonnei strains are antigenically homogeneous but they may undergo an antigenic variation that affects the somatic antigens and has been referred to as phase or form variation. Toxin 1. Endotoxin: All shigellae release endotoxin after autolysis. It is the polysaccharide lipoprotein complex of cellwall. Endotoxin shows irritating action on the intestinal wall which causes diarrhoea and subsequent intestinal SHIGELLA 4 ulcers. 2. Exotoxin : Sh. shiga (Sh. dysenteriae type I) in addition to endotoxin, produces a powerful exotoxin in very small amount in intestine. The exotoxin is a heat labile protein and acts as (a) enterotoxin as well as (b) neurotoxin. As enterotoxin, it acts upon intestinal mucosa causing transudation of fluid in the lumen and as neurotoxin it damages endothelial cells of small blood vessels of the central nervous system which results in neurological complications like polyneuritis, coma and. meningism. The exotoxin is not primarily a neurotoxin. Strains of Sh. dysenteriae 1 produce a cytotoxic which is active on Vero cells and is called verocytotoxin or VT. VT also acts upon human colon and ileal cells in tissue culture. Pathogenesis The term dysentery is loosely used to mean diarrhoea with passage of pus, blood and or mucous in the stool accompanied by abdominal cramps and tenesmus. The severity of the illness in bacillary dysentery depends on the infecting species of Shigella. Sh. shiga (Sh. dysenteriae type I) causes most severe and fulminating form of dysentery usually associated with toxaemia. The infections due to Sh. flexneri and Sh. boydii are less severe and prevalent in tropical and sub-tropical countries including India. The Sonnei infection is more frequently seen in children. The incubation period of the disease is usually less than 48 hours but varies between 1 to 7 days and infection occurs by ingestion of contaminated food. The food or drink is contaminated by faeces of infective cases or that of carriers through contaminated objects in their environment and also through flies. Shigellae are pathogenic in much smaller dose than the salmonellae and as few as 10 to 100 bacteria can cause dysentery. The organisms, after reaching the terminal ileum and colon, first attach themselves to the surface of epithelial cells and gradually they are taken by the epithelial cells where they multiply. The distal parts of the colon are more severely affected. Then they spread laterally into adjacent cells as well as to the lamina propria where replication and bacterial colonization take place. There is necrosis of surface epithelial cells. The lamina propria and submucosa develop an acute inflammatory reaction with formation of micro-abscesses on mucosal surface predominantly by polymorphonuclear leucocytes, along with capillary thrombosis. The necrotic epithelia become soft and friable and are sloughed out in patches forming superficial snailtractor serpiginous ulcers which lead to bleeding from mucosa. Endotoxin irritates the bowel causing diarrhoea. The ulcer surface is then covered by a pseudo membrane made up of fibrin, leucocytes, cell debris, necrosed epithelia and bacteria. The intestinal ulceration is due to the activity of the bacterial endotoxin. With remission, granulation tissue fills the defect and the ulcers heal by regeneration of the mucosal epithelium. The organisms tend to remain localized in the gut-wall and usually do not cause bacteraemia. In addition to endotoxin, Sh. shiga produces a potent exotoxin which causes toxaemia. The toxin causes transudation of fluid from intestinal mucosa leading to severe diarrhoea (enterotoxic action) and by toxaemia damages the vascular endothelium causing neurological complication like polyneuritis and myocarditis or joint effusions. The colonic ulcers are small, superficial with shallow depth and the intervening mucosa is oedematous. They are multiple and are covered by pseudomembrane. In fulminating infection due to Sh. dysenteriae type I, the entire mucous membrane of large gut may be affected and may slough out causing death. Fortunately milder forms of disease due to Sh. flexneri or sonnei is common. Dysentery carriers Healthy carriers may be found in some community. Carrier state is acquired after recovery from acute attack of dysentery. Laboratory diagnosis Specimens (a) For microscopy and culture, fresh stool, mucous flakes, rectal swabs are collected under aseptic SHIGELLA 5 precaution, (b) blood, serum may be examined for demonstration of rising titre of agglutinin antibodies. A. Microscopical examination of stool Coverslip preparation in saline and iodine shows large number of pus cells with degenerated nuclei. R.B.C. and macrophages. The presence of protozoa, cysts or helminthic ova is excluded. The normal bacterial flora is considerably diminished. Fluorescent antibody technique is of some help in rapid diagnosis of a case but is not usually practiced B. Bacteriological examination I. Culture Media :a) MacConkey’s agar ,b) DCA , c) S-S agar, d) Selenite F broth A loopful of material is inoculated on selective media like MacConkey’s agar or S. S. agar media. Selenite-F broth (0.4%) is used as enrichment and transport medium which permits rapid growth of enteric pathogens. Organisms from selenite-F broth are sub cultured in MacConkey’s agar after 24 hours incubation at 37°C. Colorless colonies appear on MacConkey’s agar medium after 12 to 18 hours incubation which are further tested by smear examination, motility preparation and biochemical reactions. Shigellae are Gram-negative nonmotile bacilli. Biochemical reactions Urease, Citrate, H2S and KCN negative; indole and M R positive organism is suggestive of a shigella strain. Sh. sonnei is a late lactose fermenter. Slide agglutination test It is done by using polyvalent antisera of three groups (A, B and C) of shigella and antiserum of group D (Sh. sonnei), one by one against the isolate. Monovalent antisera are used for the group for which agglutination has occurred with polyvalent antisera. Then type specific antisera for strains belonging to group A, B or C is used for agglutination test. Occasionally, agglutination may not occur due to masking of 0 antigens by K antigen, which can be removed by boiling the bacterial suspension at 100°C for 60 minutes. Colicin typing It is done for group D strains. Prevention and control As man is the major source of infection and the disease is transmitted by “food, fingers, faeces and flies” from person to person, adequate sanitation together with detection and treatment of patients and carriers must be undertaken to control the infection.. **** PASS WORD:shigella