* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download KNEE JOINT
Survey
Document related concepts
Transcript
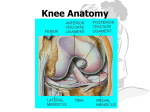
KNEE JOINT LEARNING OBJECTIVES CLASSIFICATION • Formed between lower end of femur, the upper end of tibia and the posterior surface of patella. • Gliding Synovial: Between anterior surface of lower end of femur and posterior surface of patella • Hinge synovial joint: Between inferior surface of condyles of femur and superior surface of condyles of tibia is ARTICULAR SURFACES • BONES: the femur, tibia, and patella. • ARTICULAR SURFACES: The condyles of the femur AND tibia, and the facets of the patella. • Corresponding tibial and femur condyles articulate • Articular surfaces of tibia are called medial and lateral tibial plateau • Separated from each other by a narrow, nonarticular area, widened as anterior and posterior intercondylar areas LIGAMENTS • • • Fibrous capsule Ligamentum patellae Tibial/ medial colletral ligament • • • • • • • • Fibular/ Lateral collateral ligament Oblique popliteal ligament Arcuate popliteal ligament Anterior cruciate ligament Posterior cruciate ligament Medial meniscus Lateral meniscus Transverse ligament ARTICULAR (fibrous) CAPSULE • Strong, local thickenings form ligaments. • Superiorly: Attached to the femur, just proximal to the articular margins of the condyles • Inferiorly: Attached to the articular margin of the tibia. • Posteriorly: Attached to the Intercondylar line • Laterally: Deficient on the lateral condyle, allowing the tendon of the popliteus muscle to pass • Inferolaterally: prolonged over the popliteus to form the arcuate popliteal ligament ARTICULAR CAPSULE Strengthened by five intrinsic ligaments; • • • • • Patellar ligament Fibular collateral ligament Tibial collateral ligament Oblique popliteal ligament Arcuate popliteal ligament SYNOVIAL MEMBRANE • Largest and most extensive in the body. • Commences at the upper border of the patella • Forms a large cul-de-sac beneath the Quadriceps femoris in front of the lower end of femur • Communicates with a bursa interposed between the tendon and the front of the femur. • The pouch is supported, during the movements of the knee, by the Articularis genu PATELLAR LIGAMENT • Continuation of the tendon of the quadriceps femoris muscle. • The patella is a sesamoid bone in this tendon. • Patella is most easily felt when the leg is extended. • The infrapatellar fatpad: – seperates the superior part of the deep surface of patella from the synovial membrane of the knee joint. • The deep infrapatellar bursa: – separates the inferior part of the patellar ligament from the anterior surface of the tibia. TIBIAL COLLATERAL LIGAMENT (medial ligament) • • A thickening of the fibrous capsule of the knee joint 8-9 cm long • Origin: • Insertion: – medial epicondyle of the femur – medial condyle and superio-medial surface of the tibia • Partly continuous with the tendon of the adductor magnus muscle. • The deep fibers are firmly attached to the medial meniscus and the fibrous capsule of the knee. FIBULAR COLLATERAL LIGAMENT • Round cord of 5cm • Origin: – lateral epicondyle of the femur • Insertion: – lateral surface of the head of the fibula. • The tendon of the popliteus muscle passes deep to the fibular collateral ligament • Separates it from the lateral meniscus. OBLIQUE POPLITEAL LIGAMENT • An expansion of the tendon of the semimembranosus muscle. • Strengthens the fibrous capsule of the knee joint posteriorly. • Origin: – Posterior to the medial epicondyle of the tibia • Insertion: – passes superolaterally and attaches to the posterior aspect of the fibrous capsule of the knee joint ARCUATE POPLITEAL LIGAMENT • Y-shaped • Strengthens the fibrous capsule Posteriorly. • Origin: – The stem arises from the posterior aspect of the head of the fibula. – Passes superomedially over the tendon of the popliteus muscle, and spreads out over the posterior surface of the knee joint. • Insertion: – Into the intercondylar area of the tibia and the posterior aspect of the lateral epicondyle of the femur. CRUCIATE LIGAMENTS • X shaped (cruciate). • Anterior and Posterior, according to their site of attachment to the tibia. • They are essential for the anteroposterior stability of the knee joint, especially when it is flexed • Within the capsule of the joint but are outside the synovial cavity. CRUCIATE LIGAMENTS • Join the femur and tibia • Located between the medial and lateral condyles • Separated from the joint cavity by the synovial membrane. • The synovial capsule lines the fibrous capsule. • Deficient posteriorly where it is reflected anteriorly around the cruciate ligaments. ANTERIOR CRUCIATE LIGAMENT • Weaker • Origin: – From the anterior part of the intercondylar area of the tibia, posterior to the medial meniscus. • It extends superiorly, posteriorly, and laterally • Insertion: – attach to the posterior part of the medial side of the lateral condyle of the femur. • Position of anterior cruciate ligament: – Knee flexed: slack – Knee extended: taut • Prevents POSTERIOR DISPLACEMENT of the femur on the tibia on hyperextension of the knee joint. • Prevents ANTERIOR DISPLACEMENT of tibia when the joint is flexed at a right angle POSTERIOR CRUCIATE LIGAMENT • Stronger • First structure observed when the knee joint is surgically opened posteriorly. • Origin: – From the posterior part of the intercondylar area of the tibia – passes superiorly and anteriorly on the medial side of the anterior cruciate ligament • Insertion: – attach to the anterior part of the lateral surface of the medial condyle of the femur. POSTERIOR CRUCIATE LIGAMENT • • • • • Tightens during flexion of the knee joint Prevents ANTERIOR DISPLACEMENT of the femur on the tibia And prevents POSTERIOR DISPLACEMENT of the tibia. Prevents hyperflexion of the knee joint. In the weight bearing flexed knee, it is the main stabilizing factor for the femur, e.g., when walking downhill or downstairs. • • • • • • • • • Lateral and medial (G. crescents) Slightly movable Fill the gaps between the femur and tibia during movements of the knee joint Act as shock absorbers. C-shaped (semilunar cartilages) Wedge-shaped in the transverse section. Firmly attached at their ends to the intercondylar area of the tibia. Present on the articular surface of the tibia and deepen it Articulate with the femoral condyles. MENISCI OF KNEE JOINT MENISCI OF KNEE JOINT SURFACES: • Superior surfaces are slightly concave for reception of condyles • Inferior surfaces that rest on the tibial condyles are flatter. MARGINS: • Thick at peripheral attached margins • Thin at internal unattached edges. MENISCI • • • • • The capsular fibers that attach the thick, convex margins of the menisci to the tibial condyles are called coronary ligaments. A slender fibrous band, called the transverse ligament of the knee, joins the anterior edges of the two menisci. This connection allows them to move together during movements of the femur on the tibia. The thick peripheral margins of the menisci are vascularised by genicular branches of the popliteal artery The unattached edges of the interior of the joint are avascular. MEDIAL MENISCUS • Cartilage is broader posteriorly than anteriorly. • Firmly attached to the deep surface of the tibial collateral ligament. The Anterior horn (L. cornu): • Attached ANTERIOR to the attachment of the anterior cruciate ligament at the anterior intercondylar area. The posterior horn: • Attached ANTERIOR to the attachment of the posterior cruciate ligament, at the to the posterior intercondylar area. LATERAL MENISCUS • • • • • Nearly circular and conforms to the lateral tibial condyle. Smaller More freely movable Covers a larger articular area than the medial meniscus The tendon of the popliteus muscle and bursa separate it from the fibular collateral ligaments. • The anterior and posterior horns are attached close together in the anterior and posterior intercondylar areas. • A strong tendinous slip, called the posterior meniscofemoral ligament, joins the lateral meniscus to the posterior cruciate ligament and the medial femoral condyle. BURSAE COMMUNICATING KNEE JOINT • Bursae reduce friction during movement between the bones and tendons • Four bursa communicate with the synovial cavity of the knee joint: – deep to the tendons of the quadriceps femoris – the popliteus – the medial head of the gastrocnemius muscle. BURSAE AROUND KNEE SUPRAPATELLAR (QUADRICEPS) BURSA • Large saccular extension of the synovial capsule • Passes superiorly between the femur and the tendon of the quadriceps femoris muscle. • Allows free movement of the quadriceps tendon over the distal end of the femur • Facilitates full extension and flexion of the knee joint. • The bursa is held in position by the part of the vastus intermedius muscle called the articularis genu muscle. PREPATELLAR BURSA • Between the skin and the anterior surface of the patella. • Allows free movement of the skin over the patella during flexion and extension of the leg. • May become inflamed after prolonged periods of weight bearing on the hands and knees. • Inflammation of this is "housemaid's knee" SUBCUTANEOUS INFRAPATELLAR BURSA • Located between the skin and the tibial tuberosity. • Allows the skin to glide over the tibial tuberosity and withstand pressure when kneeling with the trunk upright (e.g., when one kneels or genuflects during praying). • Inflammation of this bursa is "clergyman's knee" BLOOD SUPPLY • • • Supplied by the anastomoses around it: Five genicular branches of the popliteal artery Descending genicular branch of the femoral artery Descending branch of the lateral circumflex femoral artery Two recurrent branches of the anterior tibial artery Circumflex fibular branch of the posterior tibial artery NERVE SUPPLY • Femoral nerve, through its branches to the vasti. • Sciatic nerve, through its genicular branches of the tibial and common peroneal nerves. • Obturator nerve, through its posterior division.